Intest Res.
2021 Apr;19(2):232-238. 10.5217/ir.2019.09181.
Prospective validation of CD4+CD25+FOXP3+ T-regulatory cells as an immunological marker to differentiate intestinal tuberculosis from Crohn’s disease
- Affiliations
-
- 1Department of Gastroenterology, All India Institute of Medical Sciences, New Delhi, India
- KMID: 2515482
- DOI: http://doi.org/10.5217/ir.2019.09181
Abstract
- Background/Aims
Crohn’s disease (CD) and intestinal tuberculosis (ITB) remain “difficult-to-differentiate” diseases. We have previously documented peripheral blood frequency of CD4+CD25+FOXP3+ T-regulatory cells (Treg) as a biomarker to differentiate CD and ITB. We tried to validate these results in a larger cohort of CD and ITB patients.
Methods
Seventy treatment naïve patients of CD (n = 23) and ITB (n = 47) (diagnosed by standard criteria) were recruited prospectively from October 2016 to May 2017. Patients with history of antitubercular therapy in the past were excluded. The frequency of Treg cells in peripheral blood was determined by flow cytometry, and compared between CD and ITB patients.
Results
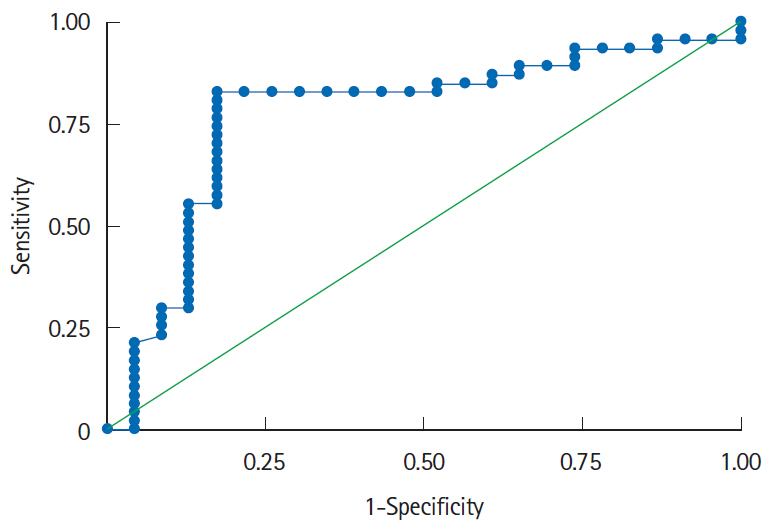
Similar to our previous study, frequency of Treg cells in peripheral blood was significantly increased in ITB as compared to CD patients (40.9 [interquartile range, 33–50] vs. 24.9 [interquartile range, 14.4–29.6], P< 0.001). Further, the receiver operating characteristics curve also showed good diagnostic accuracy with an area under the curve (AUC) of 0.77 (95% confidence interval, 0.65–0.89) and a FOXP3+ cutoff value of > 31.3% had a sensitivity and specificity of 83% and 82.6% respectively, to differentiate ITB from CD. Even for the indeterminate cases (n = 33), Treg cell frequency had similar diagnostic accuracy with an AUC of 0.85 (95% confidence interval, 0.68–0.95) and a cutoff of 32.37% had sensitivity and specificity of 87% and 95% respectively, to differentiate ITB from CD.
Conclusions
The current findings validate that the increased frequency of CD4+CD25+FOXP3+ Treg in the peripheral blood can be used as a biomarker with high diagnostic accuracy to differentiate ITB from CD.
Figure
Cited by 1 articles
-
Addition of computed tomography chest increases the diagnosis rate in patients with suspected intestinal tuberculosis
Saurabh Kedia, Raju Sharma, Sudheer Kumar Vuyyuru, Deepak Madhu, Pabitra Sahu, Bhaskar Kante, Prasenjit Das, Ankur Goyal, Karan Madan, Govind Makharia, Vineet Ahuja
Intest Res. 2022;20(2):184-191. doi: 10.5217/ir.2020.00104.
Reference
-
1. Singh P, Ananthakrishnan A, Ahuja V. Pivot to Asia: inflammatory bowel disease burden. Intest Res. 2017; 15:138–141.
Article2. Ng SC, Tang W, Ching JY, et al. Incidence and phenotype of inflammatory bowel disease based on results from the Asiapacific Crohn’s and colitis epidemiology study. Gastroenterology. 2013; 145:158–165.
Article3. Makharia GK, Srivastava S, Das P, et al. Clinical, endoscopic, and histological differentiations between Crohn’s disease and intestinal tuberculosis. Am J Gastroenterol. 2010; 105:642–651.
Article4. Lee YJ, Yang SK, Byeon JS, et al. Analysis of colonoscopic findings in the differential diagnosis between intestinal tuberculosis and Crohn’s disease. Endoscopy. 2006; 38:592–597.
Article5. Pulimood AB, Peter S, Ramakrishna B, et al. Segmental colonoscopic biopsies in the differentiation of ileocolic tuberculosis from Crohn’s disease. J Gastroenterol Hepatol. 2005; 20:688–696.
Article6. Kedia S, Sharma R, Nagi B, et al. Computerized tomography-based predictive model for differentiation of Crohn’s disease from intestinal tuberculosis. Indian J Gastroenterol. 2015; 34:135–143.
Article7. Kedia S, Sharma R, Sreenivas V, et al. Accuracy of computed tomographic features in differentiating intestinal tuberculosis from Crohn’s disease: a systematic review with meta-analysis. Intest Res. 2017; 15:149–159.
Article8. Ng SC, Hirai HW, Tsoi KK, et al. Systematic review with meta-analysis: accuracy of interferon-gamma releasing assay and anti-Saccharomyces cerevisiae antibody in differentiating intestinal tuberculosis from Crohn’s disease in Asians. J Gastroenterol Hepatol. 2014; 29:1664–1670.
Article9. Ooi CJ, Makharia GK, Hilmi I, et al. Asia Pacific consensus statements on Crohn’s disease. Part 1: Definition, diagnosis, and epidemiology. J Gastroenterol Hepatol. 2016; 31:45–55.
Article10. Gupta A, Mouli VP, Mohta S, et al. Antitubercular therapy given to differentiate Crohn’s disease from intestinal tuberculosis predisposes to stricture formation. J Crohns Colitis. 2020; 14:1611–1618.
Article11. He XY, Xiao L, Chen HB, et al. T regulatory cells and Th1/Th2 cytokines in peripheral blood from tuberculosis patients. Eur J Clin Microbiol Infect Dis. 2010; 29:643–650.
Article12. Díaz A, Santucci N, Bongiovanni B, et al. Increased frequency of CD4+ CD25+ FoxP3+ T regulatory cells in pulmonary tuberculosis patients undergoing specific treatment and its relationship with their immune-endocrine profile. J Immunol Res. 2015; 2015:985302.13. Tiwari V, Kedia S, Garg SK, et al. CD4+ CD25+ FOXP3+ T cell frequency in the peripheral blood is a biomarker that distinguishes intestinal tuberculosis from Crohn’s disease. PLoS One. 2018; 13:e0193433.14. Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn’s disease 2016: part 1. diagnosis and medical management. J Crohns Colitis. 2017; 11:3–25.
Article15. Paustian FF, Marshall JB. Intestinal tuberculosis. In : Berk JE, editor. Bockus gastroenterology. 4th ed. Philadelphia: WB Saunders;1985. p. 2018–2036.16. Logan VS. Anorectal tuberculosis. Proc R Soc Med. 1969; 62:1227–1230.17. Pratap Mouli V, Munot K, Ananthakrishnan A, et al. Endoscopic and clinical responses to anti-tubercular therapy can differentiate intestinal tuberculosis from Crohn’s disease. Aliment Pharmacol Ther. 2017; 45:27–36.
Article18. Wang Y, Liu XP, Zhao ZB, Chen JH, Yu CG. Expression of CD4+ forkhead box P3 (FOXP3)+ regulatory T cells in inflammatory bowel disease. J Dig Dis. 2011; 12:286–294.
Article19. Maul J, Loddenkemper C, Mundt P, et al. Peripheral and intestinal regulatory CD4+ CD25 (high) T cells in inflammatory bowel disease. Gastroenterology. 2005; 128:1868–1878.
Article20. Eastaff-Leung N, Mabarrack N, Barbour A, Cummins A, Barry S. Foxp3+ regulatory T cells, Th17 effector cells, and cytokine environment in inflammatory bowel disease. J Clin Immunol. 2010; 30:80–89.
Article21. Ahuja V, Subodh S, Tuteja A, et al. Genome-wide gene expression analysis for target genes to differentiate patients with intestinal tuberculosis and Crohn’s disease and discriminative value of FOXP3 mRNA expression. Gastroenterol Rep (Oxf). 2016; 4:59–67.
Article22. Sharma PK, Saha PK, Singh A, Sharma SK, Ghosh B, Mitra DK. FoxP3+ regulatory T cells suppress effector T-cell function at pathologic site in military tuberculosis. Am J Respir Crit Care Med. 2009; 179:1061–1070.
Article23. Kedia S, Das P, Madhusudhan KS, et al. Differentiating Crohn’s disease from intestinal tuberculosis. World J Gastroenterol. 2019; 25:418–432.
Article24. Jung Y, Hwangbo Y, Yoon SM, et al. Predictive factors for differentiating between Crohn’s disease and intestinal tuberculosis in Koreans. Am J Gastroenterol. 2016; 111:1156–1164.
Article25. Limsrivilai J, Shreiner AB, Pongpaibul A, et al. Meta-analytic Bayesian model for differentiating intestinal tuberculosis from Crohn’s disease. Am J Gastroenterol. 2017; 112:415–427.
Article26. Kedia S, Madhusudhan KS, Sharma R, et al. Combination of increased visceral fat and long segment involvement: development and validation of an updated imaging marker for differentiating Crohn’s disease from intestinal tuberculosis. J Gastroenterol Hepatol. 2018; 33:1234–1241.
Article27. He Y, Zhu Z, Chen Y, et al. Development and validation of a novel diagnostic nomogram to differentiate between intestinal tuberculosis and Crohn’s disease: a 6-year prospective multicenter study. Am J Gastroenterol. 2019; 114:490–499.
Article28. Das K, Ghoshal UC, Dhali GK, Benjamin J, Ahuja V, Makharia GK. Crohn’s disease in India: a multicenter study from a country where tuberculosis is endemic. Dig Dis Sci. 2009; 54:1099–1107.
Article29. Sharma SK, Ryan H, Khaparde S, et al. Index-TB guidelines: guidelines on extrapulmonary tuberculosis for India. Indian J Med Res. 2017; 145:448–463.30. Makharia GK, Sachdev V, Gupta R, Lal S, Pandey RM. AntiSaccharomyces cerevisiae antibody does not differentiate between Crohn’s disease and intestinal tuberculosis. Dig Dis Sci. 2007; 52:33–39.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peripheral Generation of CD4+ CD25+ Foxp3+ Regulatory T Cells
- A Study on the Number of Circulating CD4+CD25+Foxp3+ Regulatory T Cells and CD4+CD25-Foxp3+ T Cells in Psoriasis
- Dynamic Frequency of Blood CD4+CD25+ Regulatory T Cells in Rats with Collagen-induced Arthritis
- Alteration of CD4+CD25+Foxp3+ T cell level in Kawasaki disease
- IL-4 Induces CD4+CD25+ Regulatory T Cells from CD4+CD25- T Cells in Peripheral Blood