Korean J Orthod.
2021 May;51(3):157-165. 10.4041/kjod.2021.51.3.157.
The effect of different micro-osteoperforation depths on the rate of orthodontic tooth movement: A singlecenter, single-blind, randomized clinical trial
- Affiliations
-
- 1Department of Oral and Dental Health Program, Üsküdar University Vocational School of Health Services, İstanbul, Turkey
- 2Department of Orthodontics, Faculty of Dentistry, Ondokuz Mayıs University, Atakum, Samsun, Turkey
- KMID: 2515819
- DOI: http://doi.org/10.4041/kjod.2021.51.3.157
Abstract
Objective
This study aimed to identify the clinical effectiveness of two different penetration depths of micro-osteoperforations (MOPs) on the rate of orthodontic tooth movement.
Methods
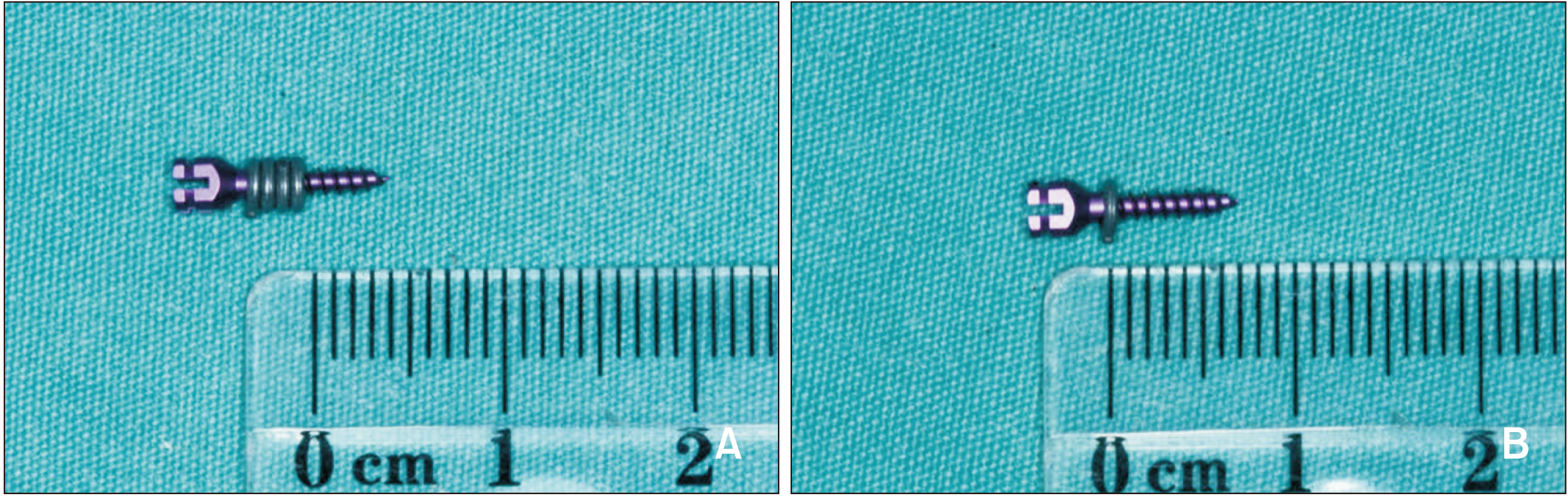
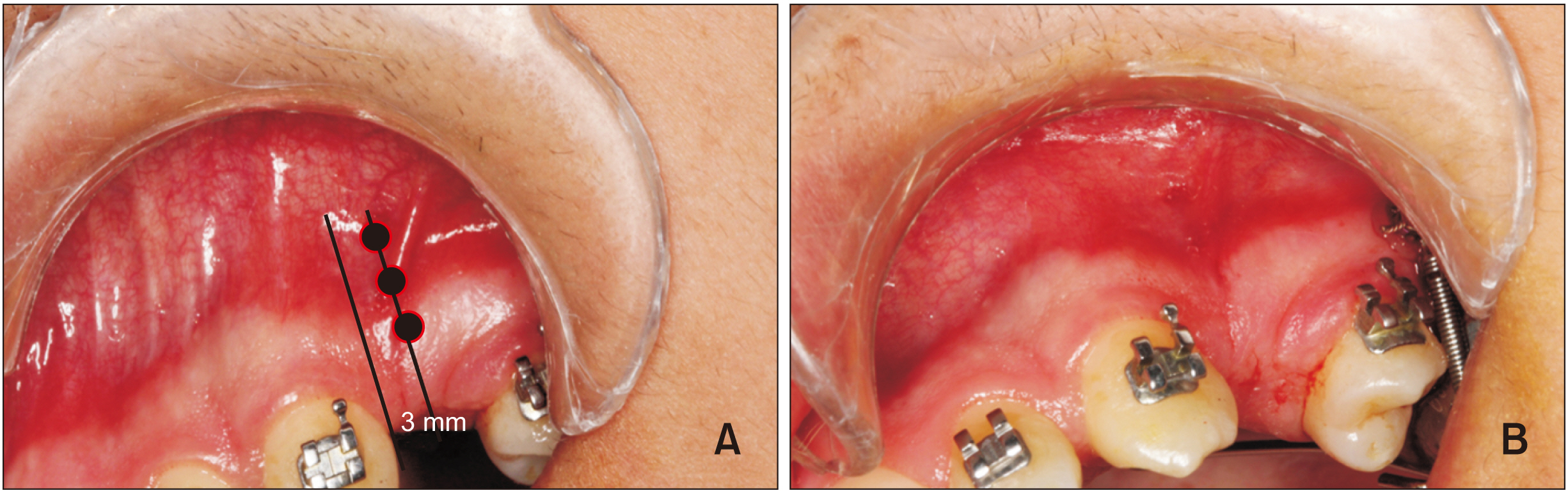
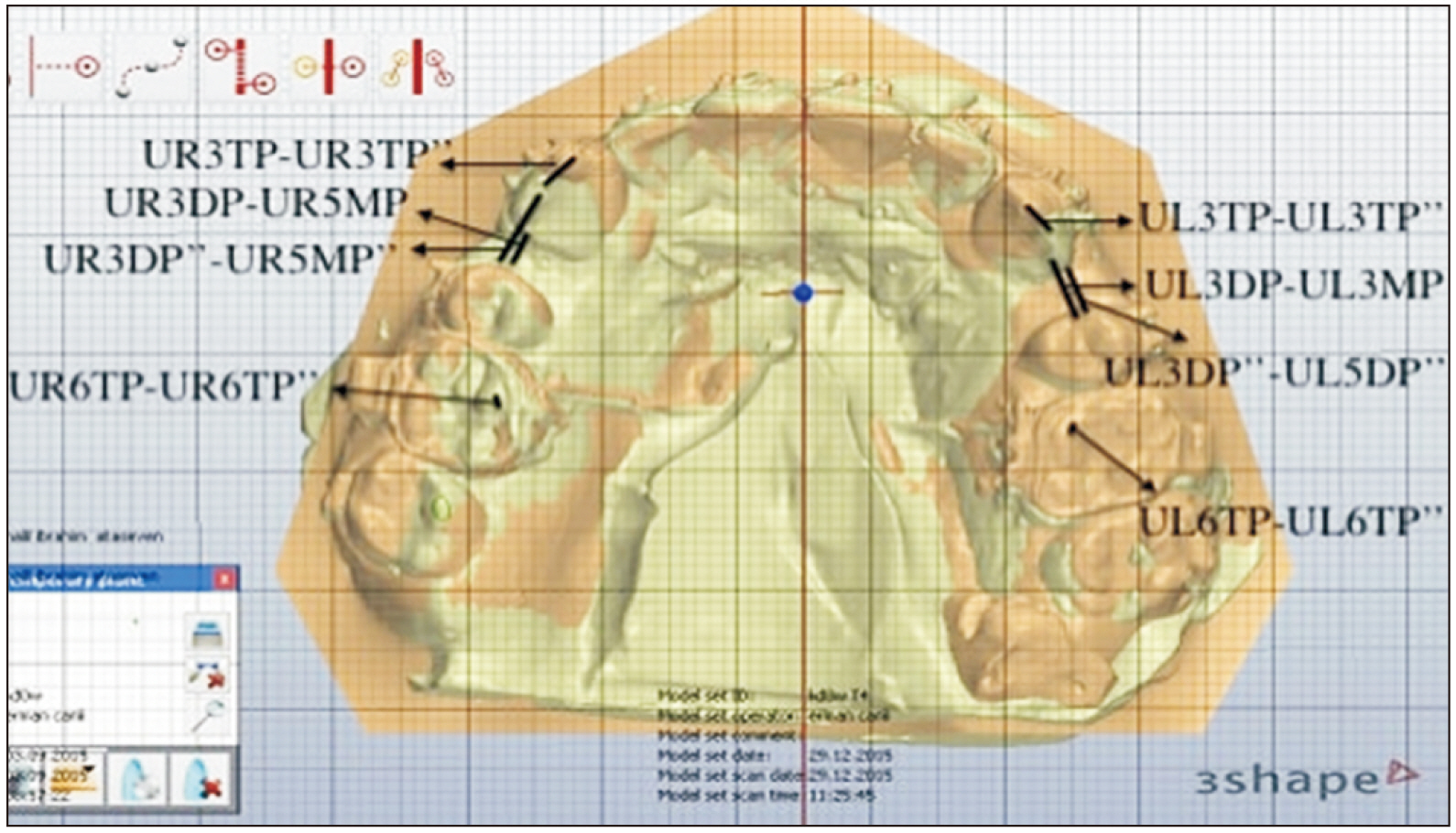
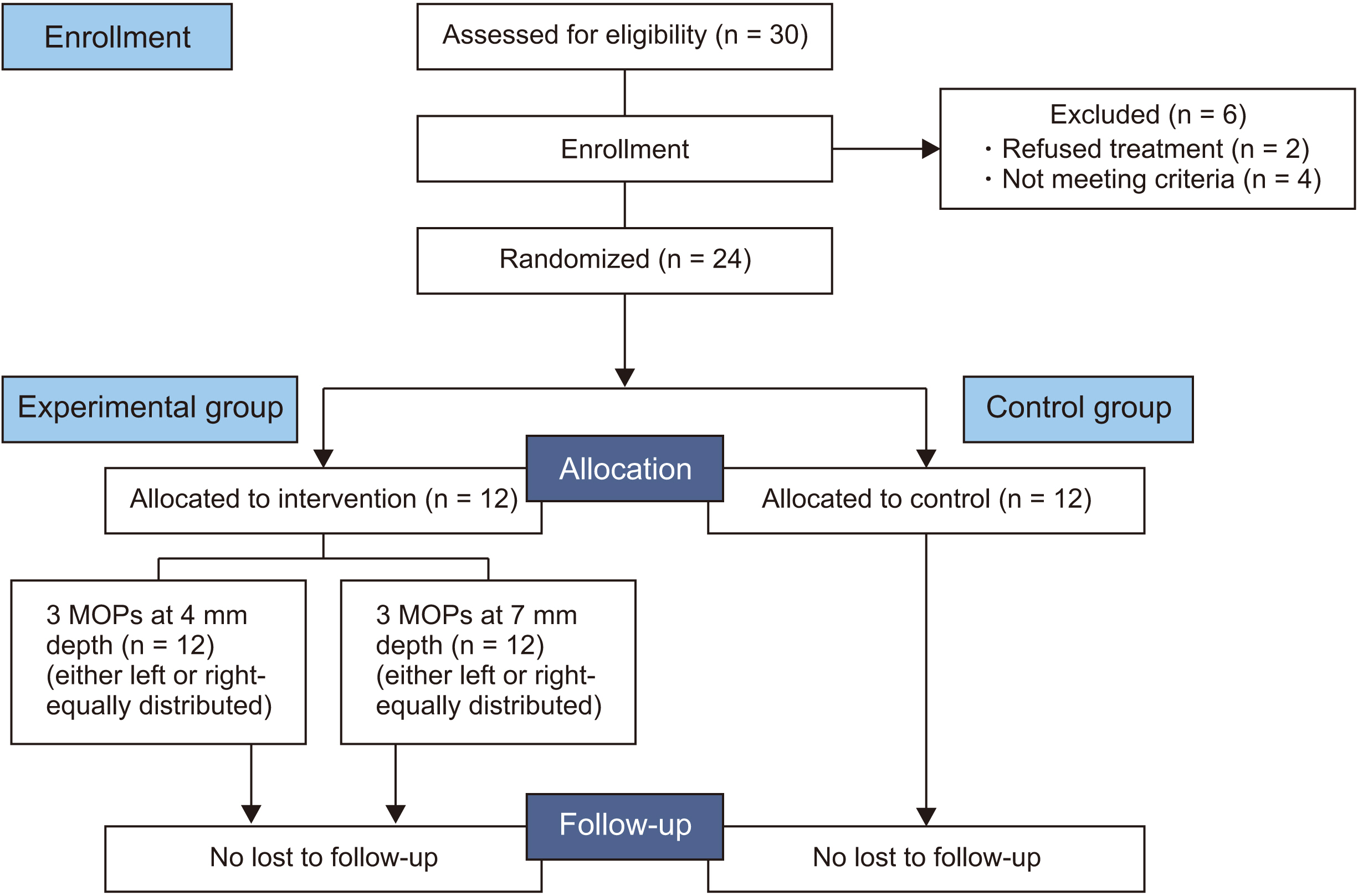
Twenty-four patients requiring the removal of the upper first premolar teeth were selected and randomly divided into two groups. The control group participants did not undergo MOPs. Participants in the experimental group underwent three MOPs each at 4-mm (MOP-4) and 7-mm (MOP-7) depths, which were randomly and equally performed to either the left or right side distal to the canine. The retraction amount was measured on three-dimensional digital models on the 28th day of retraction. MOP-related pain was measured using a visual analog scale (VAS). Between-group statistical differences in the VAS scores were determined using an independent t-test and those in canine retraction were determined using analysis of variance and posthoc Tukey test.
Results
No significant difference was found between the MOP-4 (1.22 ± 0.29 mm/month) and MOP-7 (1.29 ± 0.31 mm/month) groups in terms of the canine retraction rate. Moreover, both the groups demonstrated a significantly higher canine movement than the control group (0.88 ± 0.19 mm/ month). MOPs did not significantly affect the mesialization of the posterior teeth (p > 0.05). Moreover, the pain scores in the MOP-4 and MOP-7 groups were similar and showed no statistically significant difference.
Conclusions
Three MOPs with a depth of 4 mm can be performed as an effective method to increase the rate of tooth movement. However, three MOPs with depths of 4–7 mm does not additionally enhance tooth movement.
Keyword
Figure
Reference
-
1. Tsichlaki A, Chin SY, Pandis N, Fleming PS. 2016; How long does treatment with fixed orthodontic appliances last? A systematic review. Am J Orthod Dentofacial Orthop. 149:308–18. DOI: 10.1016/j.ajodo.2015.09.020. PMID: 26926017.
Article2. Uribe F, Padala S, Allareddy V, Nanda R. 2014; Patients', parents', and orthodontists' perceptions of the need for and costs of additional procedures to reduce treatment time. Am J Orthod Dentofacial Orthop. 145(4 Suppl):S65–73. DOI: 10.1016/j.ajodo.2013.12.015. PMID: 24680026.
Article3. Talic NF. 2011; Adverse effects of orthodontic treatment: a clinical perspective. Saudi Dent J. 23:55–9. DOI: 10.1016/j.sdentj.2011.01.003. PMID: 24151415. PMCID: PMC3770235.
Article4. Soma S, Matsumoto S, Higuchi Y, Takano-Yamamoto T, Yamashita K, Kurisu K, et al. 2000; Local and chronic application of PTH accelerates tooth movement in rats. J Dent Res. 79:1717–24. DOI: 10.1177/00220345000790091301. PMID: 11023269.
Article5. Nishimura M, Chiba M, Ohashi T, Sato M, Shimizu Y, Igarashi K, et al. 2008; Periodontal tissue activation by vibration: intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am J Orthod Dentofacial Orthop. 133:572–83. DOI: 10.1016/j.ajodo.2006.01.046. PMID: 18405822.
Article6. Yavuz MC, Sunar O, Buyuk SK, Kantarcı A. 2018; Comparison of piezocision and discision methods in orthodontic treatment. Prog Orthod. 19:44. DOI: 10.1186/s40510-018-0244-y. PMID: 30370430. PMCID: PMC6204431.
Article7. Alikhani M, Alansari S, Sangsuwon C, Alikhani M, Chou MY, Alyami B, et al. 2015; Micro-osteoperforations: minimally invasive accelerated tooth movement. Semin Orthod. 21:162–9. DOI: 10.1053/j.sodo.2015.06.002.
Article8. Teixeira CC, Khoo E, Tran J, Chartres I, Liu Y, Thant LM, et al. 2010; Cytokine expression and accelerated tooth movement. J Dent Res. 89:1135–41. DOI: 10.1177/0022034510373764. PMID: 20639508. PMCID: PMC3318047.
Article9. Alikhani M, Raptis M, Zoldan B, Sangsuwon C, Lee YB, Alyami B, et al. 2013; Effect of micro-osteoperforations on the rate of tooth movement. Am J Orthod Dentofacial Orthop. 144:639–48. DOI: 10.1016/j.ajodo.2013.06.017. PMID: 24182579.
Article10. Nicozisis JL. 2013; Accelerated orthodontics through microosteoperforation. Orthod Pract. 4:56–7.11. Feizbakhsh M, Zandian D, Heidarpour M, Farhad SZ, Fallahi HR. 2018; The use of micro-osteoperforation concept for accelerating differential tooth movement. J World Fed Orthod. 7:56–60. DOI: 10.1016/j.ejwf.2018.04.002.
Article12. Schulz KF, Altman DG, Moher D. CONSORT Group. 2010; CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 8:18. DOI: 10.1186/1741-7015-8-18. PMID: 20334633. PMCID: PMC2860339.
Article13. Galvão MCS, Sato JR, Coelho EC. 2012; Dahlberg formula: a novel approach for its evaluation. Dental Press J Orthod. 17:115–24. DOI: 10.1590/S2176-94512012000100015.
Article14. Alkebsi A, Al-Maaitah E, Al-Shorman H, Abu Alhaija E. 2018; Three-dimensional assessment of the effect of micro-osteoperforations on the rate of tooth movement during canine retraction in adults with Class II malocclusion: a randomized controlled clinical trial. Am J Orthod Dentofacial Orthop. 153:771–85. DOI: 10.1016/j.ajodo.2017.11.026. PMID: 29853235.
Article15. George D, Mallery P. 2010. SPSS for Windows step by step: a simple guide and reference, 17.0 update. Pearson;Boston:16. Aboalnaga AA, Salah Fayed MM, El-Ashmawi NA, Soliman SA. 2019; Effect of micro-osteoperforation on the rate of canine retraction: a split-mouth randomized controlled trial. Prog Orthod. 20:21. DOI: 10.1186/s40510-019-0274-0. PMID: 31155698. PMCID: PMC6545296.
Article17. Cheung T, Park J, Lee D, Kim C, Olson J, Javadi S, et al. 2016; Ability of mini-implant-facilitated micro-osteoperforations to accelerate tooth movement in rats. Am J Orthod Dentofacial Orthop. 150:958–67. DOI: 10.1016/j.ajodo.2016.04.030. PMID: 27894545. PMCID: PMC5131371.
Article18. Haliloglu-Ozkan T, Arici N, Arici S. 2018; In-vivo effects of flapless osteopuncture-facilitated tooth movement in the maxilla and the mandible. J Clin Exp Dent. 10:e761–7. DOI: 10.4317/jced.54981. PMID: 30305873. PMCID: PMC6174022.
Article19. Azeem M, Ul Haq A, Ilyas M, Ul Hamid W, Hayat MB, Jamal F, et al. 2018; Bacteremia after micro-osteoperforation. Int Orthod. 16:463–9. DOI: 10.1016/j.ortho.2018.06.001. PMID: 30006078.
Article20. Lee JW, Cha JY, Park KH, Kang YG, Kim SJ. 2018; Effect of flapless osteoperforation-assisted tooth movement on atrophic alveolar ridge: histomorphometric and gene-enrichment analysis. Angle Orthod. 88:82–90. DOI: 10.2319/061217-388.1. PMID: 29016190.
Article21. Sivarajan S, Doss JG, Papageorgiou SN, Cobourne MT, Wey MC. 2019; Mini-implant supported canine retraction with micro-osteoperforation: a split-mouth randomized clinical trial. Angle Orthod. 89:183–9. DOI: 10.2319/011518-47.1. PMID: 30372126.
Article22. Cramer CL, Campbell PM, Opperman LA, Tadlock LP, Buschang PH. 2019; Effects of micro-osteoperforations on tooth movement and bone in the beagle maxilla. Am J Orthod Dentofacial Orthop. 155:681–92. DOI: 10.1016/j.ajodo.2018.06.015. PMID: 31053284.
Article23. Andrade I Jr, Sousa AB, da Silva GG. 2014; New therapeutic modalities to modulate orthodontic tooth movement. Dental Press J Orthod. 19:123–33. DOI: 10.1590/2176-9451.19.6.123-133.sar. PMID: 25628089. PMCID: PMC4347420.24. Shahabee M, Shafaee H, Abtahi M, Rangrazi A, Bardideh E. 2020; Effect of micro-osteoperforation on the rate of orthodontic tooth movement-a systematic review and a meta-analysis. Eur J Orthod. 42:211–21. DOI: 10.1093/ejo/cjz049. PMID: 31215993.
Article25. Kundi I, Alam MK, Shaheed S. 2020; Micro-osteo perforation effects as an intervention on canine retraction. Saudi Dent J. 32:15–20. DOI: 10.1016/j.sdentj.2019.05.009. PMID: 31920274. PMCID: PMC6950836.
Article26. Attri S, Mittal R, Batra P, Sonar S, Sharma K, Raghavan S, et al. 2018; Comparison of rate of tooth movement and pain perception during accelerated tooth movement associated with conventional fixed appliances with micro-osteoperforations- a randomised controlled trial. J Orthod. 45:225–33. DOI: 10.1080/14653125.2018.1528746. PMID: 30281397.27. Alikhani M. 2017. Clinical guide to accelerated orthodontics with a focus on micro-osteoperforations. Springer;Cham: DOI: 10.1007/978-3-319-43401-8.28. Kolte R, Kolte A, Mahajan A. 2014; Assessment of gingival thickness with regards to age, gender and arch location. J Indian Soc Periodontol. 18:478–81. DOI: 10.4103/0972-124X.138699. PMID: 25210263. PMCID: PMC4158590.
Article29. Müller HP, Könönen E. 2005; Variance components of gingival thickness. J Periodontal Res. 40:239–44. DOI: 10.1111/j.1600-0765.2005.00798.x. PMID: 15853970.
Article30. Işik Aslan B, Baloştuncer B, Dinçer M. 2013; Are there differences on tooth movement between different sectional canine retractors? J Orofac Orthop. 74:226–35. DOI: 10.1007/s00056-013-0142-3. PMID: 23649279.
Article31. Kini U, Nandeesh BN. Fogelman I, Gnanasegaran G, van der Wall H, editors. 2012. Physiology of bone formation, remodeling, and metabolism. Radionuclide and hybrid bone imaging. Springer;Berlin, Heidelberg: p. 29–57. DOI: 10.1007/978-3-642-02400-9_2.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of tooth movement and biological response in corticotomy and micro-osteoperforation in rabbits
- The effects of electrical current from a micro-electrical device on tooth movement
- Mode of tooth movement according to the timing of orthodontic force application after extraction
- An experimental study on the effect of half sine-wave pulsed electromagnetic field in orthodontic tooth movement
- Comparison of clinical and histological characteristics of orthodontic tooth movement into recent and healed extraction sites combined with corticotomy in rats