Korean J Gastroenterol.
2021 Feb;77(2):71-76. 10.4166/kjg.2021.024.
Pharmacological Treatments of Esophageal Dysphagia
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2513416
- DOI: http://doi.org/10.4166/kjg.2021.024
Abstract
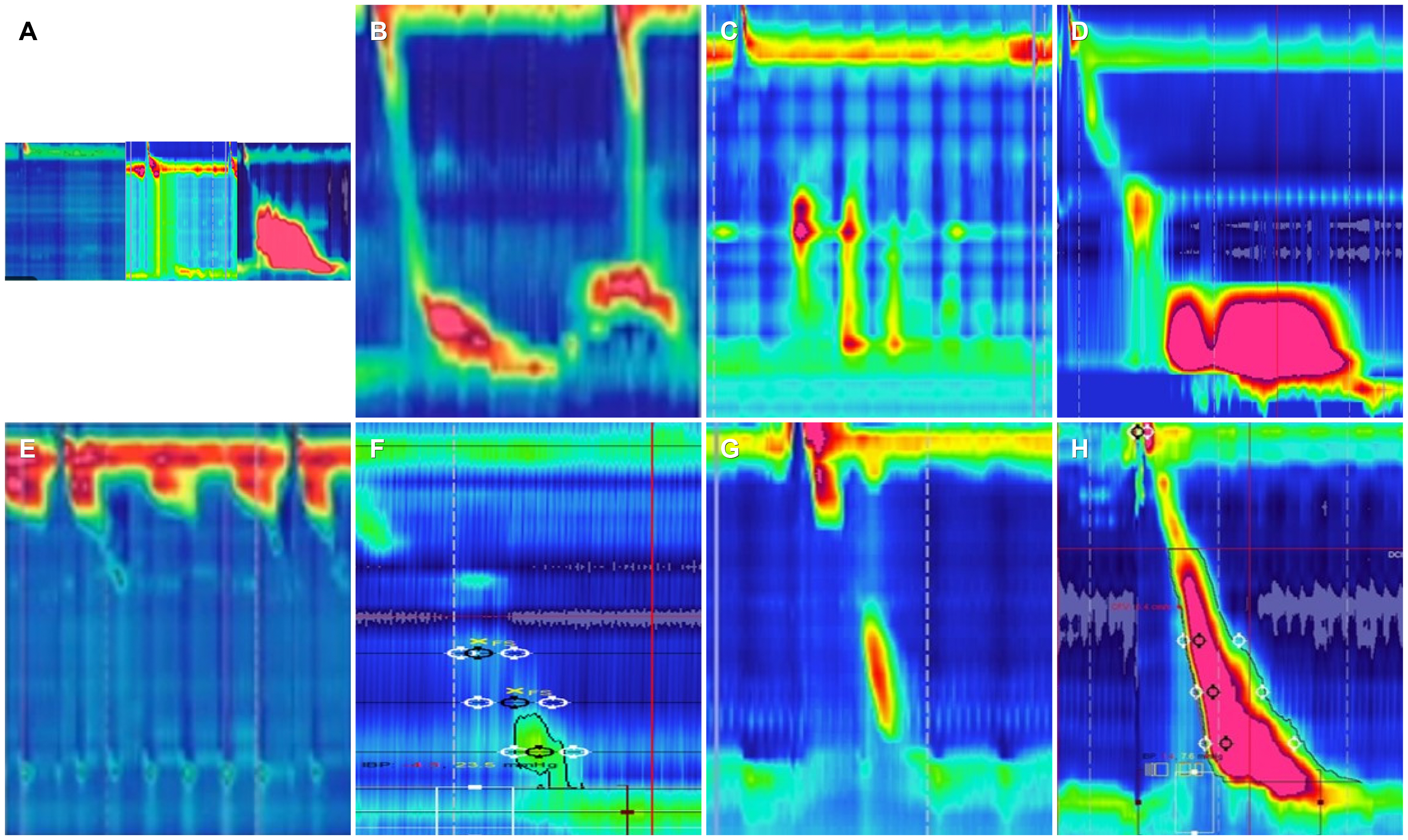
- Patients with esophageal dysphagia need a step-by-step approach for diagnosis and treatment. Endoscopic with biopsy and barium esophagogram are the essential tests evaluating anatomical abnormality and esophageal bolus stasis. Further imaging or esophageal function tests such as high-resolution esophageal manometry, functional endoluminal imaging probe, CT or endoscopic ultrasound are required. In the case of dysphagia due to esophageal motility disorder, whether it is the major motility disorder or minor motility disorder should be identified in high resolution manometry. Major motility disorders show esophagogastric junction obstruction or major peristaltic defects. In this case, the severity of the symptoms should be assessed and patients who need endoscopic or surgical treatment targeting lower esophageal sphincter should be screened. Impaired lower esophageal sphincter relaxation (achalasia, esophagogastric junction outflow obstruction, esophageal spasm or abnormal hypercontraction (jackhammer esophagus), hypotensive contraction (ineffective esophageal motility, failed peristalsis), esophageal hypersensitivity (noncardiac chest pain), gastroesophageal reflux disease and esophageal bolus stasis are the possible mechanisms causing dysphagia symptoms. The proper medical treatment depends on underlying mechanisms.
Keyword
Figure
Reference
-
1. Gyawali CP, Carlson DA, Chen JW, Patel A, Wong RJ, Yadlapati RH. 2020; ACG clinical guidelines: clinical use of esophageal physiologic testing. Am J Gastroenterol. 115:1412–1428. DOI: 10.14309/ajg.0000000000000734. PMID: 32769426.
Article2. Kahrilas PJ, Bredenoord AJ, Carlson DA, Pandolfino JE. 2018; Advances in management of esophageal motility disorders. Clin Gastroenterol Hepatol. 16:1692–1700. DOI: 10.1016/j.cgh.2018.04.026. PMID: 29702296. PMCID: PMC6317712.
Article3. Kahrilas PJ, Bredenoord AJ, Fox M, et al. 2015; The Chicago Classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 27:160–174. DOI: 10.1111/nmo.12477. PMID: 25469569. PMCID: PMC4308501.
Article4. Jung HK, Hong SJ, Lee OY, et al. 2020; 2019 Seoul consensus on esophageal achalasia guidelines. J Neurogastroenterol Motil. 26:180–203. DOI: 10.5056/jnm20014. PMID: 32235027. PMCID: PMC7176504.
Article5. Khalaf M, Chowdhary S, Elias PS, Castell D. 2018; Distal esophageal spasm: a review. Am J Med. 131:1034–1040. DOI: 10.1016/j.amjmed.2018.02.031. PMID: 29605413.
Article6. Roman S, Kahrilas PJ. 2013; Management of spastic disorders of the esophagus. Gastroenterol Clin North Am. 42:27–43. DOI: 10.1016/j.gtc.2012.11.002. PMID: 23452629. PMCID: PMC3618975.
Article7. Konturek JW, Gillessen A, Domschke W. 1995; Diffuse esophageal spasm: a malfunction that involves nitric oxide? Scand J Gastroenterol. 30:1041–1045. DOI: 10.3109/00365529509101604. PMID: 8578161.
Article8. Orlando RC, Bozymski EM. 1973; Clinical and manometric effects of nitroglycerin in diffuse esophageal spasm. N Engl J Med. 289:23–25. DOI: 10.1056/NEJM197307052890106. PMID: 4196712.
Article9. Eherer AJ, Schwetz I, Hammer HF, et al. 2002; Effect of sildenafil on oesophageal motor function in healthy subjects and patients with oesophageal motor disorders. Gut. 50:758–764. DOI: 10.1136/gut.50.6.758. PMID: 12010875. PMCID: PMC1773249.
Article10. Kligler B, Chaudhary S. 2007; Peppermint oil. Am Fam Physician. 75:1027–1030. PMID: 17427617.11. Pimentel M, Bonorris GG, Chow EJ, Lin HC. 2001; Peppermint oil improves the manometric findings in diffuse esophageal spasm. J Clin Gastroenterol. 33:27–31. DOI: 10.1097/00004836-200107000-00007. PMID: 11418786.
Article12. Khalaf MHG, Chowdhary S, Elmunzer BJ, Elias PS, Castell D. 2019; Impact of peppermint therapy on dysphagia and non-cardiac chest pain: a pilot study. Dig Dis Sci. 64:2214–2218. DOI: 10.1007/s10620-019-05523-8. PMID: 30771044.
Article13. Cannon RO 3rd, Quyyumi AA, Mincemoyer R, et al. 1994; Imipramine in patients with chest pain despite normal coronary angiograms. N Engl J Med. 330:1411–1417. DOI: 10.1056/NEJM199405193302003. PMID: 8159194.
Article14. Clouse RE, Lustman PJ, Eckert TC, Ferney DM, Griffith LS. 1987; Low-dose trazodone for symptomatic patients with esophageal contraction abnormalities. A double-blind, placebo-controlled trial. Gastroenterology. 92:1027–1036. DOI: 10.1016/0016-5085(87)90979-6. PMID: 3549420.15. Achem SR. 2007; Management of esophageal chest pain. Gastroenterol Hepatol (N Y). 3:765–767. PMID: 21960783. PMCID: PMC3104155.16. Hoogerwerf WA, Pasricha PJ, Thosani N, et al. 2001; Pharmacologic therapy in treating achalasia. Gastrointest Endosc Clin N Am. 11:311–324. vii. PMID: 11319064.
Article17. Vaezi MF, Pandolfino JE, Yadlapati RH, Greer KB, Kavitt RT. 2020; ACG clinical guidelines: diagnosis and management of achalasia. Am J Gastroenterol. 115:1393–1411. DOI: 10.14309/ajg.0000000000000731. PMID: 32773454.
Article18. Annese V, Bassotti G, Coccia G, et al. 2000; A multicentre randomised study of intrasphincteric botulinum toxin in patients with oesophageal achalasia. GISMAD Achalasia Study Group. Gut. 46:597–600. DOI: 10.1136/gut.46.5.597. PMID: 10764700. PMCID: PMC1727941.19. Friedenberg F, Gollamudi S, Parkman HP. 2004; The use of botulinum toxin for the treatment of gastrointestinal motility disorders. Dig Dis Sci. 49:165–175. DOI: 10.1023/B:DDAS.0000017434.53075.80. PMID: 15104353.20. Ren LH, Chen WX, Qian LJ, Li S, Gu M, Shi RH. 2014; Addition of prokinetics to PPI therapy in gastroesophageal reflux disease: a meta-analysis. World J Gastroenterol. 20:2412–2419. DOI: 10.3748/wjg.v20.i9.2412. PMID: 24605040. PMCID: PMC3942846.
Article