J Korean Neurosurg Soc.
2020 May;63(3):342-345. 10.3340/jkns.2020.0094.
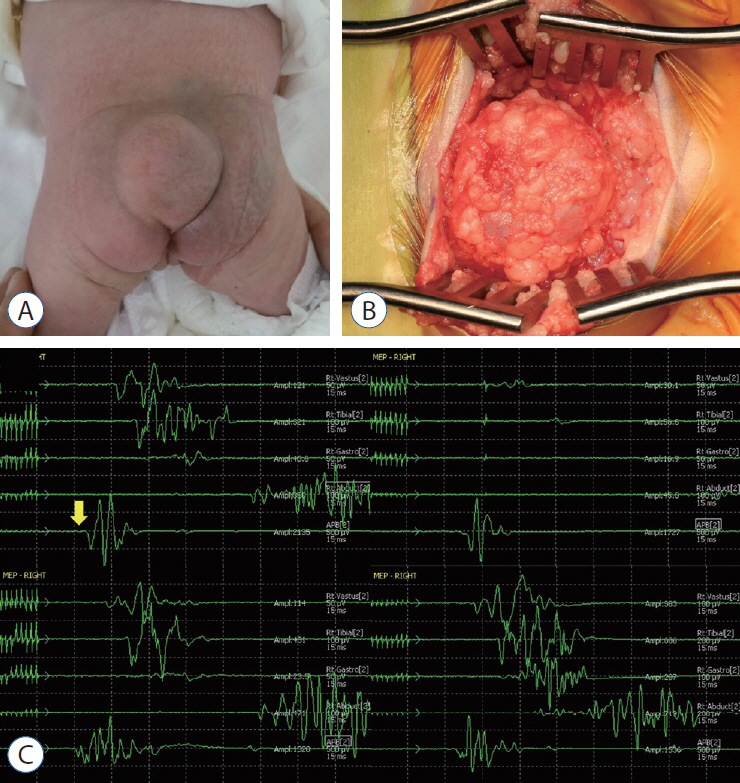
Enlargement of Extraspinal Cysts in Spinal Dysraphism : A Reason for Early Untethering
- Affiliations
-
- 1Division of Pediatric Neurosurgery, Seoul National University Children's Hospital, Seoul, Korea
- 2Department of Anatomy and Cell Biology, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2501721
- DOI: http://doi.org/10.3340/jkns.2020.0094
Abstract
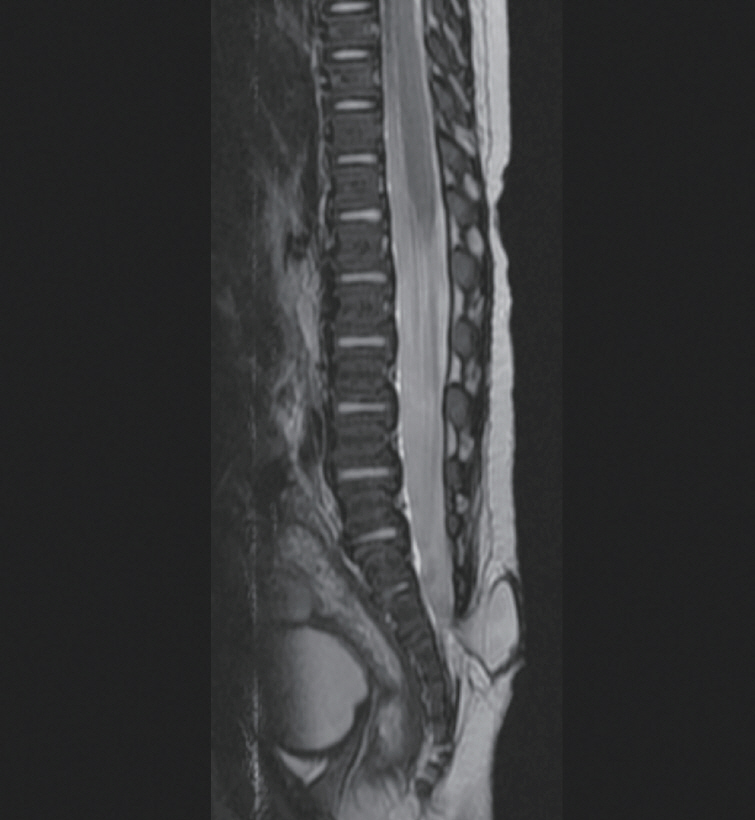
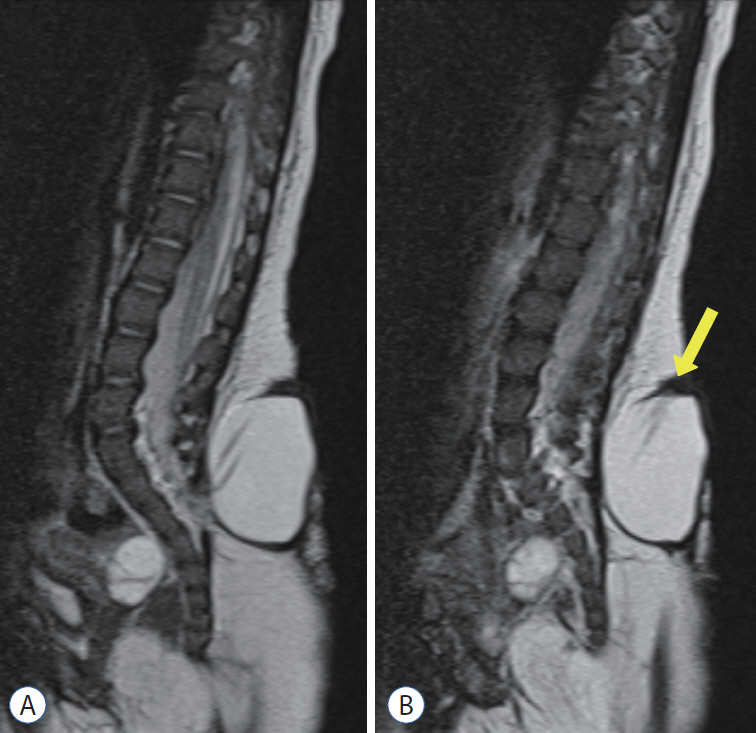
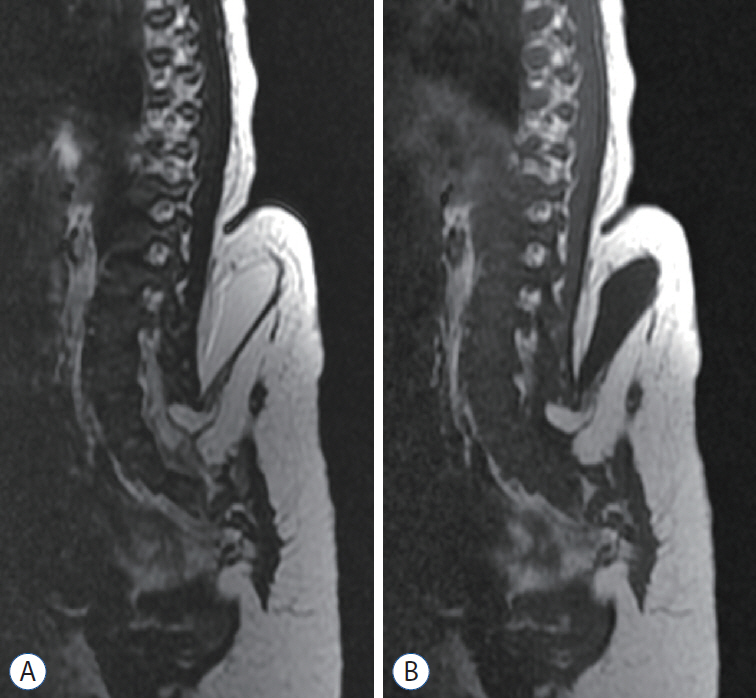
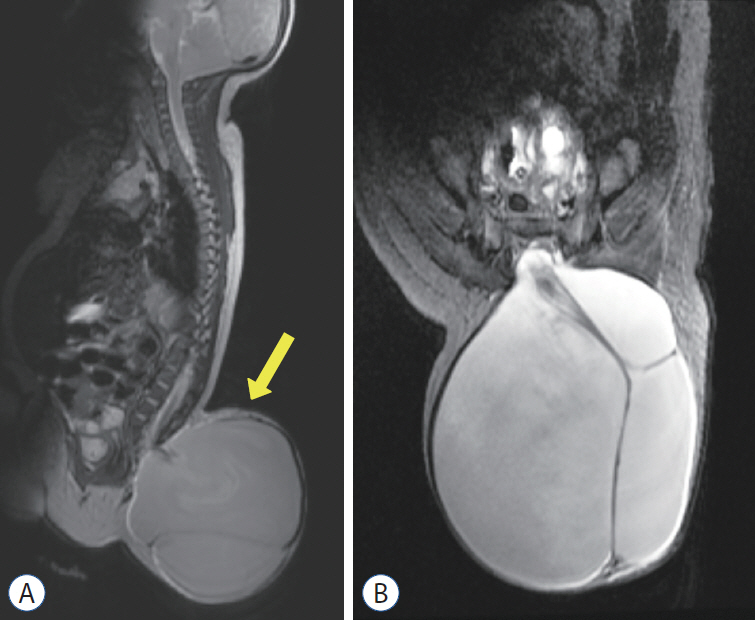
- Some types of spinal dysraphism can be accompanied by extraspinal cysts, including myelomeningocele, myelocystocele, myelocele, meningocele, limited dorsal myeloschisis, lipomyelomeningocele, and terminal myelocystocele. Each disease is classified according to the developmental mechanism, embryologic process, site of occurrence, or internal structure of the extraspinal cyst. In most cystic spinal dysraphisms except meningocele, part of the spinal cord is attached to the cyst dome. Most open spinal dysraphisms pose a risk of infection and require urgent surgical intervention, but when the cyst is accompanied by closed spinal dysraphism, the timing of surgery may vary. However, if the extraspinal cyst grows, it aggravates tethering by pulling the tip of the cord, which is attached to the dome of the cyst. This causes neurological deficits, so urgent surgery is required to release the tethered cord.
Keyword
Figure
Cited by 1 articles
-
Disorders of Secondary Neurulation : Mainly Focused on Pathoembryogenesis
Jeyul Yang, Ji Yeoun Lee, Kyung Hyun Kim, Kyu-Chang Wang
J Korean Neurosurg Soc. 2021;64(3):386-405. doi: 10.3340/jkns.2021.0023.
Reference
-
References
1. Gupta DK, Mahapatra AK. Terminal myelocystoceles: a series of 17 cases. J Neurosurg. 103(4 Suppl):344–352. 2005.
Article2. Kim KH, Chong S, Lee JY, Kim K, Kim SK, Wang KC. Decreased MEPs during subcutaneous dissection for untethering surgery of a "true" lipomyelomeningocele: aggravated traction of the spinal cord by release of the sac from the original nest. Childs Nerv Syst. 35:529–533. 2019.
Article3. Kumar R, Chandra A. Terminal myelocystocele. Indian J Pediatr. 69:1083–1086. 2002.
Article4. Lee JY, Phi JH, Kim SK, Cho BK, Wang KC. Urgent surgery is needed when cyst enlarges in terminal myelocystoceles. Childs Nerv Syst. 27:2149–2153. 2011.
Article5. McLone DG, Naidich TP. Terminal Myelocystocele. Neurosurgery. 16:36–43. 1985.
Article6. Morioka T, Hashiguchi K, Yoshida F, Matsumoto K, Miyagi Y, Nagata S, et al. Neurosurgical management of occult spinal dysraphism associated with OEIS complex. Childs Nerv Syst. 24:723–729. 2008.
Article7. Pang D, Zovickian J, Lee JY, Moes GS, Wang KC. Terminal myelocystocele: surgical observations and theory of embryogenesis. Neurosurgery. 70:1383–1405. discussion 1404-1405. 2012.8. Wataya T, Horikawa K, Kitagawa M, Tashiro Y. Thoracic meningocele in lumbo-costo-vertebral syndrome in a child: possible enlargement with repeated motion by anchoring to the diaphragm. J Neurosurg Pediatr. 18:183–186. 2016.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative Neurophysiology Monitoring for Spinal Dysraphism
- Intramedullary Spinal Cord Lipoma without Spinal Dysraphism
- Spinal Dysraphism and Tethered Cord Syndrome
- Multiple Lumbar Intradural Dermoid Cysts without Spinal Dysraphism
- Intraoperative Monitoring for Tethered Cord Syndrome Using Somatosensory Evoked Potential and Motor Evoked Potential: Report of three cases