Cancer Res Treat.
2021 Jul;53(3):881-888. 10.4143/crt.2020.1008.
Safety, Efficacy, and Patient Satisfaction with Initial Peripherally Inserted Central Catheters Compared with Usual Intravenous Access in Terminally Ill Cancer Patients: A Randomized Phase II Study
- Affiliations
-
- 1Department of Family Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 2Division of Medical Oncology and Hematology, Department of Internal Medicine, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- 3Department of Neurology, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Uijeongbu, Korea
- 4Department of Radiology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Yangsan, Korea
- KMID: 2518412
- DOI: http://doi.org/10.4143/crt.2020.1008
Abstract
- Purpose
The purpose of this study was to investigate whether routine insertion of peripherally inserted central catheter (PICC) at admission to a hospice-palliative care (HPC) unit is acceptable in terms of safety and efficacy and whether it results in superior patient satisfaction compared to usual intravenous (IV) access.
Materials and Methods
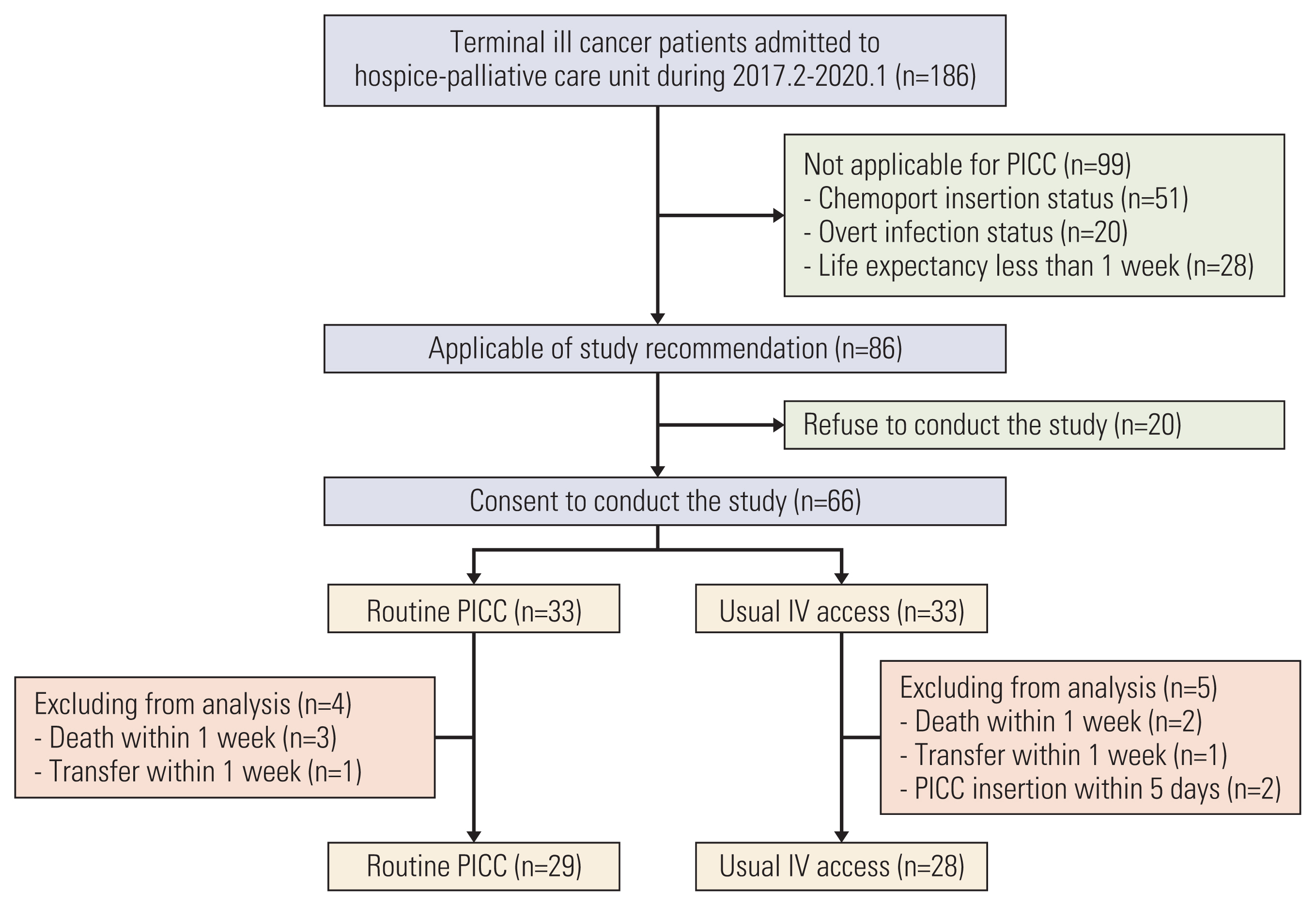
Terminally ill cancer patients were randomly assigned to two arms: routine PICC access and usual IV access arm. The primary endpoint was IV maintenance success rate, defined as the rate of functional IV maintenance until the intended time (discharge, transfer, or death).
Results
A total of 66 terminally ill cancer patients were enrolled and randomized to study arms. Among them, 57 patients (routine PICC, 29; usual IV, 28) were analyzed. In the routine PICC arm, mean time to PICC was 0.84 days (range, 0 to 3 days), 27 patients maintained PICC with function until the intended time. In the usual IV arm, 11 patients maintained peripheral IV access until the intended time, and 15 patients underwent PICC insertion. The IV maintenance success rate in the routine PICC arm (27/29, 93.1%) was similar to that in the usual IV arm (26/28, 92.8%, p=0.958). Patient satisfaction at day 5 was better in the routine PICC arm (97%, ‘a little comfort’ or ‘much comfort’) compared with the usual IV arm (21%) (p <0.001).
Conclusion
Routine PICC insertion in terminally ill cancer patients was comparable in safety and efficacy and resulted in superior satisfaction compared with usual IV access. Thus, routine PICC insertion could be considered at admission to the HPC unit.
Figure
Reference
-
References
1. Cleeland CS. Cancer-related symptoms. Semin Radiat Oncol. 2000; 10:175–90.
Article2. Walshe LJ, Malak SF, Eagan J, Sepkowitz KA. Complication rates among cancer patients with peripherally inserted central catheters. J Clin Oncol. 2002; 20:3276–81.
Article3. Ng PK, Ault MJ, Ellrodt AG, Maldonado L. Peripherally inserted central catheters in general medicine. Mayo Clin Proc. 1997; 72:225–33.
Article4. Lundh Hagelin C, Seiger A, Furst CJ. Quality of life in terminal care: with special reference to age, gender and marital status. Support Care Cancer. 2006; 14:320–8.5. Lee GJ, Ahn HS, Go SE, Kim JH, Seo MW, Kang SH, et al. Patient’s factors at entering hospice affecting length of survival in a hospice center. Cancer Res Treat. 2015; 47:1–8.
Article6. Llobera J, Esteva M, Rifa J, Benito E, Terrasa J, Rojas C, et al. Terminal cancer. duration and prediction of survival time. Eur J Cancer. 2000; 36:2036–43.7. Park K, Jun HJ, Oh SY. Safety, efficacy, and patient-perceived satisfaction of peripherally inserted central catheters in terminally ill cancer patients: a prospective multicenter observational study. Support Care Cancer. 2016; 24:4987–92.
Article8. Park K, Lim HG, Hong JY, Song H. Safety and efficacy of peripherally inserted central catheters in terminally Ill cancer patients: single institute experience. Korean J Hosp Palliat Care. 2014; 17:179–84.
Article9. Yamada R, Morita T, Yashiro E, Otani H, Amano K, Tei Y, et al. Patient-reported usefulness of peripherally inserted central venous catheters in terminally ill cancer patients. J Pain Symptom Manage. 2010; 40:60–6.
Article10. McGee DC, Gould MK. Preventing complications of central venous catheterization. N Engl J Med. 2003; 348:1123–33.
Article11. Gunst M, Matsushima K, Vanek S, Gunst R, Shafi S, Frankel H. Peripherally inserted central catheters may lower the incidence of catheter-related blood stream infections in patients in surgical intensive care units. Surg Infect (Larchmt). 2011; 12:279–82.
Article12. Cheong K, Perry D, Karapetis C, Koczwara B. High rate of complications associated with peripherally inserted central venous catheters in patients with solid tumours. Intern Med J. 2004; 34:234–8.
Article13. Yap YS, Karapetis C, Lerose S, Iyer S, Koczwara B. Reducing the risk of peripherally inserted central catheter line complications in the oncology setting. Eur J Cancer Care (Engl). 2006; 15:342–7.
Article14. Mermel LA. Prevention of intravascular catheter-related infections. Ann Intern Med. 2000; 132:391–402.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safety and Efficacy of Peripherally Inserted Central Catheters in Terminally Ill Cancer Patients: Single Institute Experience
- Safety and Effectiveness of Indwelling Percutaneous Drainage in Hospitalized Terminally Ill Cancer Patients with Recurrent Ascites
- Availability of peripheral inserted central catheters in severe hemophilia patients with inhibitors
- Early-onset Pericardial Effusion after Peripherally Inserted Central Venous Catheterization in a Preterm Infant
- Safety and Efficacy of Peripherally Inserted Central Catheter Placement by Surgical Intensivist–Led Vascular Access Team