J Korean Diabetes.
2024 Mar;25(1):35-41. 10.4093/jkd.2024.25.1.35.
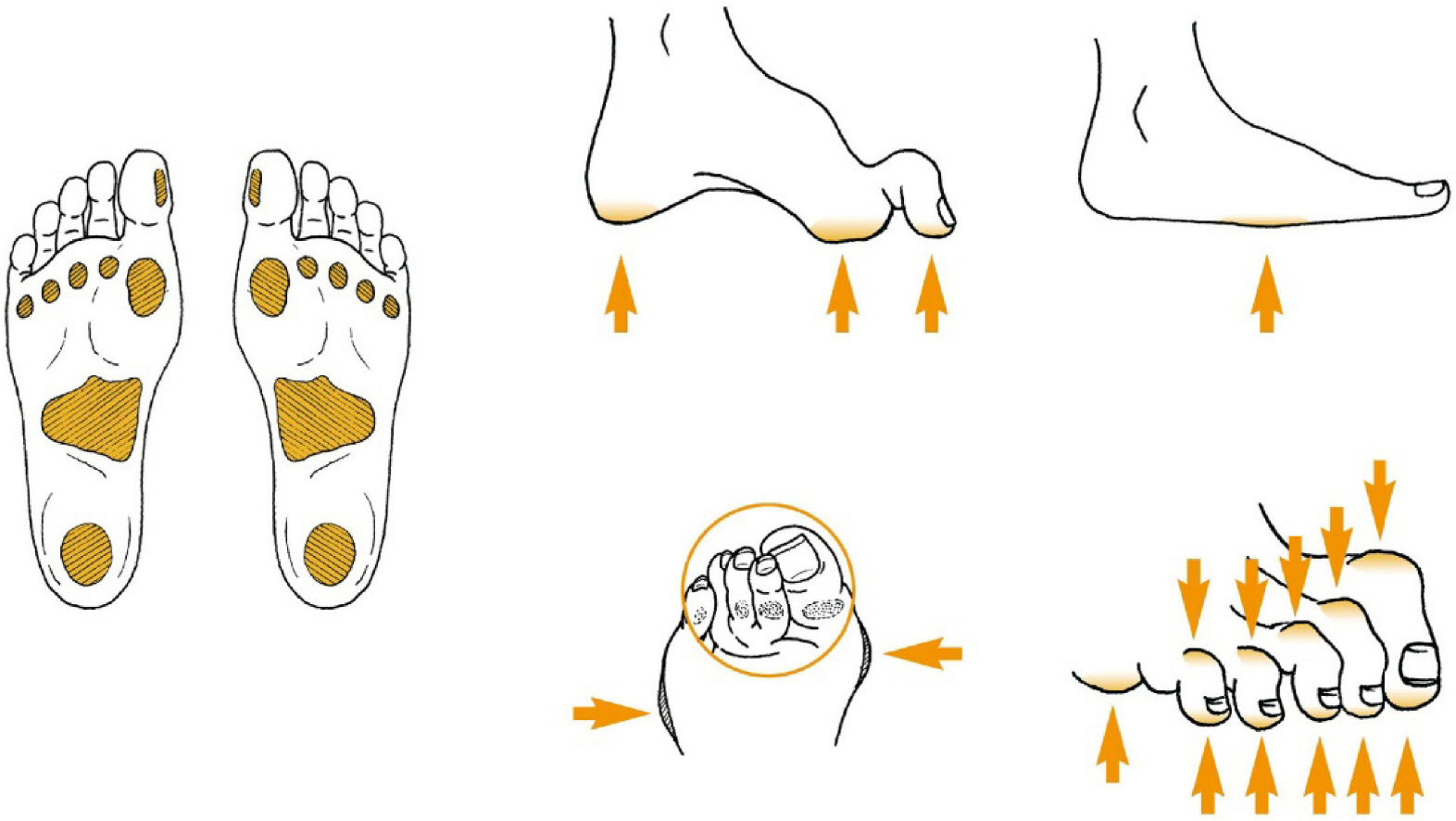
Prevention of Diabetic Foot and Treatment of Pre-Ulcerative Signs
- Affiliations
-
- 1Diabetic Wound Center, Korea University Guro Hospital, Seoul, Korea
- 2Department of Nursing, Korea University Guro Hospital, Seoul, Korea
- KMID: 2554119
- DOI: http://doi.org/10.4093/jkd.2024.25.1.35
Abstract
- Diabetes is one of the most prevalent chronic conditions and is expected to affect nearly 800 million people worldwide by 2045. Diabetes entails many complications; diabetic foot is among the most notorious complications. It requires complex long-term treatments and often has a high rate of relapse. Diabetic foot significantly threatens patient quality of life and imposes a considerable economic burden on both patients and healthcare systems. Therefore, prevention of diabetic foot is essential. It is important to identify patients at-risk of diabetic foot through regular check-ups and assessments. At-risk diabetic foot patients should be educated about foot self-care, appropriate footwear, and pre-ulcerative signs. Once pre-ulcerative lesions are found, swift intervention by trained professionals is necessary. Multidisciplinary collaboration in education of diabetic patients about diabetic foot is recommended and should consistently support patients in managing foot self-care.
Keyword
Figure
Reference
-
1.Schaper NC., van Netten JJ., Apelqvist J., Bus SA., Fitridge R., Game F, et al. Practical guidelines on the prevention and management of diabetes-related foot disease (IWGDF 2023 update). Diabetes Metab Res Rev. 2024. 40:e3657.
Article2.Pavicic T., Korting HC. Xerosis and callus formation as a key to the diabetic foot syndrome: dermatologic view of the problem and its management. J Dtsch Dermatol Ges. 2006. 4:935–41.
Article3.Armstrong DG., Boulton AJM., Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017. 376:2367–75.
Article4.Moxey PW., Gogalniceanu P., Hinchliffe RJ., Loftus IM., Jones KJ., Thompson MM, et al. Lower extremity ampu-tations - a review of global variability in incidence. Diabet Med. 2011. 28:1144–53.
Article5.Bus SA., Sacco ICN., Monteiro-Soares M., Raspovic A., Paton J., Rasmussen A, et al. Guidelines on the prevention of foot ulcers in persons with diabetes (IWGDF 2023 update). Diabetes Metab Res Rev. 2024. 40:e3651.
Article6.Han SG. Management of diabetic wound. Paju: Koonja;2008.7.Rayman G., Vas PR., Baker N., Taylor CG Jr., Gooday C., Alder AI, et al. The Ipswich touch test: a simple and novel method to identify inpatients with diabetes at risk of foot ulceration. Diabetes Care. 2011. 34:1517–8.8.Kozol RA., Bredenberg CE., Fey JD., Oates RP. Dependent rubor as a predictor of limb risk in patients with claudication. Arch Surg. 1984. 119:932–5.
Article9.Yang JP., Lee YN., Son JW., Han SK. The impact of extracorporeal shock wave therapy on microcirculation in diabetic feet: a pilot study. Adv Skin Wound Care. 2019. 32:563–7.
Article10.Nather A., Cao S., Chen JLW., Low AY. Prevention of diabetic foot complications. Singapore Med J. 2018. 59:291–4.
Article11.Baird SA., Skinner CM., Trail S., Frankis JS. Anhydrosis in the diabetic foot: a comparison of two urea creams. Diabetic Foot J. 2003. 6:122–36.12.Aan de Stegge WB., Mejaiti N., van Netten JJ., Dijkgraaf MGW., van Baal JG., Busch-Westbroek TE, et al. The cost-effectiveness and cost-utility of at-home infrared temperature monitoring in reducing the incidence of foot ulcer recurrence in patients with diabetes (DIATEMP): study protocol for a randomized controlled trial. Trials. 2018. 19:520.
Article13.Arts ML., Waaijman R., de Haart M., Keukenkamp R., Nollet F., Bus SA. Offloading effect of therapeutic footwear in patients with diabetic neuropathy at high risk for plantar foot ulceration. Diabet Med. 2012. 29:1534–41.
Article14.Reiber GE., Vileikyte L., Boyko EJ., del Aguila M., Smith DG., Lavery LA, et al. Causal pathways for incident low-er-extremity ulcers in patients with diabetes from two settings. Diabetes Care. 1999. 22:157–62.
Article15.Waaijman R., de Haart M., Arts ML., Wever D., Verlouw AJ., Nollet F, et al. Risk factors for plantar foot ulcer recurrence in neuropathic diabetic patients. Diabetes Care. 2014. 37:1697–705.
Article16.Murray HJ., Young MJ., Hollis S., Boulton AJ. The association between callus formation, high pressures and neuropathy in diabetic foot ulceration. Diabet Med. 1996. 13:979–82.
Article17.Richard JL., Sotto A., Lavigne JP. New insights in diabetic foot infection. World J Diabetes. 2011. 2:24–32.
Article18.Lim JZ., Ng NS., Thomas C. Prevention and treatment of diabetic foot ulcers. J R Soc Med. 2017. 110:104–9.
Article19.Thorud JC., Plemmons B., Buckley CJ., Shibuya N., Jupi-ter DC. Mortality after nontraumatic major amputation among patients with diabetes and peripheral vascular disease: a systematic review. J Foot Ankle Surg. 2016. 55:591–9.20.Rastogi A., Goyal G., Kesavan R., Bal A., Kumar H., Man-galanadanam , et al. Long term outcomes after incident diabetic foot ulcer: multicenter large cohort prospective study (EDI-FOCUS investigators) epidemiology of diabetic foot complications study: epidemiology of diabetic foot complications study. Diabetes Res Clin Pract. 2020. 162:108113.21.Pop-Busui R., Boulton AJ., Feldman EL., Bril V., Freeman R., Malik RA, et al. Diabetic neuropathy: a position statement by the American Diabetes Association. Diabetes Care. 2017. 40:136–54.
Article22.Schmidt BM., Holmes CM., Ye W., Pop-Busui R. A tale of two eras: mining big data from electronic health records to determine limb salvage rates with podiatry. Curr Diabetes Rev. 2019. 15:497–502.
Article23.Schmidt BM., Holmes CM., Najarian K., Gallagher K., Haus JM., Shadiow J, et al. On diabetic foot ulcer knowledge gaps, innovation, evaluation, prediction markers, and clin-ical needs. J Diabetes Complications. 2022. 36:108317.
Article24.Coffey L., Mahon C., Gallagher P. Perceptions and experi-ences of diabetic foot ulceration and foot care in people with diabetes: a qualitative meta-synthesis. Int Wound J. 2019. 16:183–210.
Article25.Apelqvist J., Larsson J. What is the most effective way to reduce incidence of amputation in the diabetic foot? Diabetes Metab Res Rev. 2000. 16(Suppl 1):S75–83.
Article