J Korean Med Sci.
2021 Apr;36(13):e86. 10.3346/jkms.2021.36.e86.
Mortality and Morbidities according to Time of Birth in Extremely Low Birth Weight Infants
- Affiliations
-
- 1Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Stem Cell and Regenerative Medicine Institute, Samsung Medical Center, Seoul, Korea
- 3Department of Health Sciences and Technology, SAIHST, Sungkyunkwan University, Seoul, Korea
- KMID: 2514760
- DOI: http://doi.org/10.3346/jkms.2021.36.e86
Abstract
- Background
Although the overall quality of high-risk neonatal care has improved recently, there is still concern about a difference in the quality of care when comparing off-hour births and regular-hour births. Moreover, there are no data in Korea regarding the impact of time of birth on mortality and morbidities in preterm infants.
Methods
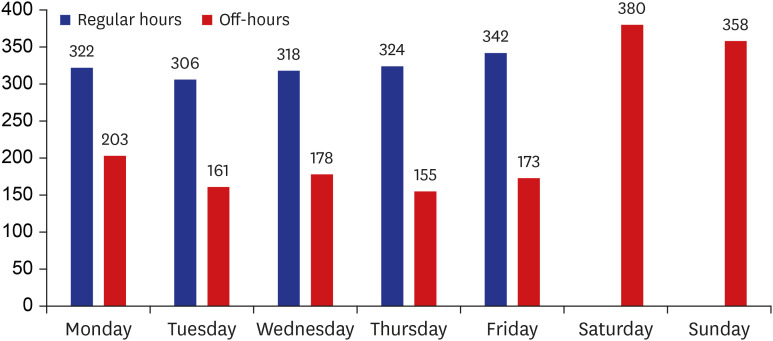
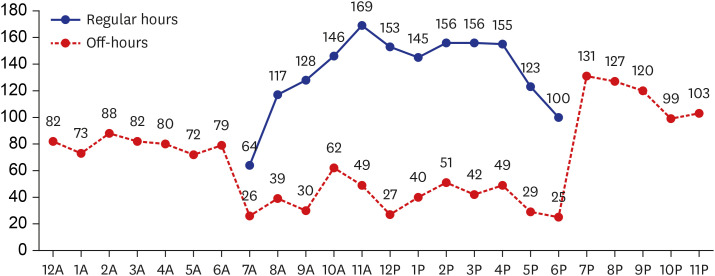
A total of 3,220 infants weighing < 1,000 g and born at 23–34 weeks in 2013–2017 were analyzed based on the Korean Neonatal Network data. Mortality and major morbidities were analyzed using logistic regression according to time of birth during off-hours (nighttime, weekend, and holiday) and regular hours. The institutes were sub-grouped into hospital group I and hospital group II based on the neonatal intensive care unit (NICU) care level defined by the mortality rates of < 50% and ≥ 50%, respectively, in infants born at 23–24 weeks' gestation.
Results
The number of births during regular hours and off-hours was similar. In the total population and hospital group I, off-hour births were not associated with increased neonatal mortality and morbidities. However, in hospital group II, increased early mortality was found in the off-hour births when compared to regular-hour births.
Conclusion
Efforts to improve the overall quality of NICU are required to lower the early mortality rate in off-hour births. Also, other sensitive indexes for the evaluation of quality of NICU care should be further studied.
Keyword
Figure
Reference
-
1. de Graaf JP, Ravelli AC, Visser GH, Hukkelhoven C, Tong WH, Bonsel GJ, et al. Increased adverse perinatal outcome of hospital delivery at night. BJOG. 2010; 117(9):1098–1107. PMID: 20497413.
Article2. Lee SK, Lee DS, Andrews WL, Baboolal R, Pendray M, Stewart S, et al. Higher mortality rates among inborn infants admitted to neonatal intensive care units at night. J Pediatr. 2003; 143(5):592–597. PMID: 14615728.
Article3. Abdel-Latif ME, Bajuk B, Oei J, Lui K. New South Wales and the Australian Capital Territory Neonatal Intensive Care Audit Group. Mortality and morbidities among very premature infants admitted after hours in an Australian neonatal intensive care unit network. Pediatrics. 2006; 117(5):1632–1639. PMID: 16651317.
Article4. Gould JB, Qin C, Chavez G. Time of birth and the risk of neonatal death. Obstet Gynecol. 2005; 106(2):352–358. PMID: 16055587.
Article5. Luo ZC, Karlberg J. Timing of birth and infant and early neonatal mortality in Sweden 1973–95: longitudinal birth register study. BMJ. 2001; 323(7325):1327–1330. PMID: 11739216.
Article6. Jensen EA, Lorch SA. Association between off-peak hour birth and neonatal morbidity and mortality among very low birth weight infants. J Pediatr. 2017; 186:41–48.e4. PMID: 28284476.
Article7. Gould JB, Qin C, Marks AR, Chavez G. Neonatal mortality in weekend vs weekday births. JAMA. 2003; 289(22):2958–2962. PMID: 12799403.
Article8. Pasupathy D, Wood AM, Pell JP, Fleming M, Smith GC. Time of birth and risk of neonatal death at term: retrospective cohort study. BMJ. 2010; 341:c3498. PMID: 20634347.
Article9. Stephansson O, Dickman PW, Johansson AL, Kieler H, Cnattingius S. Time of birth and risk of intrapartum and early neonatal death. Epidemiology. 2003; 14(2):218–222. PMID: 12606889.
Article10. Palmer WL, Bottle A, Aylin P. Association between day of delivery and obstetric outcomes: observational study. BMJ. 2015; 351:h5774. PMID: 26602245.
Article11. Mangold WD. Neonatal mortality by the day of the week in the 1974–75 Arkansas live birth cohort. Am J Public Health. 1981; 71(6):601–605. PMID: 7235098.
Article12. Mathers CD. Births and perinatal deaths in Australia: variations by day of week. J Epidemiol Community Health. 1983; 37(1):57–62. PMID: 6683744.
Article13. Kalogiannidis I, Margioula-Siarkou C, Petousis S, Goutzioulis M, Prapas N, Agorastos T. Infant births during the internal night are at increased risk for operative delivery and NICU admission. Arch Gynecol Obstet. 2011; 284(1):65–71. PMID: 20652279.
Article14. Lee SM, Chang YS, Park WS. Korean Neonatal Network. International perspectives: implementation of the Korean Neonatal Network. Neoreviews. 2019; 20(4):e177–88. PMID: 31261059.
Article15. Park JH, Chang YS, Sung S, Park WS. Korean Neonatal Network. Mortality rate-dependent variations in the timing and causes of death in extremely preterm infants born at 23–24 weeks' gestation. Pediatr Crit Care Med. 2019; 20(7):630–637. PMID: 31013260.
Article16. Kim JK, Chang YS, Sung S, Park WS. Mortality rate-dependent variations in the survival without major morbidities rate of extremely preterm infants. Sci Rep. 2019; 9(1):7371. PMID: 31089251.
Article17. Bell MJ, Ternberg JL, Feigin RD, Keating JP, Marshall R, Barton L, et al. Neonatal necrotizing enterocolitis. Therapeutic decisions based upon clinical staging. Ann Surg. 1978; 187(1):1–7. PMID: 413500.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study of Prematurity and Low Birth Weight Infants
- Clinical and Statistical Observation for Low Birth Weight Infants
- Hypoalbuminemia in Extremely Low Birth Weight Infants
- Changes in birth rates of low birth weight and premature infants in Korea over the past 7 years
- Fluconazole prophylaxis against invasive candidiasis in very low and extremely low birth weight preterm neonates: a systematic review and meta-analysis