J Korean Med Sci.
2021 May;36(19):e127. 10.3346/jkms.2021.36.e127.
Effect of Opioids on All-cause Mortality and Sustained Opioid Use in Elderly Patients with Hip Fracture: a Korea Nationwide Cohort Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Gyeongsang National University Hospital, Jinju, Korea
- 2Department of Healthcare Management, Graduate School of Public Health, Yonsei University, Seoul, Korea
- 3Department of Orthopaedic Surgery, Eulji University Hospital, Daejeon, Korea
- 4Department of Orthopaedic Surgery, Yeungnam University Medical Center, Daegu, Korea
- 5Department of Orthopaedic Surgery, Ajou Medical Center, Suwon, Korea
- KMID: 2515862
- DOI: http://doi.org/10.3346/jkms.2021.36.e127
Abstract
- Background
The purpose of our study was to assess the use of opioids before and after hip fracture in elderly patients in order to determine the effect of opioid use on all-cause mortality, and to analyze how the history of opioid use before fracture increases the risk of sustained use following hip fracture using a Korea nationwide cohort.
Methods
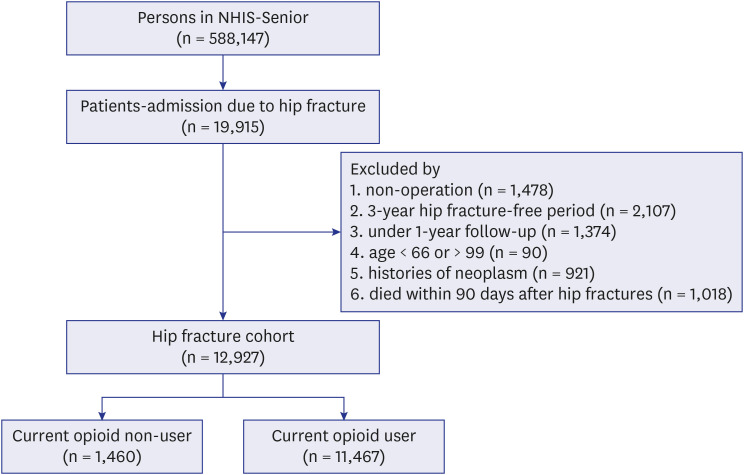
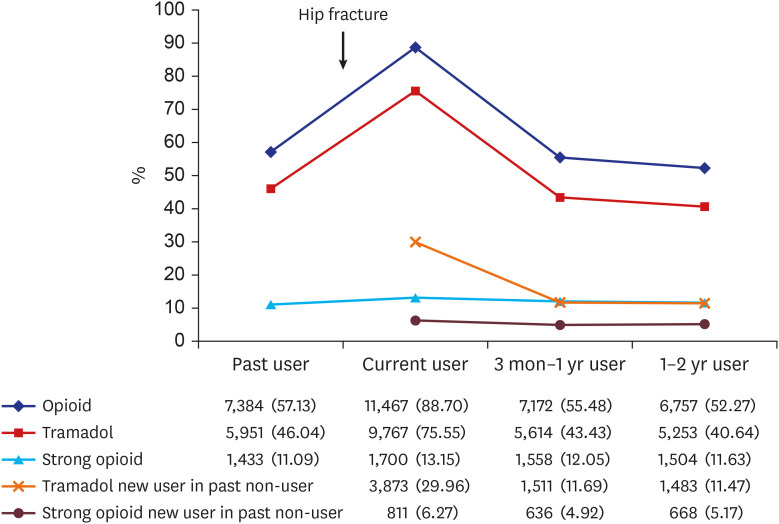
Our study identified hip fracture patients from the Korean National Health Insurance Service-Senior cohort. The index date was defined as 90-days after admission to the acute care hospital that fulfilled the eligibility criteria of elderly hip fracture. Patients were classified into past user, current user, and sustained user according to the use of opioid at each period based on the time of admission and index date. The opioids were classified into strong opioids and tramadol. A generalized estimating equation model with a Poisson distribution and logarithmic link function was performed to estimate the adjusted rate ratios (aRRs) and 95% confidence intervals (CIs) to assess the association between past use and sustained use. A multivariable-adjusted Cox proportional hazard model was used to investigate the effects of strong opioid and tramadol use on all-cause mortality.
Results
A total of 12,927 patients were included in our study. There were 7,384 (57.12%) opioid past-users, 11,467 (88.71%) opioid current-users, and 7,172 (55.48%) sustained users. In comparison of the death risk according to current use or the defined daily dose of the opioids or past opioid use, there were no significant differences in the adjusted hazard ratio for death in all groups, compared to the current non-users (P > 0.05). Among survivors 1 year after hip fracture, opioid past-use increased the risk of opioid sustained use by 1.52-fold (aRR; 95% CI, 1.45–1.8; P < 0.001).
Conclusion
Current use and past use of opioid did not increase all-cause mortality after hip fracture in elderly patients over 65 years of age. Past use of opioid before hip fracture increased risk of sustained use of opioid compared to the current opioid used without past use.
Keyword
Figure
Reference
-
1. Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017; 137(5):625–630. PMID: 28321571.
Article2. A'Court J, Lees D, Harrison W, Ankers T, Reed MR. Pain and analgesia requirements with hip fracture surgery. Orthop Nurs. 2017; 36(3):224–228. PMID: 28538539.3. Jang SY, Cha YH, Mun YS, Kim SH, Kim HY, Choy WS. Acute cholecystitis in elderly patients after hip fracture: a nationwide cohort study. J Korean Med Sci. 2019; 34(5):e36. PMID: 30718989.
Article4. Lindestrand AG, Christiansen ML, Jantzen C, van der Mark S, Andersen SE. Opioids in hip fracture patients: an analysis of mortality and post hospital opioid use. Injury. 2015; 46(7):1341–1345. PMID: 25952252.
Article5. Fabi DW. Multimodal analgesia in the hip fracture patient. J Orthop Trauma. 2016; 30(Suppl 1):S6–S11. PMID: 27101321.
Article6. Flanagan CD, Fuell Wysong E, Ramey JS, Gunasekar A, Vallier HA. Traumatic orthopaedic injury is not an independent risk factor for high postdischarge opioid consumption. J Am Acad Orthop Surg Glob Res Rev. 2017; 1(8):e058. PMID: 30211368.
Article7. Simoni AH, Nikolajsen L, Olesen AE, Christiansen CF, Pedersen AB. Opioid use after hip fracture surgery: a Danish nationwide cohort study from 2005 to 2015. Eur J Pain. 2019; 23(7):1309–1317. PMID: 30848038.
Article8. Maiese BA, Pham AT, Shah MV, Eaddy MT, Lunacsek OE, Wan GJ. Hospitalization costs for patients undergoing orthopedic surgery treated with intravenous acetaminophen (IV-APAP) plus other IV analgesics or IV opioid monotherapy for postoperative pain. Adv Ther. 2017; 34(2):421–435. PMID: 27943118.
Article9. Kim YI, Kim YY, Yoon JL, Won CW, Ha S, Cho KD, et al. Cohort profile: National Health Insurance Service-senior (NHIS-senior) cohort in Korea. BMJ Open. 2019; 9(7):e024344.
Article10. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):e016640.
Article11. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the National Health Insurance Service-National Sample Cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15. PMID: 26822938.
Article12. Park C, Jang S, Jang S, Ha YC, Lee YK, Yoon HK, et al. Identification and validation of osteoporotic hip fracture using the national health insurance database. J Korean Hip Soc. 2010; 22(4):305–311.
Article13. Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24(11):2887–2892. PMID: 23681088.
Article14. Cho SK, Jung SY, Choi S, Im SG, Kim H, Choi WS, et al. Factors related to the use of opioids as early treatment in patients with knee osteoarthritis. Arthritis Res Ther. 2019; 21(1):222. PMID: 31685008.
Article15. Cha Y, Jang SY, Yoo JI, Choi HG, Hwang JW, Choy W. Effect of opioids on all-cause mortality and opioid addiction in total hip arthroplasty: a Korea nationwide cohort study. J Korean Med Sci. 2021; 36(13):e87. PMID: 33821594.
Article16. WHO Collaborating Center for Drug Statistics Methodology. ATC/DDD index 2020. Updated 2020. Assessed January 1, 2020. https://www.whocc.no/atc_ddd_index/.17. Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005; 43(11):1130–1139. PMID: 16224307.
Article18. Morone NE, Weiner DK. Pain as the fifth vital sign: exposing the vital need for pain education. Clin Ther. 2013; 35(11):1728–1732. PMID: 24145043.
Article19. Hannon CP, Calkins TE, Li J, Culvern C, Darrith B, Nam D, et al. The James A. Rand Young Investigator's Award: large opioid prescriptions are unnecessary after total joint arthroplasty: a randomized controlled trial. J Arthroplasty. 2019; 34(7S):S4–10. PMID: 30799266.20. Birke H, Kurita GP, Sjøgren P, Højsted J, Simonsen MK, Juel K, et al. Chronic non-cancer pain and the epidemic prescription of opioids in the Danish population: trends from 2000 to 2013. Acta Anaesthesiol Scand. 2016; 60(5):623–633. PMID: 26861026.
Article21. Larochelle MR, Zhang F, Ross-Degnan D, Wharam JF. Trends in opioid prescribing and co-prescribing of sedative hypnotics for acute and chronic musculoskeletal pain: 2001–2010. Pharmacoepidemiol Drug Saf. 2015; 24(8):885–892. PMID: 25906971.
Article22. Birke H, Ekholm O, Sjøgren P, Kurita GP, Højsted J. Long-term opioid therapy in Denmark: a disappointing journey. Eur J Pain. 2017; 21(9):1516–1527. PMID: 28481052.
Article23. Lindestrand AG, Christiansen MLS, Jantzen C, van der Mark S, Andersen SE. Opioids in hip fracture patients: an analysis of mortality and post hospital opioid use. Injury. 2015; 46(7):1341–1345. PMID: 25952252.
Article24. Gallagher R. New category of opioid-related death. Can Fam Physician. 2018; 64(2):95–96. PMID: 29449232.25. Summers S, Grau L, Massel D, Rosas S, Ong A, Hernandez VH. Opioid use disorders are associated with perioperative morbidity and mortality in the hip fracture population. J Orthop Trauma. 2018; 32(5):238–244. PMID: 29356800.
Article26. Subedi M, Bajaj S, Kumar MS, Yc M. An overview of tramadol and its usage in pain management and future perspective. Biomed Pharmacother. 2019; 111:443–451. PMID: 30594783.
Article27. By the American Geriatrics Society 2015 Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015; 63(11):2227–2246. PMID: 26446832.28. Bachhuber MA, Hennessy S, Cunningham CO, Starrels JL. Increasing benzodiazepine prescriptions and overdose mortality in the United States, 1996–2013. Am J Public Health. 2016; 106(4):686–688. PMID: 26890165.
Article29. Morris BJ, Mir HR. The opioid epidemic: impact on orthopaedic surgery. J Am Acad Orthop Surg. 2015; 23(5):267–271. PMID: 25911660.30. Cozowicz C, Olson A, Poeran J, Mörwald EE, Zubizarreta N, Girardi FP, et al. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain. 2017; 158(12):2422–2430. PMID: 28891865.
Article31. Bonner BE, Castillo TN, Fitz DW, Zhao JZ, Klemt C, Kwon YM. Preoperative opioid use negatively affects patient-reported outcomes after primary total hip arthroplasty. J Am Acad Orthop Surg. 2019; 27(22):e1016–20. PMID: 30829899.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Opioids on All-cause Mortality and Opioid Addiction in Total Hip Arthroplasty: a Korea Nationwide Cohort Study
- Incidence, Morbidity and Mortality in Patients Older than 50 Years with Second Hip Fracture in a Jeju Cohort Study
- The incidence of hip fracture and mortality rate after hip fracture in Korea: A nationwide population-based cohort study
- The Prevalence of Clostridium difficile Colitis and Effect on All-Cause Mortality in Elderly Patients after Hip Fracture Surgery: A Korean Nationwide Cohort Study
- Postoperative Mortality and the Associated Factors in Elderly Patients with Hip Fracture