J Korean Foot Ankle Soc.
2021 Jun;25(2):100-107. 10.14193/jkfas.2021.25.2.100.
The Current Status of Bacterial Identification by Wound Culture for Diabetic Foot Lesions in a Single Tertiary Hospital in South Korea
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Busan, Korea
- KMID: 2516648
- DOI: http://doi.org/10.14193/jkfas.2021.25.2.100
Abstract
- Purpose
The present study aimed to develop guidelines regarding initial choice of antibiotics for diabetic foot ulcers (DFU) by investigating bacterial isolates.
Materials and Methods
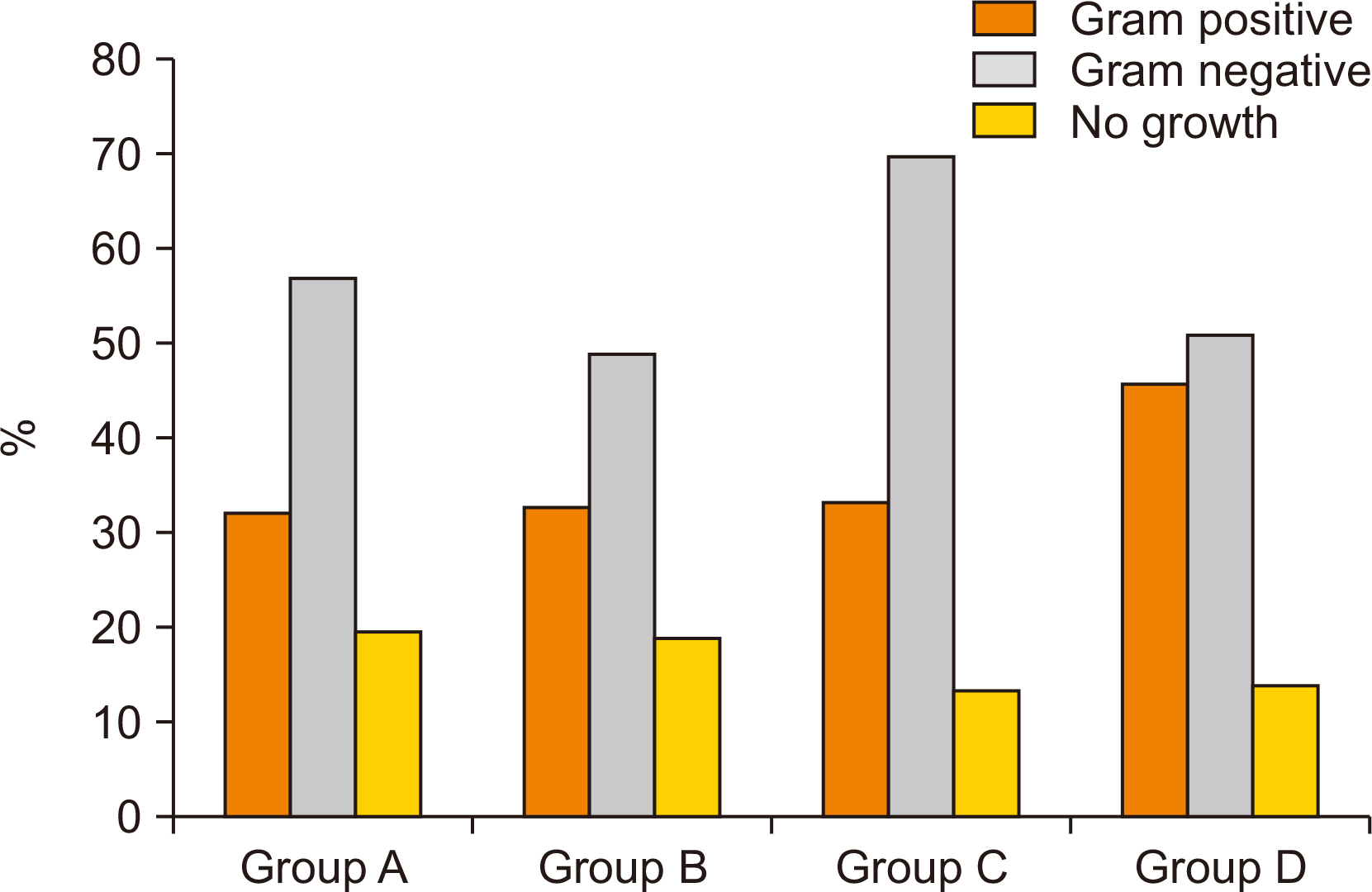
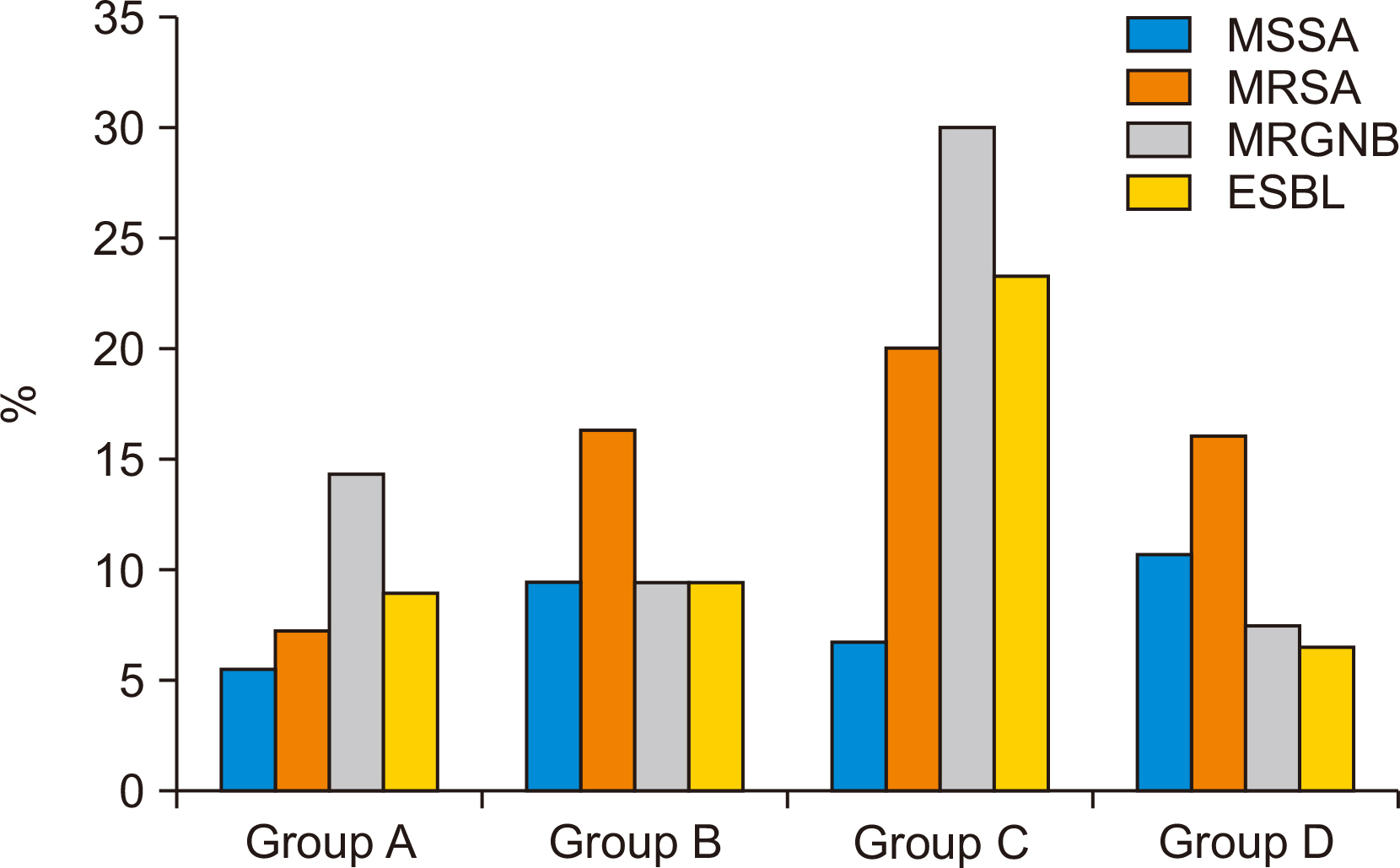
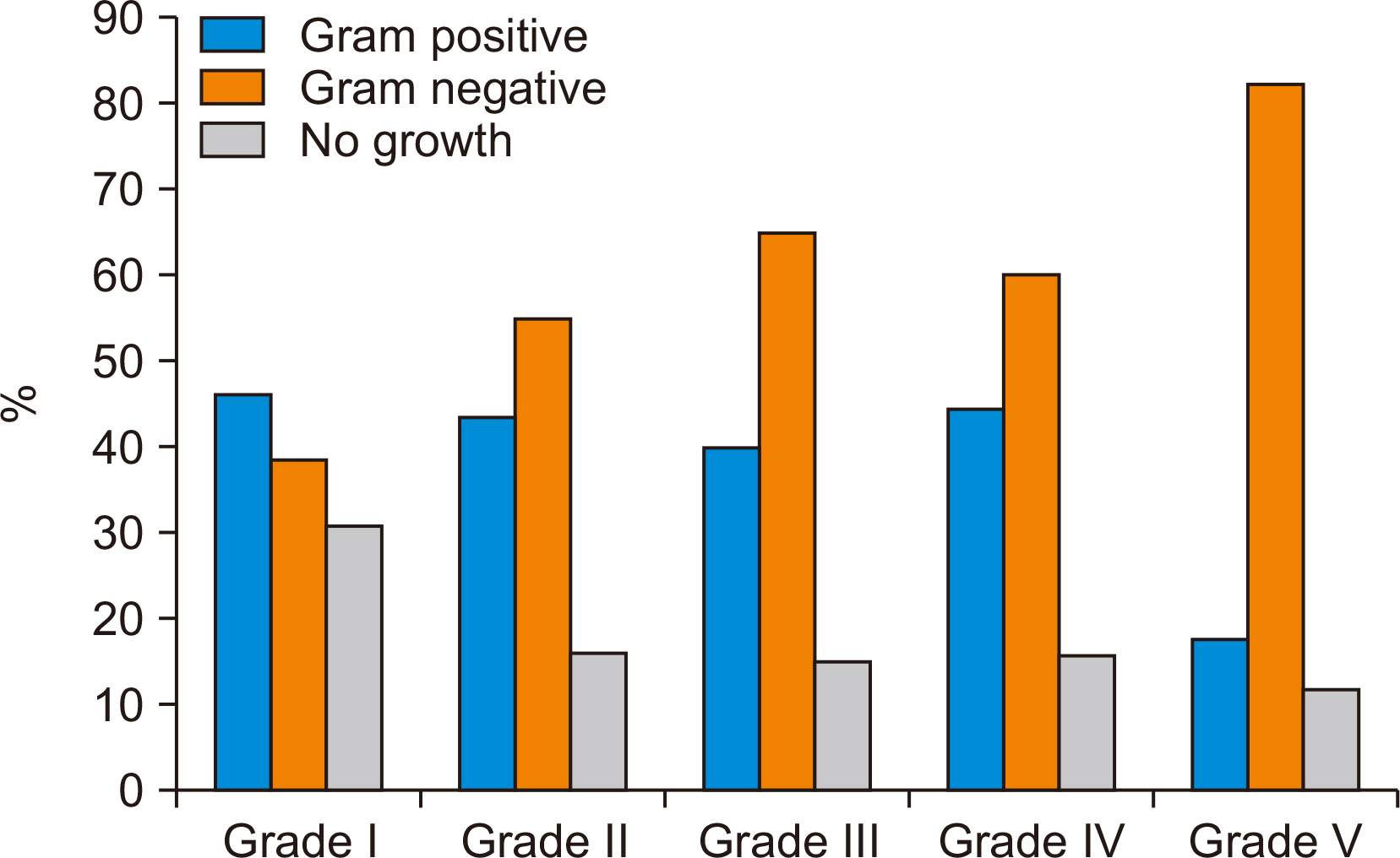
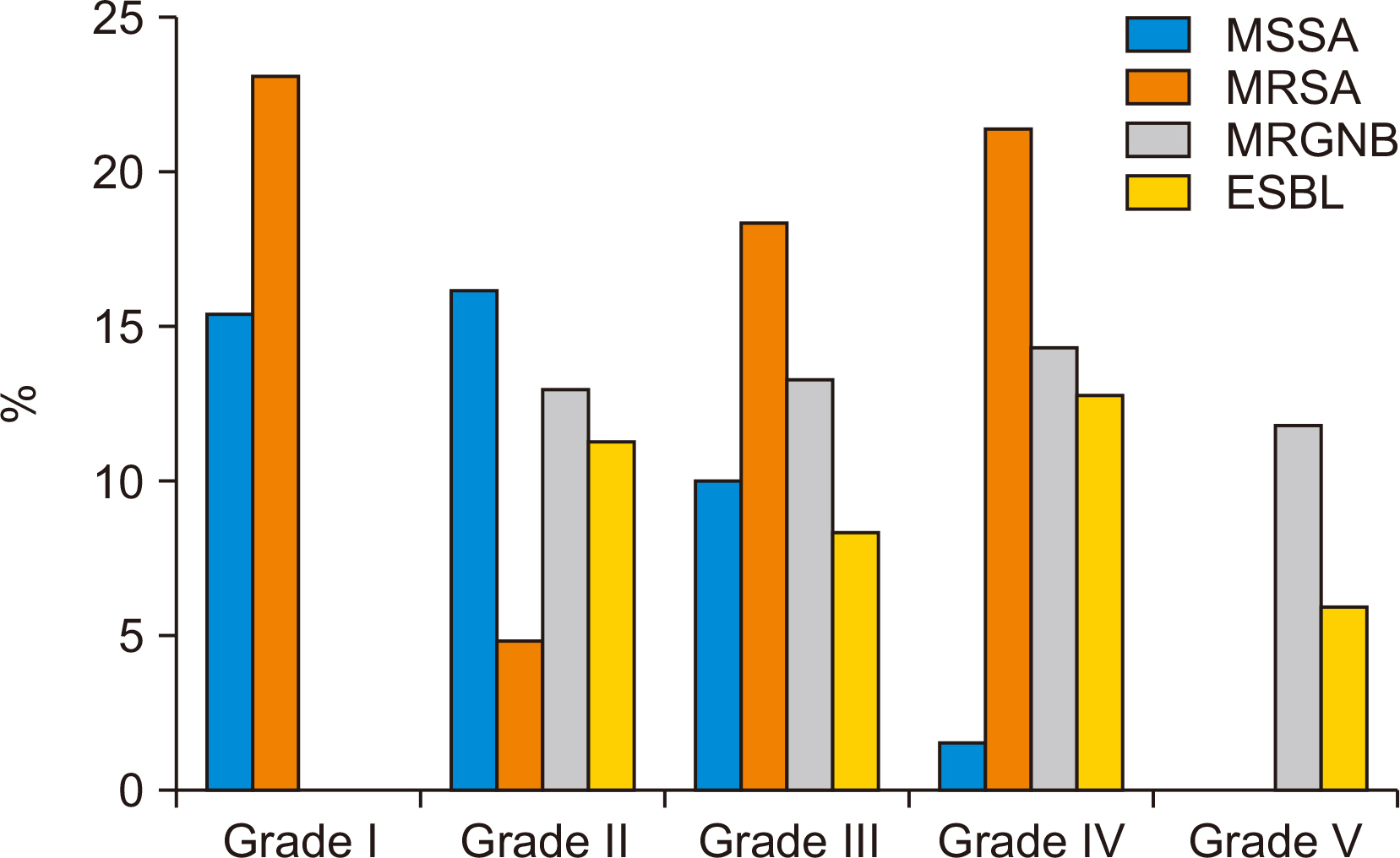
This study included 223 DFU patients that visited a single tertiary hospital and underwent bacterial culture between January 2016 and February 2020. The study was conducted in two parts: 1) to compare bacterial isolates and wound healing according to comorbidities such as chronic kidney disease (CKD) and peripheral artery disease (PAD), and 2) to compare bacterial isolates according to wound depth using the Wagner classification.
Results
Of the 223 patients, 43 had CKD (group A), 56 had PAD (group B), 30 had CKD and PAD (group C), and 94 had none of these comorbidities (group D). The isolation rate for multidrug-resistant gram-negative bacteria (MRGNB) and gram-negative to grampositive bacteria ratio were highest in group C (p=0.018, p=0.038), and the proportion that achieved wound healing was lowest in group C (p<0.001). In the second part of the study, subjects were classified into 5 grades by wound depth using the Wagner classification; 13 grade I, 62 grade II, 60 grade III, 70 grade IV, and 17 grade V. No significant difference was observed between these grades in terms of isolation rates or gram-negative to gram-positive bacteria ratios.
Conclusion
This study suggests antibiotics that cover gram-negative bacteria including MRGNB produces better results in the presence of CKD and PAD and that initial antibiotic choice should be based on the presence of CKD and PAD rather than wound depth.
Figure
Reference
-
1. Lavery LA, Armstrong DG, Wunderlich RP, Tredwell J, Boulton AJ. 2003; Diabetic foot syndrome: evaluating the prevalence and incidence of foot pathology in Mexican Americans and non-Hispanic whites from a diabetes disease management cohort. Diabetes Care. 26:1435–8. doi: 10.2337/diacare.26.5.1435. DOI: 10.2337/diacare.26.5.1435. PMID: 12716801.
Article2. Apelqvist J, Ragnarson-Tennvall G, Persson U, Larsson J. 1994; Diabetic foot ulcers in a multidisciplinary setting. An economic analysis of primary healing and healing with amputation. J Intern Med. 235:463–71. doi: 10.1111/j.1365-2796.1994.tb01104.x. DOI: 10.1111/j.1365-2796.1994.tb01104.x. PMID: 8182403.
Article3. Fisher TK, Scimeca CL, Bharara M, Mills JL Sr, Armstrong DG. 2010; A step-wise approach for surgical management of diabetic foot infections. J Vasc Surg. 52(3 Suppl):72S–5S. doi: 10.1016/j.jvs.2010.06.011. DOI: 10.1016/j.jvs.2010.06.011. PMID: 20804936.
Article4. Ertugrul BM, Oncul O, Tulek N, Willke A, Sacar S, Tunccan OG, et al. 2012; A prospective, multi-center study: factors related to the management of diabetic foot infections. Eur J Clin Microbiol Infect Dis. 31:2345–52. doi: 10.1007/s10096-012-1574-1. DOI: 10.1007/s10096-012-1574-1. PMID: 22354524.
Article5. Eleftheriadou I, Tentolouris N, Argiana V, Jude E, Boulton AJ. 2010; Methicillin-resistant Staphylococcus aureus in diabetic foot infections. Drugs. 70:1785–97. doi: 10.2165/11538070-000000000-00000. DOI: 10.2165/11538070-000000000-00000. PMID: 20836573.6. Ihm CG. 2000; Diabetic nephropathy. Korean J Med. 59:367–76. DOI: 10.3904/kjim.2019.109. PMID: 31048658. PMCID: PMC6506734.7. Kaminski M, Frescos N, Tucker S. 2012; Prevalence of risk factors for foot ulceration in patients with end-stage renal disease on haemodialysis. Intern Med J. 42:e120–8. doi: 10.1111/j.1445-5994.2011.02605.x. DOI: 10.1111/j.1445-5994.2011.02605.x. PMID: 21999812.
Article8. Margolis DJ, Hofstad O, Feldman HI. 2008; Association between renal failure and foot ulcer or lower-extremity amputation in patients with diabetes. Diabetes Care. 31:1331–6. doi: 10.2337/dc07-2244. DOI: 10.2337/dc07-2244.
Article9. Leskinen Y, Salenius JP, Lehtimäki T, Huhtala H, Saha H. 2002; The prevalence of peripheral arterial disease and medial arterial calcification in patients with chronic renal failure: requirements for diagnostics. Am J Kidney Dis. 40:472–9. doi: 10.1053/ajkd.2002.34885. DOI: 10.1053/ajkd.2002.34885. PMID: 12200797.
Article10. Prompers L, Huijberts M, Apelqvist J, Jude E, Piaggesi A, Bakker K, et al. 2007; High prevalence of ischaemia, infection and serious comorbidity in patients with diabetic foot disease in Europe. Baseline results from the Eurodiale study. Diabetologia. 50:18–25. doi: 10.1007/s00125-006-0491-1. DOI: 10.1007/s00125-006-0491-1. PMID: 17093942.
Article11. Kang MJ, Choi SH, Im S, Kong HS, Park MS, Heo CY, et al. 2008; The impact of peripheral arterial disease on the treatment and amputation of diabetic foot ulcer. J Korean Soc Vasc Surg. 24:113–8.12. Calhoun JH, Cantrell J, Cobos J, Lacy J, Valdez RR, Hokanson J, et al. 1988; Treatment of diabetic foot infections: Wagner classification, therapy, and outcome. Foot Ankle. 9:101–6. doi: 10.1177/107110078800900301. DOI: 10.1177/107110078800900301. PMID: 3229695.
Article13. Kirby AE, Garner K, Levin BR. 2012; The relative contributions of physical structure and cell density to the antibiotic susceptibility of bacteria in biofilms. Antimicrob Agents Chemother. 56:2967–75. doi: 10.1128/AAC.06480-11. DOI: 10.1128/AAC.06480-11. PMID: 22450987. PMCID: PMC3370779.
Article14. Bernstein BH, Tam H. 2005; Combination of subatmospheric pressure dressing and gravity feed antibiotic instillation in the treatment of postsurgical diabetic foot wounds: a case series. Wounds. 17:37–48.15. Benotmane A, Mohammedi F, Ayad F, Kadi K, Azzouz A. 2000; Diabetic foot lesions: etiologic and prognostic factors. Diabetes Metab. 26:113–7. PMID: 10804325.16. Song JY. 2011; Antimicrobial therapy in diabetic foot infections. J Korean Diabetes. 12:83–7. doi: 10.4093/jkd.2011.12.2.83. DOI: 10.4093/jkd.2011.12.2.83.
Article17. Seo YB, Noh JY, Huh JY, Lee J, Song JY, Han SK, et al. 2007; Diabetic foot infection: microbiologic analysis based on deep tissue biopsy. Infect Chemother. 39:237–42.18. Park SJ, Jung HJ, Shin HK, Kim E, Lim JJ, Yoon JW. 2009; Microbiology and antibiotic selection for diabetic foot infections. J Korean Foot Ankle Soc. 13:150–5.19. Aragón-Sánchez J, Lipsky BA, Lázaro-Martínez JL. 2013; Gram-negative diabetic foot osteomyelitis: risk factors and clinical presentation. Int J Low Extrem Wounds. 12:63–8. doi: 10.1177/1534734613477423. DOI: 10.1177/1534734613477423. PMID: 23446368.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Vascular Clogging, Wound Status and Bacterial Culture in Diabetic Foot Ulcers
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Prevention and Education for Diabetic Foot
- Current Trends in the Treatment of Diabetic Foot: Analysis of the Korean Foot and Ankle Society (KFAS) Member Survey
- Prevention of Diabetic Foot and Treatment of Pre-Ulcerative Signs