J Korean Neurosurg Soc.
2021 Mar;64(2):143-150. 10.3340/jkns.2020.0124.
Intraoperative Neurophysiology Monitoring for Spinal Dysraphism
- Affiliations
-
- 1Department of Rehabilitation Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2513847
- DOI: http://doi.org/10.3340/jkns.2020.0124
Abstract
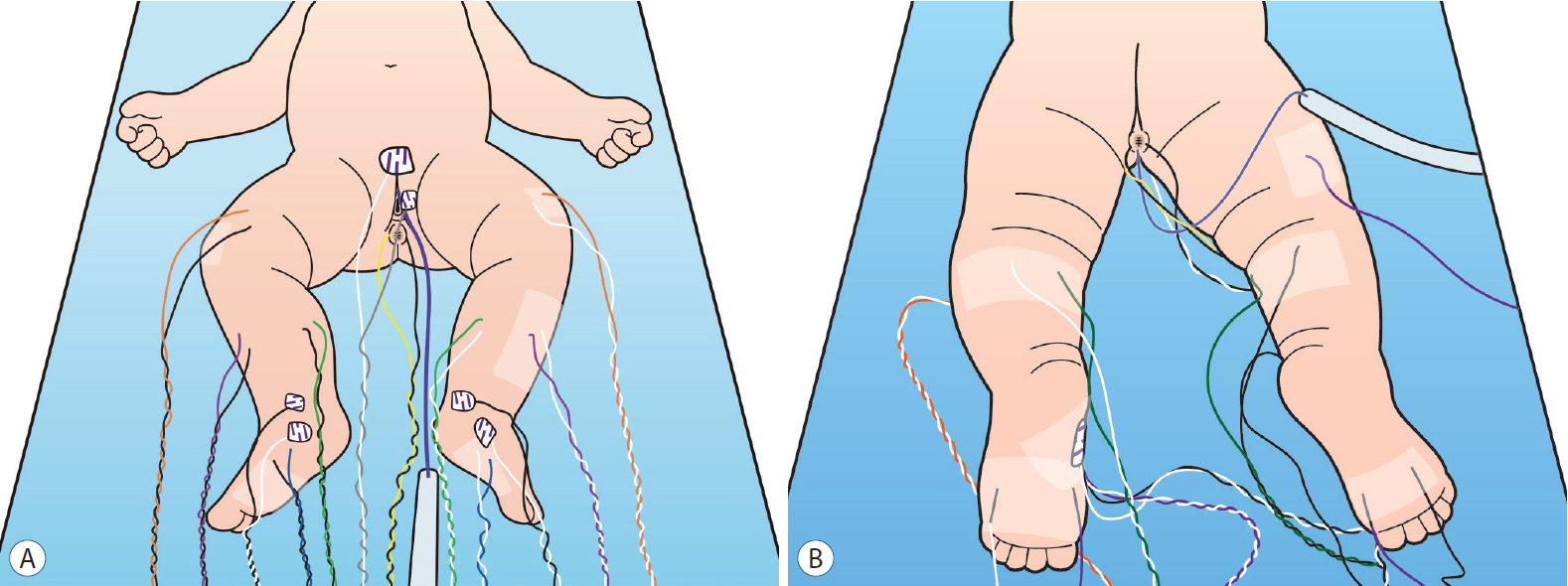
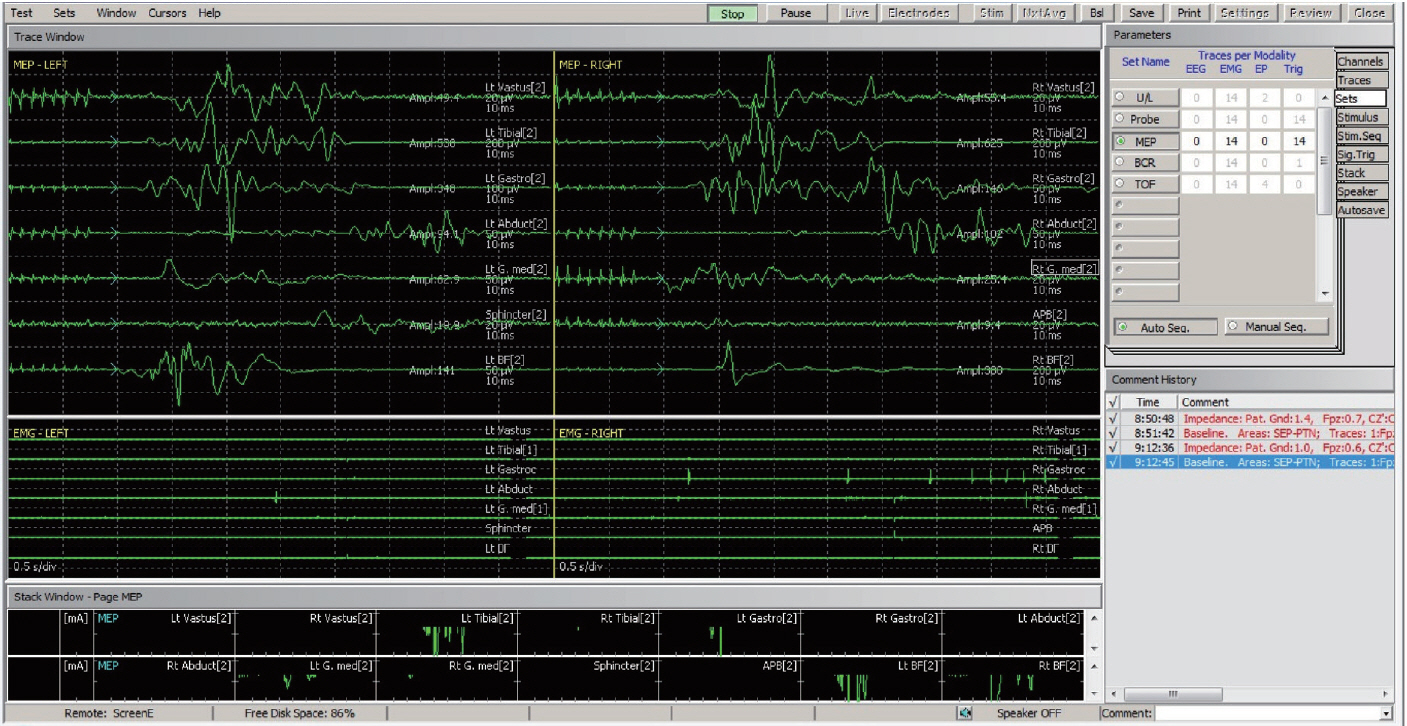
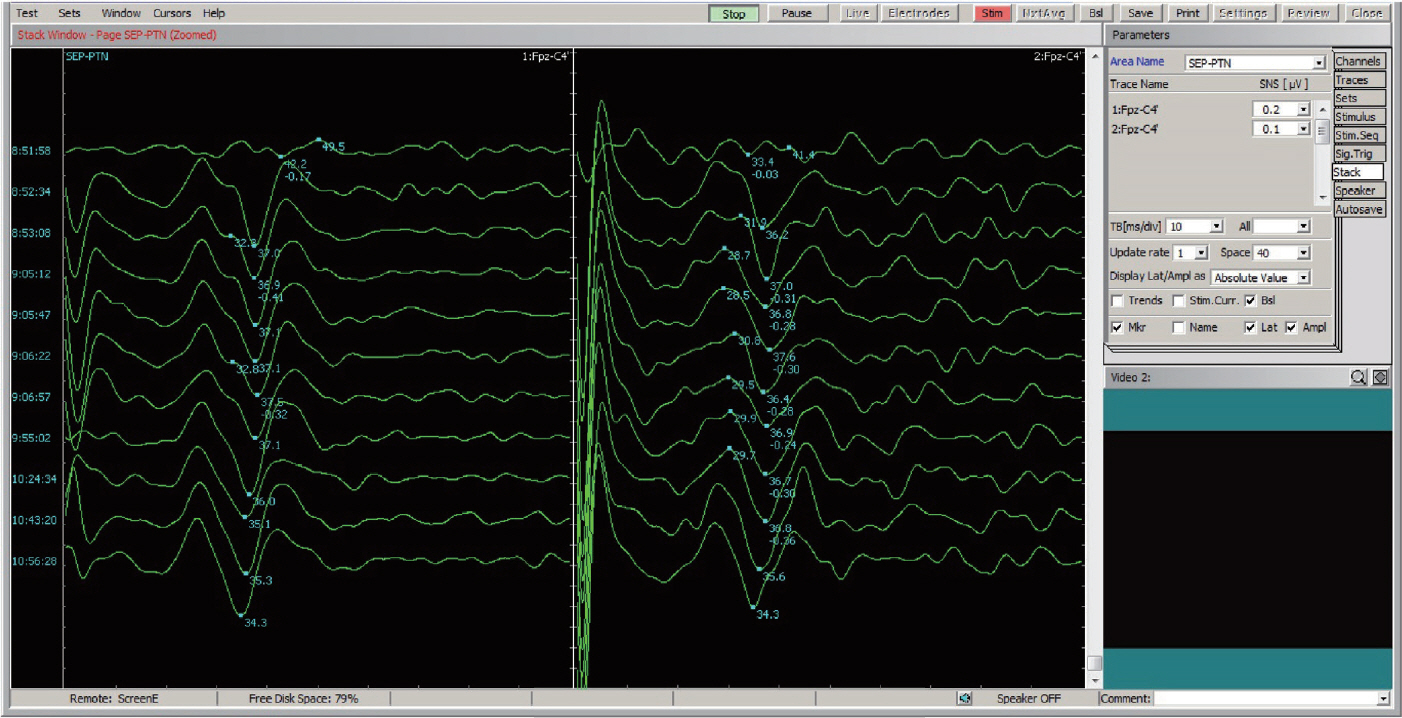
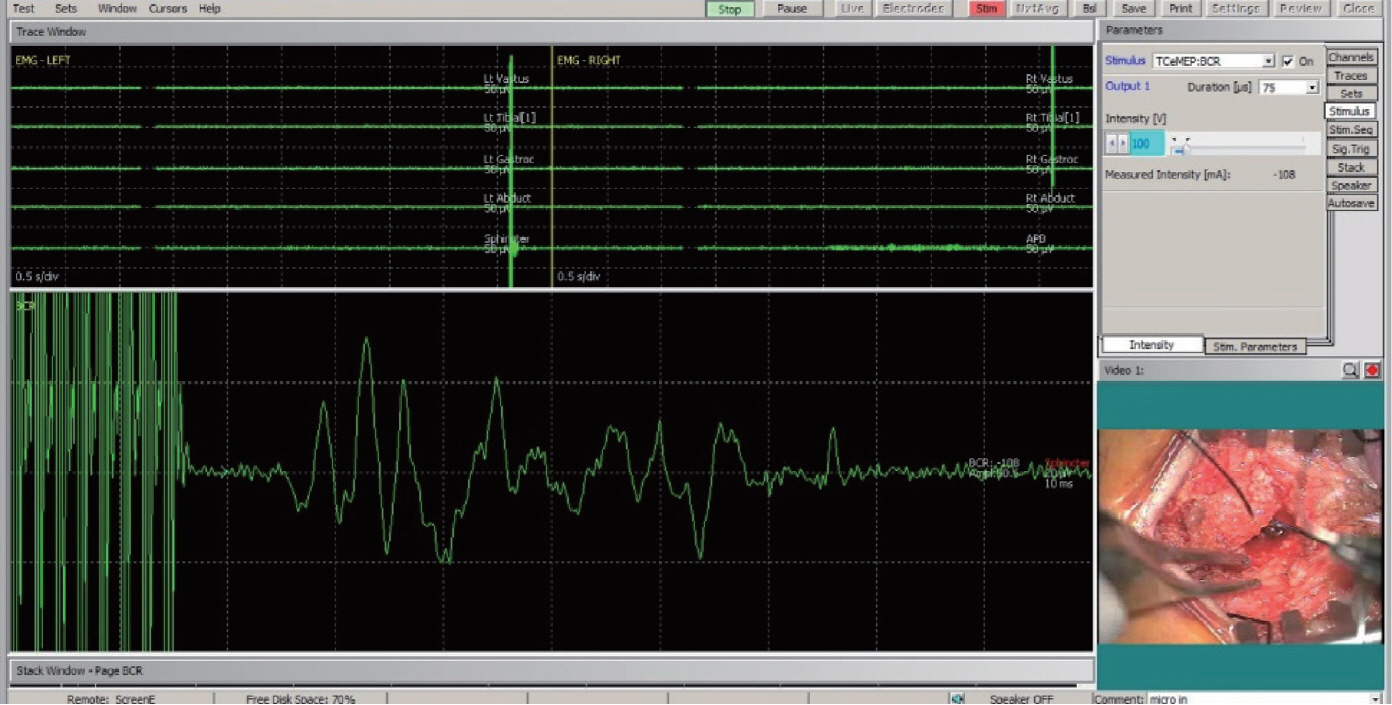
- Spinal dysraphism often causes neurological impairment from direct involvement of lesions or from cord tethering. The conus medullaris and lumbosacral roots are most vulnerable. Surgical intervention such as untethering surgery is indicated to minimize or prevent further neurological deficits. Because untethering surgery itself imposes risk of neural injury, intraoperative neurophysiological monitoring (IONM) is indicated to help surgeons to be guided during surgery and to improve functional outcome. Monitoring of electromyography (EMG), motor evoked potential, and bulbocavernosus reflex (BCR) is essential modalities in IONM for untethering. Sensory evoked potential can be also employed to further interpretation. In specific, free-running EMG and triggered EMG is of most utility to identify lumbosacral roots within the field of surgery and filum terminale or non-functioning cord can be also confirmed by absence of responses at higher intensity of stimulation. The sacral nervous system should be vigilantly monitored as pathophysiology of tethered cord syndrome affects the sacral function most and earliest. BCR monitoring can be readily applicable for sacral monitoring and has been shown to be useful for prediction of postoperative sacral dysfunction. Further research is guaranteed because current IONM methodology in spinal dysraphism is still deficient of quantitative and objective evaluation and fails to directly measure the sacral autonomic nervous system.
Figure
Reference
-
References
1. Albright AL, Pollack IF, Adelson PD, Solot JJ. Outcome data and analysis in pediatric neurosurgery. Neurosurgery. 45:101–106. 1999.
Article2. Cha S, Wang KC, Park K, Shin HI, Lee JY, Chong S, et al. Predictive value of intraoperative bulbocavernosus reflex during untethering surgery for post-operative voiding function. Clin Neurophysiol. 129:2594–2601. 2018.
Article3. Deletis V, Vodusek DB. Intraoperative recording of the bulbocavernosus reflex. Neurosurgery. 40:88–93. discussion 92-93. 1997.
Article4. Deletis V, Vodusek DB, Abbott R, Epstein FJ, Turndorf H. Intraoperative monitoring of the dorsal sacral roots: minimizing the risk of iatrogenic micturition disorders. Neurosurgery. 30:72–75. 1992.5. Hwang H, Wang KC, Bang MS, Shin HI, Kim SK, Phi JH, et al. Optimal stimulation parameters for intraoperative bulbocavernosus reflex in infants. J Neurosurg Pediatr. 20:464–470. 2017.
Article6. Journée HL, Polak HE, de Kleuver M. Influence of electrode impedance on threshold voltage for transcranial electrical stimulation in motor evoked potential monitoring. Med Biol Eng Comput. 42:557–561. 2004.
Article7. Kothbauer KF, Novak K. Intraoperative monitoring for tethered cord surgery: an update. Neurosurg Focus. 16:E8. 2004.
Article8. Krassioukov AV, Sarjeant R, Arkia H, Fehlings MG. Multimodality intraoperative monitoring during complex lumbosacral procedures: indications, techniques, and long-term follow-up review of 61 consecutive cases. J Neurosurg Spine. 1:243–253. 2004.
Article9. McLone DG. Occult dysraphism and the tethered spinal cord lipomas. In : Choix M, Di Rocco C, Hockley A, editors. Pediatric Neurosurgery. Philadelphia: Churchill Livingstone;1999. p. 61–78.10. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode: part I-surgical technique. Neurosurgery. 65:511–528. 2009.11. Pang D, Zovickian J, Oviedo A. Long-term outcome of total and near-total resection of spinal cord lipomas and radical reconstruction of the neural placode, part II: outcome analysis and preoperative profiling. Neurosurgery. 66:253–272. 2010.12. Prell J, Rampp S, Romstöck J, Fahlbusch R, Strauss C. Train time as a quantitative electromyographic parameter for facial nerve function in patients undergoing surgery for vestibular schwannoma. J Neurosurg. 106:826–832. 2007.
Article13. Quiñones-Hinojosa A, Gadkary CA, Gulati M, Von Koch CS, Lyon R, Weinstein PR, et al. Neurophysiological monitoring for safe surgical tethered cord syndrome release in adults. Surg Neurol. 62:127–133. 2004.
Article14. Ryken T, Menezes A. Intraoperative electrical and manometric monitoring in lumbosacral surgery. In : Loftus CM, Traynelis VC, editors. Intraoperative Monitoring Techniques in Neurosurgery. New York: McGraw-Hill;1994. p. 257–268.15. Shinomiya K, Fuchioka M, Matsuoka T, Okamoto A, Yoshida H, Mutoh N, et al. Intraoperative monitoring for tethered spinal cord syndrome. Spine (Phila Pa 1976). 16:1290–1294. 1991.
Article16. Song WH, Park JH, Tae BS, Kim SM, Hur M, Seo JH, et al. Establishment of novel intraoperative monitoring and mapping method for the cavernous nerve during robot-assisted radical prostatectomy: results of the phase I/II, first-in-human, feasibility study. Eur Urol. 78:221–228. 2020.
Article17. Tanaka Y, Kawaguchi M, Noguchi Y, Yoshitani K, Kawamata M, Masui K, et al. Systematic review of motor evoked potentials monitoring during thoracic and thoracoabdominal aortic aneurysm open repair surgery: a diagnostic meta-analysis. J Anesth. 30:1037–1050. 2016.
Article18. Von Koch CS, Quinones-Hinojosa A, Gulati M, Lyon R, Peacock WJ, Yingling CD. Clinical outcome in children undergoing tethered cord release utilizing intraoperative neurophysiological monitoring. Pediatr Neurosurg. 37:81–86. 2002.
Article19. Yamada S, Won DJ, Yamada SM. Pathophysiology of tethered cord syndrome: correlation with symptomatology. Neurosurg Focus. 16:E6. 2004.
Article20. Yamada S, Zinke DE, Sanders D. Pathophysiology of “tethered cord syndrome”. J Neurosurg. 54:494–503. 1981.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spinal Dysraphism in the Last Two Decades : What I Have Seen during the Era of Dynamic Advancement
- Intraoperative Monitoring for Tethered Cord Syndrome Using Somatosensory Evoked Potential and Motor Evoked Potential: Report of three cases
- Intramedullary Spinal Cord Lipoma without Spinal Dysraphism
- Spinal Dysraphism and Tethered Cord Syndrome
- Enlargement of Extraspinal Cysts in Spinal Dysraphism : A Reason for Early Untethering