Ann Surg Treat Res.
2021 Aug;101(2):85-92. 10.4174/astr.2021.101.2.85.
Clinical impact of the treatment modality on small, solitary, recurrent intrahepatic hepatocellular carcinomas after primary liver resection
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery, Chonnam National University Medical School, Gwangju, Korea
- 3Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2519001
- DOI: http://doi.org/10.4174/astr.2021.101.2.85
Abstract
- Purpose
The aim of this study was to determine the survival benefit based on different treatment strategies in patients with small, solitary, recurring intrahepatic hepatocellular carcinomas (HCCs) that were defined as recurred Barcelona Clinic Liver Cancer stage O (reBCLC-O).
Methods
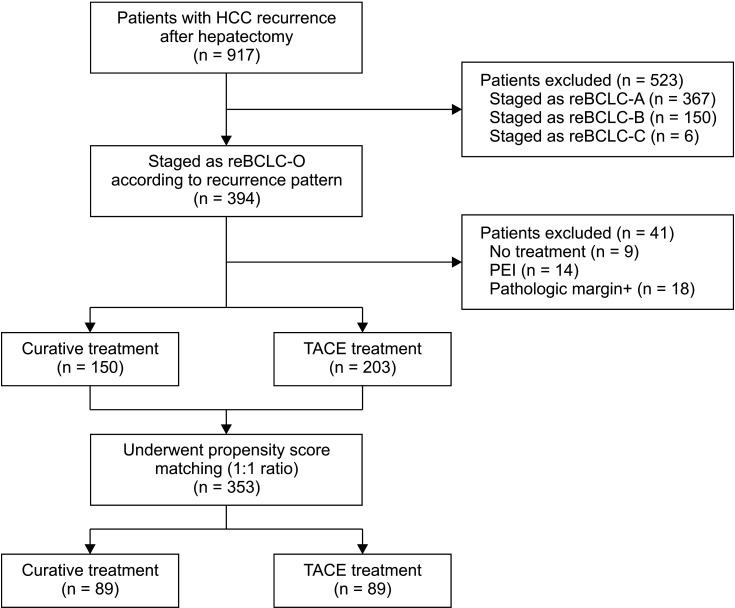
Among the 917 patients with HCC recurrence after primary hepatic resection, 394 patients with reBCLC-O were selected. Of these, 150 patients underwent curative treatment (re-resection, radiofrequency ablation, and liver transplantation) and 203 underwent transarterial chemoembolization (TACE) group for recurrent HCC. After propensity score matching (PSM), both the groups were well balanced (89 patients in each group).
Results
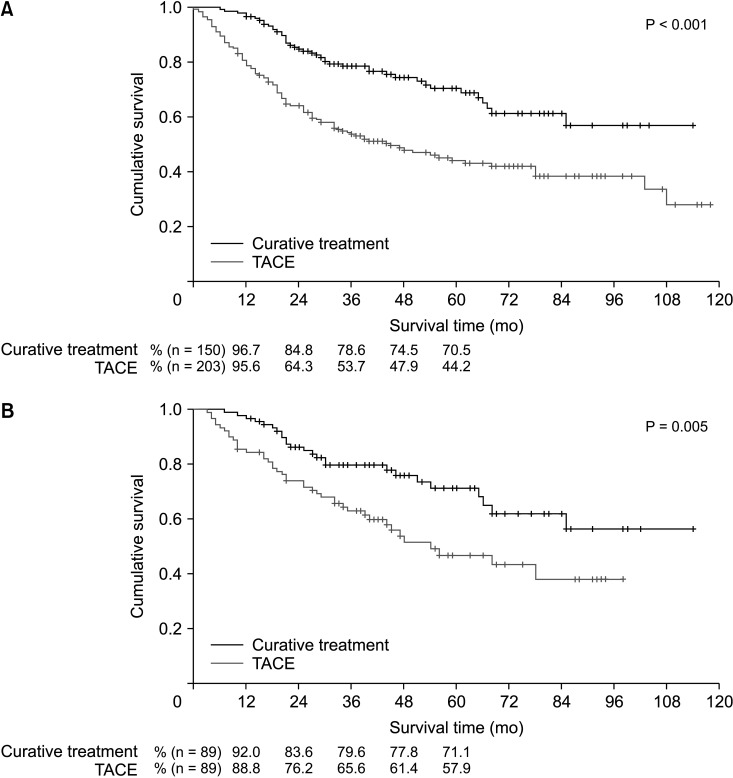
Before PSM, the 1-, 3-, and 5-year overall survival (OS) rates of patients in the curative treatment group (96.7%, 78.6%, and 70.5%, respectively) were significantly better than those in the TACE treatment group (95.6%, 53.7%, and 44.2%, respectively) (P < 0.001). After PSM, the 1-, 3-, and 5-year OS rates also differed significantly (92.0%, 79.6%, and 71.1% in the curative treatment group vs. 88.8%, 65.6%, and 57.9% in the TACE group) (P = 0.005). The independent predictors of worse OS were tumor number at the time of resection and treatment modality for the recurrence, time interval to recurrence, and prothrombin time international normalized ratio and alpha-fetoprotein levels at the time of recurrence.
Conclusion
The OS of patients in the curative treatment group was better than that in the non-curative treatment group after PSM. Based on our results, curative treatment should be strongly recommended in the patients with reBCLC-O recurrence for better survival.
Figure
Reference
-
1. Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015; 136:E359–E386. PMID: 25220842.
Article2. Marrero JA, Kulik LM, Sirlin CB, Zhu AX, Finn RS, Abecassis MM, et al. Diagnosis, staging, and management of hepatocellular carcinoma: 2018 practice guidance by the American Association for the Study of Liver Diseases. Hepatology. 2018; 68:723–750. PMID: 29624699.
Article3. Pawlik TM, Poon RT, Abdalla EK, Zorzi D, Ikai I, Curley SA, et al. Critical appraisal of the clinical and pathologic predictors of survival after resection of large hepatocellular carcinoma. Arch Surg. 2005; 140:450–457. PMID: 15897440.
Article4. Poon RT, Fan ST. Hepatectomy for hepatocellular carcinoma: patient selection and postoperative outcome. Liver Transpl. 2004; 10(2 Suppl 1):S39–S45.
Article5. Bismuth H, Chiche L, Adam R, Castaing D, Diamond T, Dennison A. Liver resection versus transplantation for hepatocellular carcinoma in cirrhotic patients. Ann Surg. 1993; 218:145–151. PMID: 8393649.
Article6. Cha C, Fong Y, Jarnagin WR, Blumgart LH, DeMatteo RP. Predictors and patterns of recurrence after resection of hepatocellular carcinoma. J Am Coll Surg. 2003; 197:753–758. PMID: 14585409.
Article7. Cha CH, Ruo L, Fong Y, Jarnagin WR, Shia J, Blumgart LH, et al. Resection of hepatocellular carcinoma in patients otherwise eligible for transplantation. Ann Surg. 2003; 238:315–321. PMID: 14501497.
Article8. Lu X, Zhao H, Yang H, Mao Y, Sang X, Miao R, et al. A prospective clinical study on early recurrence of hepatocellular carcinoma after hepatectomy. J Surg Oncol. 2009; 100:488–493. PMID: 19653238.
Article9. Rahbari NN, Mehrabi A, Mollberg NM, Müller SA, Koch M, Büchler MW, et al. Hepatocellular carcinoma: current management and perspectives for the future. Ann Surg. 2011; 253:453–469. PMID: 21263310.10. Arnaoutakis DJ, Mavros MN, Shen F, Alexandrescu S, Firoozmand A, Popescu I, et al. Recurrence patterns and prognostic factors in patients with hepatocellular carcinoma in noncirrhotic liver: a multi-institutional analysis. Ann Surg Oncol. 2014; 21:147–154. PMID: 23959056.
Article11. Hirokawa F, Hayashi M, Asakuma M, Shimizu T, Inoue Y, Uchiyama K. Risk factors and patterns of early recurrence after curative hepatectomy for hepatocellular carcinoma. Surg Oncol. 2016; 25:24–29. PMID: 26979637.
Article12. Tung-Ping Poon R, Fan ST, Wong J. Risk factors, prevention, and management of postoperative recurrence after resection of hepatocellular carcinoma. Ann Surg. 2000; 232:10–24. PMID: 10862190.
Article13. Korean Association for the Study of the Liver (KASL). KASL clinical practice guidelines for liver cirrhosis: ascites and related complications. Clin Mol Hepatol. 2018; 24:230–277. PMID: 29991196.14. European Association for the Study of the Liver. Electronic address: easloffice@easloffice.eu. European Association for the Study of the Liver. EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018; 69:182–236. PMID: 29628281.15. Arima K, Nitta H, Beppu T, Nakagawa S, Okabe H, Imai K, et al. Impact of repeated hepatectomy on liver regeneration in hepatocellular carcinoma: a propensity score-based analysis. Anticancer Res. 2019; 39:965–970. PMID: 30711982.
Article16. Ochiai T, Inoue H, Watanabe N, Ito H, Toma A, Morimura R, et al. Outcome of a second hepatectomy in octogenarians with hepatocellular carcinoma recurrence: single centre's experience. ANZ J Surg. 2019; 89:1270–1274. PMID: 31280497.
Article17. Ho CM, Lee PH, Shau WY, Ho MC, Wu YM, Hu RH. Survival in patients with recurrent hepatocellular carcinoma after primary hepatectomy: comparative effectiveness of treatment modalities. Surgery. 2012; 151:700–709. PMID: 22284764.
Article18. Ferrer-Fàbrega J, Forner A, Liccioni A, Miquel R, Molina V, Navasa M, et al. Prospective validation of ab initio liver transplantation in hepatocellular carcinoma upon detection of risk factors for recurrence after resection. Hepatology. 2016; 63:839–849. PMID: 26567038.19. Zhang X, Li C, Wen T, Peng W, Yan L, Yang J. Treatment for intrahepatic recurrence after curative resection of hepatocellular carcinoma: salvage liver transplantation or re-resection/radiofrequency ablation? A Retrospective Cohort Study. Int J Surg. 2017; 46:178–185. PMID: 28890407.
Article20. Xia Y, Li J, Liu G, Wang K, Qian G, Lu Z, et al. Long-term effects of repeat hepatectomy vs percut aneous radiof requency ablation among patients with recurrent hepatocellular carcinoma: a randomized clinical trial. JAMA Oncol. 2020; 6:255–263. PMID: 31774468.21. Feng Y, Wu H, Huang DQ, Xu C, Zheng H, Maeda M, et al. Radiofrequency ablation versus repeat resection for recurrent hepatocellular carcinoma (≤ 5 cm) after initial curative resection. Eur Radiol. 2020; 30:6357–6368. PMID: 32529568.
Article22. Lu LH, Mei J, Kan A, Ling YH, Li SH, Wei W, et al. Treatment optimization for recurrent hepatocellular carcinoma: repeat hepatic resection versus radiofrequency ablation. Cancer Med. 2020; 9:2997–3005. PMID: 32108433.
Article23. Poon RT, Fan ST, Lo CM, Liu CL, Wong J. Intrahepatic recurrence after curative resection of hepatocellular carcinoma: long-term results of treatment and prognostic factors. Ann Surg. 1999; 229:216–222. PMID: 10024103.24. Shimada M, Takenaka K, Gion T, Fujiwara Y, Kajiyama K, Maeda T, et al. Prognosis of recurrent hepatocellular carcinoma: a 10-year surgical experience in Japan. Gastroenterology. 1996; 111:720–726. PMID: 8780578.
Article25. Shah SA, Greig PD, Gallinger S, Cattral MS, Dixon E, Kim RD, et al. Factors associated with early recurrence after resection for hepatocellular carcinoma and outcomes. J Am Coll Surg. 2006; 202:275–283. PMID: 16427553.
Article26. Bruix J, Reig M, Sherman M. Evidence-based diagnosis, staging, and treatment of patients with hepatocellular carcinoma. Gastroenterology. 2016; 150:835–853. PMID: 26795574.
Article27. Shimoda M, Tago K, Shiraki T, Mori S, Kato M, Aoki T, et al. Risk factors for early recurrence of single lesion hepatocellular carcinoma after curative resection. World J Surg. 2016; 40:2466–2471. PMID: 27138886.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Appropriate treatment modality for solitary small hepatocellular carcinoma: Radiofrequency ablation vs. resection vs. transplantation?
- Complete Remission with Transarterial Chemoembolization in a Patient with Hepatocellular Carcinoma Who Showed Early Recurrence following Surgical Resection
- Results of Hepatectomy as First Treatment for Hepatocellular Carcinoma within the Milan Criteria with Preserved Liver Function
- A Case of Long Term Survival in Patient with Early Intrahepatic Recurrence and Extrahepatic Metastasis after Curative Resection of Hepatocellular Carcinoma
- Study of Genomic Heterogeneity of Hepatocellular Carcinomas by Using Arbitrary Primer Polymerase Chain Reaction (AP-PCR)