Ann Surg Treat Res.
2021 Sep;101(3):167-180. 10.4174/astr.2021.101.3.167.
Meta-analysis of transanal versus laparoscopic total mesorectal excision for rectal cancer: a ‘New Health Technology’ assessment in South Korea
- Affiliations
-
- 1Division for New Health Technology Assessment, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
- 2TaTME Assessment Committee, National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
- 3Division of Colorectal Surgery, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 4Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 5Division of Colon and Rectal Surgery, Department of Surgery, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 6Department of General Surgery, Ewha Womans University College of Medicine, Seoul, Korea
- 7Department of Preventive Medicine, School of Medicine, Kyungpook National University, Daegu, Korea
- 8Department of Internal Medicine, Hanyang University Guri Hospital, Guri, Korea
- 9Department of Surgery, Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2519847
- DOI: http://doi.org/10.4174/astr.2021.101.3.167
Abstract
- Purpose
Under the South Korea’s unique health insurance structure, any new surgical technology must be evaluated first by the government in order to consider whether that particular technology can be applied to patients for further clinical trials as categorized as ‘New Health Technology,’ then potentially covered by the insurance sometime later. The aim of this meta-analysis was to assess the safety and efficacy of transanal total mesorectal excision (TaTME) for rectal cancer, activated by the National Evidence-based Healthcare Collaborating Agency (NECA) TaTME committee.
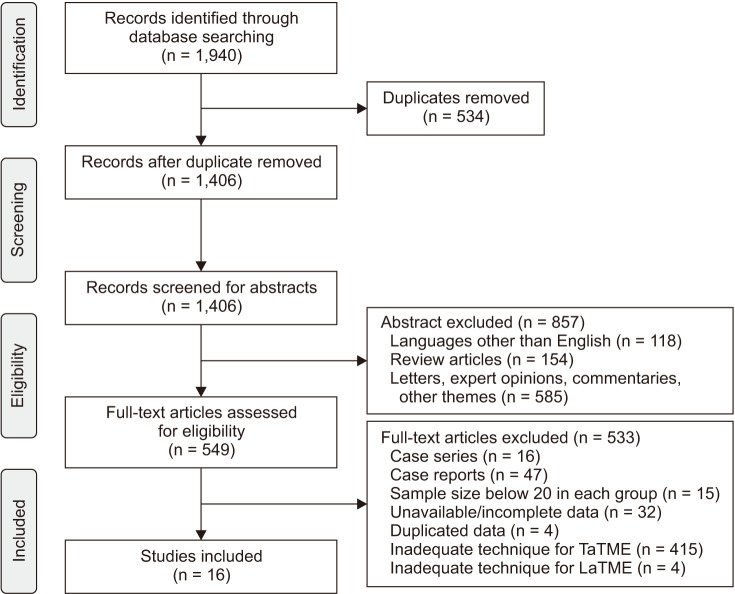
Methods
We systematically searched Ovid-MEDLINE, Ovid-Embase, Cochrane, and Korean databases (from their inception until August 31, 2019) for studies published that compare TaTME with laparoscopic total mesorectal excision (LaTME). End-points included perioperative and pathological outcomes.
Results
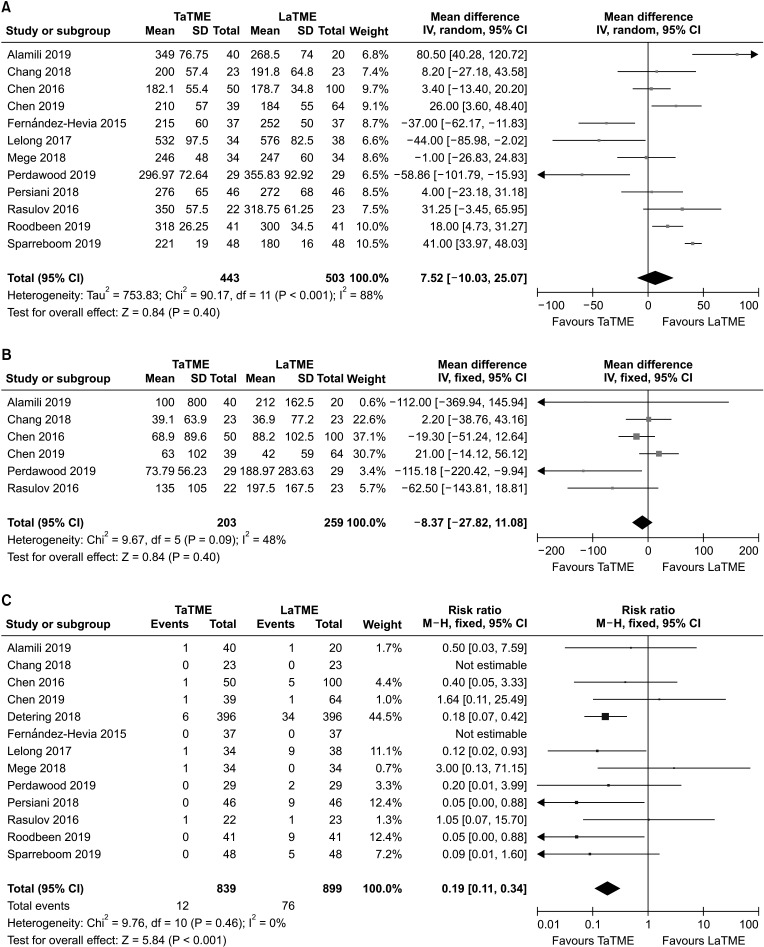
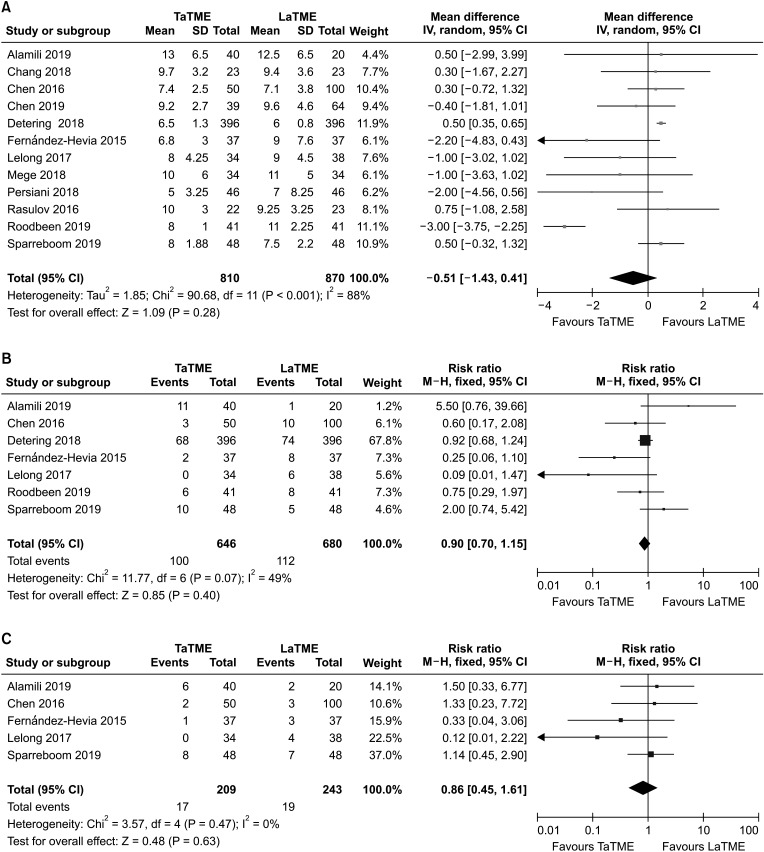
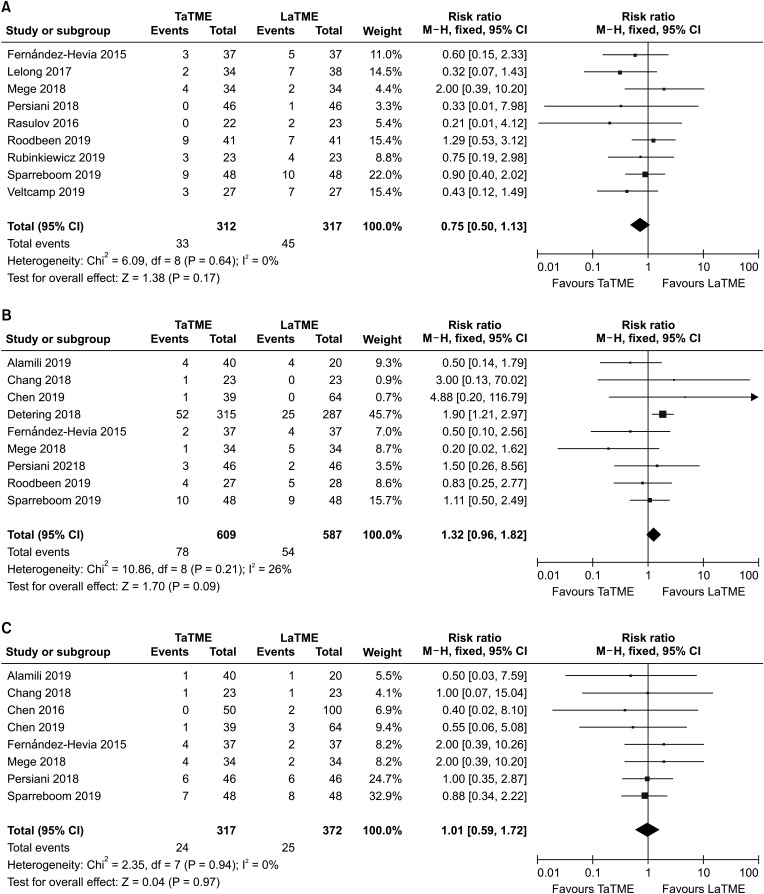
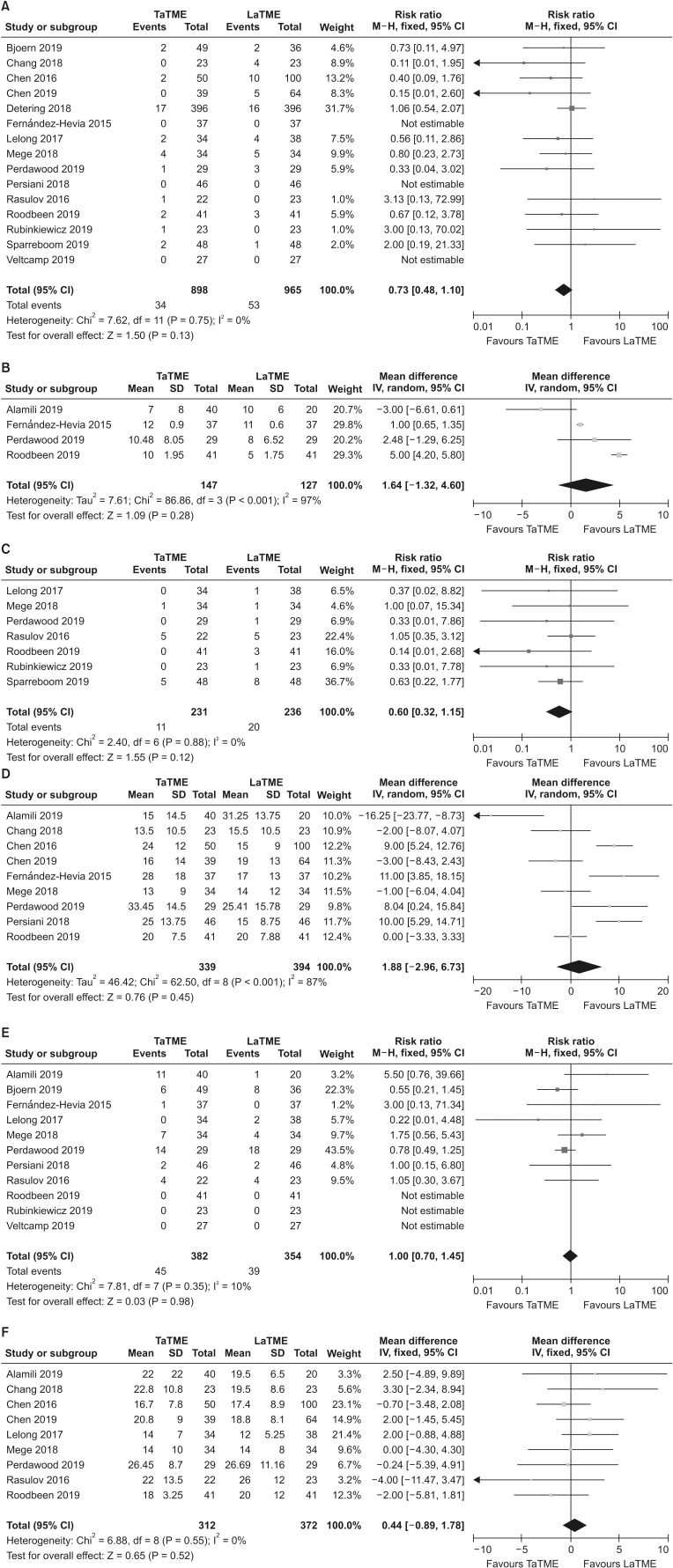
Sixteen cohort studies (7 for case-matched studies) were identified, comprising 1,923 patients (938 TaTMEs and 985 LaTMEs). Regarding perioperative outcomes, the conversion rate was significantly lower in TaTME (risk ratio, 0.19; 95% confidence interval, 0.11–0.34; P < 0.001); whereas other perioperative outcomes were similar to LaTME. There were no statistically significant differences in pathological results between the 2 procedures.
Conclusion
Our meta-analysis showed comparable results in preoperative and pathologic outcomes between TaTME and LaTME, and indicated the benefit of TaTME with low conversion. Extensive evaluations of well-designed, multicenter randomized controlled trials are required to come to unequivocal conclusions, but the results showed that TaTME is a potentially beneficial technique in some specific cases. This meta-analysis suggests that TaTME can be performed for rectal cancer patients as a ‘New Health Technology’ endorsed by NECA in South Korea.
Keyword
Figure
Reference
-
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424. PMID: 30207593.
Article2. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery-the clue to pelvic recurrence? Br J Surg. 1982; 69:613–616. PMID: 6751457.
Article3. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998; 133:894–899. PMID: 9711965.4. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484. PMID: 15992696.5. Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005; 365:1718–1726. PMID: 15894098.
Article6. Penninckx F, Kartheuser A, Van de Stadt J, Pattyn P, Mansvelt B, Bertrand C, et al. Outcome following laparoscopic and open total mesorectal excision for rectal cancer. Br J Surg. 2013; 100:1368–1375. PMID: 23939849.
Article7. Lujan J, Valero G, Hernandez Q, Sanchez A, Frutos MD, Parrilla P. Randomized clinical trial comparing laparoscopic and open surgery in patients with rectal cancer. Br J Surg. 2009; 96:982–989. PMID: 19644973.
Article8. Mizrahi I, Sands DR. Transanal total mesorectal excision for rectal cancer: a review. Ann Laparosc Endosc Surg. 2017; 2:144.
Article9. Sylla P, Rattner DW, Delgado S, Lacy AM. NOTES transanal rectal cancer resection using transanal endoscopic microsurgery and laparoscopic assistance. Surg Endosc. 2010; 24:1205–1210. PMID: 20186432.
Article10. Penna M, Hompes R, Arnold S, Wynn G, Austin R, Warusavitarne J, et al. Transanal total mesorectal excision: international registry results of the first 720 cases. Ann Surg. 2017; 266:111–117. PMID: 27735827.11. de Lacy FB, van Laarhoven JJ, Pena R, Arroyave MC, Bravo R, Cuatrecasas M, et al. Transanal total mesorectal excision: pathological results of 186 patients with mid and low rectal cancer. Surg Endosc. 2018; 32:2442–2447. PMID: 29101570.
Article12. Abbott SC, Stevenson AR, Bell SW, Clark D, Merrie A, Hayes J, et al. An assessment of an Australasian pathway for the introduction of transanal total mesorectal excision (taTME). Colorectal Dis. 2018; 20:O1–O6. PMID: 29165862.
Article13. 2017 European Society of Coloproctology (ESCP) collaborating group. An international multicentre prospective audit of elective rectal cancer surgery; operative approach versus outcome, including transanal total mesorectal excision (TaTME). Colorectal Dis. 2018; 20 Suppl 6:33–46. PMID: 30255642.14. Wasmuth HH, Faerden AE, Myklebust TÅ, Pfeffer F, Norderval S, Riis R, et al. Transanal total mesorectal excision for rectal cancer has been suspended in Norway. Br J Surg. 2020; 107:121–130. PMID: 31802481.
Article15. Sylla P, Knol JJ, D'Andrea AP, Perez RO, Atallah SB, Penna M, et al. Urethral injury and other urologic injuries during transanal total mesorectal excision: an international collaborative study. Ann Surg. 2021; 274:e115–e125. PMID: 31567502.16. Caycedo-Marulanda A, Verschoor CP. Experience beyond the learning curve of transanal total mesorectal excision (taTME) and its effect on the incidence of anastomotic leak. Tech Coloproctol. 2020; 24:309–316. PMID: 32112245.
Article17. Persiani R, Agnes A, Belia F, D'Ugo D, Biondi A. The learning curve of TaTME for mid-low rectal cancer: a comprehensive analysis from a five-year institutional experience. Surg Endosc. 2020; 10. 26. [Epub]. DOI: 10.1007/s00464-020-08115-0.
Article18. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare inter vent ions: expl anat ion and elaboration. BMJ. 2009; 339:b2700. PMID: 19622552.19. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; 25:603–605. PMID: 20652370.
Article20. Quirke P, Steele R, Monson J, Grieve R, Khanna S, Couture J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet. 2009; 373:821–828. PMID: 19269520.
Article21. Efthimiou O. Practical guide to the meta-analysis of rare events. Evid Based Ment Health. 2018; 21:72–76. PMID: 29650528.
Article22. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005; 5:13. PMID: 15840177.
Article23. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003; 327:557–560. PMID: 12958120.
Article24. Fernández-Hevia M, Delgado S, Castells A, Tasende M, Momblan D, Díaz del Gobbo G, et al. Transanal total mesorectal excision in rectal cancer: short-term outcomes in comparison with laparoscopic surgery. Ann Surg. 2015; 261:221–227. PMID: 25185463.25. Chen CC, Lai YL, Jiang JK, Chu CH, Huang IP, Chen WS, et al. Transanal total mesorectal excision versus laparoscopic surgery for rectal cancer receiving neoadjuvant chemoradiation: a matched case-control study. Ann Surg Oncol. 2016; 23:1169–1176. PMID: 26597369.
Article26. Rasulov AO, Mamedli ZZ, Gordeyev SS, Kozlov NA, Dzhumabaev HE. Short-term outcomes after transanal and laparoscopic total mesorectal excision for rectal cancer. Tech Coloproctol. 2016; 20:227–234. PMID: 26794213.
Article27. Lelong B, Meillat H, Zemmour C, Poizat F, Ewald J, Mege D, et al. Short- and mid-term outcomes after endoscopic transanal or laparoscopic transabdominal total mesorectal excision for low rectal cancer: a single institutional case-control study. J Am Coll Surg. 2017; 224:917–925. PMID: 28024946.
Article28. Chang TC, Kiu KT. Transanal total mesorectal excision in lower rectal cancer: comparison of short-term outcomes with conventional laparoscopic total mesorectal excision. J Laparoendosc Adv Surg Tech A. 2018; 28:365–369. PMID: 29190178.
Article29. Detering R, Roodbeen SX, van Oostendorp SE, Dekker JT, Sietses C, Bemelman WA, et al. Three-year nationwide experience with transanal total mesorectal excision for rectal cancer in the Netherlands: a propensity score-matched comparison with conventional laparoscopic total mesorectal excision. J Am Coll Surg. 2019; 228:235–244. PMID: 30639298.
Article30. Mege D, Hain E, Lakkis Z, Maggiori L, Prost À, Panis Y. Is trans-anal total mesorectal excision really safe and better than laparoscopic total mesorectal excision with a perineal approach first in patients with low rectal cancer?: a learning curve with case-matched study in 68 patients. Colorectal Dis. 2018; 20:O143–O151. PMID: 29693307.
Article31. Persiani R, Biondi A, Pennestrì F, Fico V, De Simone V, Tirelli F, et al. Transanal total mesorectal excision vs laparoscopic total mesorectal excision in the treatment of low and middle rectal cancer: a propensity score matching analysis. Dis Colon Rectum. 2018; 61:809–816. PMID: 29771810.
Article32. Alamili M, Levic K, Kanstrup K, Bisgaard T, Bulut O. Inflammatory response after transanal total mesorectal excision. Dan Med J. 2019; 66:A5555. PMID: 31256779.33. Bjoern MX, Nielsen S, Perdawood SK. Quality of life after surgery for rectal cancer: a comparison of functional outcomes after transanal and laparoscopic approaches. J Gastrointest Surg. 2019; 23:1623–1630. PMID: 30603861.
Article34. Chen YT, Kiu KT, Yen MH, Chang TC. Comparison of the short-term outcomes in lower rectal cancer using three different surgical techniques: transanal total mesorectal excision (TME), laparoscopic TME, and open TME. Asian J Surg. 2019; 42:674–680. PMID: 30318319.
Article35. Perdawood SK, Warnecke M, Bjoern MX, Eiholm S. The pattern of defects in mesorectal specimens: is there a difference between transanal and laparoscopic approaches? Scand J Surg. 2019; 108:49–54. PMID: 29966503.
Article36. Roodbeen SX, Penna M, Mackenzie H, Kusters M, Slater A, Jones OM, et al. Transanal total mesorectal excision (TaTME) versus laparoscopic TME for MRI-defined low rectal cancer: a propensity score-matched analysis of oncological outcomes. Surg Endosc. 2019; 33:2459–2467. PMID: 30350103.
Article37. Rubinkiewicz M, Zarzycki P, Witowski J, Pisarska M, Gajewska N, Torbicz G, et al. Functional outcomes after resections for low rectal tumors: comparison of transanal with laparoscopic total mesorectal excision. BMC Surg. 2019; 19:79. PMID: 31277628.
Article38. Sparreboom CL, Komen N, Rizopoulos D, van Westreenen HL, Doornebosch PG, Dekker JW, et al. Transanal total mesorectal excision: how are we doing so far? Colorectal Dis. 2019; 21:767–774. PMID: 30844130.
Article39. Veltcamp Helbach M, Koedam TW, Knol JJ, Velthuis S, Bonjer HJ, Tuynman JB, et al. Quality of life after rectal cancer surgery: differences between laparoscopic and transanal total mesorectal excision. Surg Endosc. 2019; 33:79–87. PMID: 29967994.
Article40. Thorpe H, Jayne DG, Guillou PJ, Quirke P, Copeland J, Brown JM, et al. Patient factors influencing conversion from laparoscopical ly assisted to open surgery for colorectal cancer. Br J Surg. 2008; 95:199–205. PMID: 17696215.41. Pandya S, Murray JJ, Coller JA, Rusin LC. Laparoscopic colectomy: indications for conversion to laparotomy. Arch Surg. 1999; 134:471–475. PMID: 10323418.42. Pikarsky AJ, Saida Y, Yamaguchi T, Martinez S, Chen W, Weiss EG, et al. Is obesity a high-risk factor for laparoscopic colorectal surgery? Surg Endosc. 2002; 16:855–858. PMID: 11997837.
Article43. Veldkamp R, Gholghesaei M, Bonjer HJ, Meijer DW, Buunen M, Jeekel J, et al. Laparoscopic resection of colon cancer: consensus of the European Association of Endoscopic Surgery (EAES). Surg Endosc. 2004; 18:1163–1185. PMID: 15457376.
Article44. Rouanet P, Mourregot A, Azar CC, Carrere S, Gutowski M, Quenet F, et al. Transanal endoscopic proctectomy: an innovative procedure for difficult resection of rectal tumors in men with narrow pelvis. Dis Colon Rectum. 2013; 56:408–415. PMID: 23478607.45. Di Candido F, Carvello M, Keller DS, Vanni E, Maroli A, Montroni I, et al. A comparative cost analysis of transanal and laparoscopic total mesorectal excision for rectal cancer. Updates Surg. 2021; 73:85–91. PMID: 32929690.
Article46. Krarup PM, Jorgensen LN, Andreasen AH, Harling H. Danish Colorectal Cancer Group. A nationwide study on anastomotic leakage after colonic cancer surgery. Colorectal Dis. 2012; 14:e661–e667. PMID: 22564292.
Article47. Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. 2010; 251:807–818. PMID: 20395841.
Article48. Larsen SG, Pfeffer F, Kørner H. Norwegian Colorectal Cancer Group. Norwegian moratorium on transanal total mesorectal excision. Br J Surg. 2019; 106:1120–1121. PMID: 31304578.
Article49. Gachabayov M, Bergamaschi R. Is taTME delivering? Updates Surg. 2019; 71:13–15. PMID: 30796631.
Article50. Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH, et al. Pathology Review Committee. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002; 26:350–357. PMID: 11859207.51. Lin HH, Lin JK, Lin CC, Lan YT, Wang HS, Yang SH, et al. Circumferential margin plays an independent impact on the outcome of rectal cancer patients receiving curative total mesorectal excision. Am J Surg. 2013; 206:771–777. PMID: 23871321.
Article52. McGrath S, Zhao X, Steele R, Thombs BD, Benedetti A. DEPRESsion Screening Data (DEPRESSD) Collaboration. Estimating the sample mean and standard deviation from commonly reported quantiles in meta-analysis. Stat Methods Med Res. 2020; 1. 30. [Epub]. DOI: 10.1177/0962280219889080.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Surgical Techniques for Transanal Local Excision for Early Rectal Cancer
- Short- and mid-term outcomes of transanal versus laparoscopic total mesorectal excision for low rectal cancer: a meta-analysis
- Transanal total mesorectal excision for rectal cancer: it’s come a long way and here to stay
- Transanal Total Mesorectal Excision for Rectal Cancer: Perioperative and Oncological Outcomes
- Robotic Total Mesorectal Excision for Rectal Cancer: Current Evidences and Future Perspectives