Neurointervention.
2021 Mar;16(1):52-58. 10.5469/neuroint.2020.00381.
Trends in Utilization of Preoperative Embolization for Spinal Metastases: A Study of the National Inpatient Sample 2005–2017
- Affiliations
-
- 1Mayo Clinic Neuro-Informatics Laboratory, Department of Neurologic Surgery, Mayo Clinic, Rochester, MN, USA
- 2Department of Neurologic Surgery, Mayo Clinic, Rochester, MN, USA
- 3Dr. Kiran C. Patel College of Allopathic Medicine, Nova Southeastern University, Davie, FL, USA
- 4Department of Neuroscience, University of Minnesota, Minneapolis, MN, USA
- 5Department of Radiology, Mayo Clinic, Rochester, MN, USA
- KMID: 2513344
- DOI: http://doi.org/10.5469/neuroint.2020.00381
Abstract
- Purpose
While previous studies have suggested that preoperative embolization of hypervascular spinal metastases may alleviate intraoperative blood loss and improve resectability, trends and driving factors for choosing this approach have not been extensively explored. Therefore, we evaluated the trends and assessed the factors associated with preoperative embolization utilization for spinal metastatic tumors using a national inpatient database.
Materials and Methods
The National Inpatient Sample database of the Healthcare Cost and Utilization Project was queried for patients undergoing surgical resection for spinal metastasis between January 1, 2005 and December 31, 2017. Patients undergoing preoperative embolization were identified; trends in the utilization of preoperative embolization were analyzed using the Cochran-Armitage test. Multivariable regression was conducted to assess factors associated with higher preoperative embolization utilization.
Results
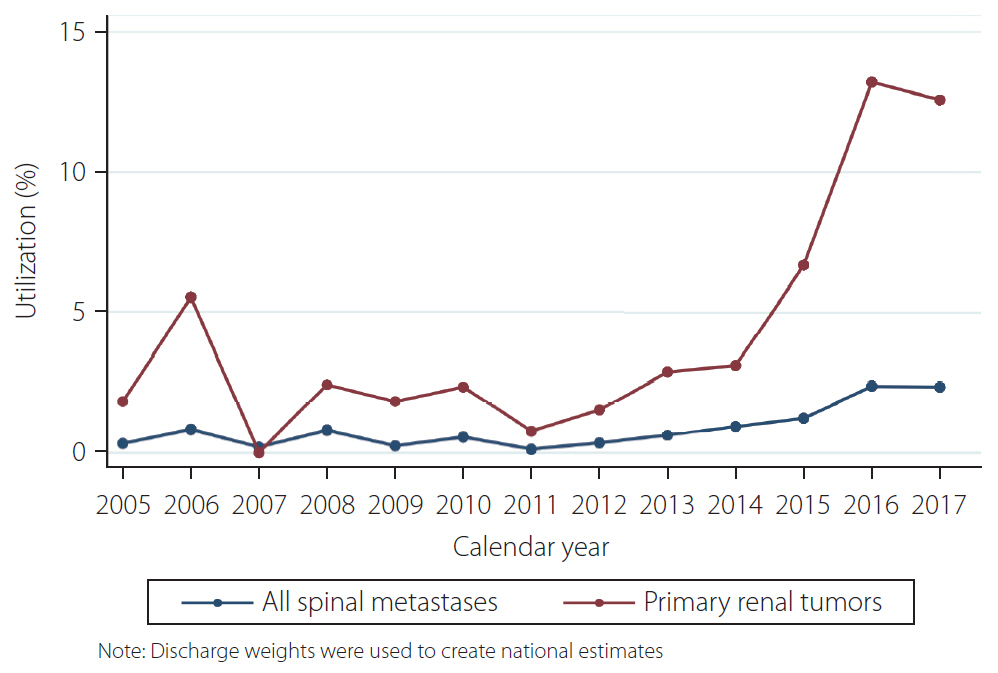
A total of 11,508 patients with spinal metastasis were identified; 105 (0.91%) underwent preoperative embolization. Of those 105 patients, 79 (75.24%) patients had a primary renal cancer, as compared to 1,732 (15.19%) of those who did not undergo preoperative embolization (P<0.001). The majority of patients in the non-preoperative embolization cohort had a primary lung tumor (n=3,562, 31.24%). Additionally, patient comorbidities were similar among the 2 groups (P>0.05). Trends in preoperative embolization indicated an increase of 0.16% (standard error: 0.024%, P<0.001) in utilization per year.
Conclusion
Utilization of preoperative embolization for spinal metastasis is increasing yearly, especially for patients with renal cancer, suggesting that surgeons may increasingly consider embolization before surgical resection for hypervascular tumors. Additionally, the literature has shown the intraoperative and postoperative benefits of this procedure.
Keyword
Figure
Reference
-
1. Prince EA, Ahn SH. Interventional management of vertebral body metastases. Semin Intervent Radiol. 2013; 30:278–281.
Article2. Djindjian R, Houdart R, Rey A. [Place of embolization in the investigation and therapy of cerebral and spinal malformations and vascular tumors. (Apropos of 50 cases)]. Ann Med Interne (Paris). 1973; 124:365–375. French.3. Luksanapruksa P, Buchowski JM, Tongsai S, Singhatanadgige W, Jennings JW. Systematic review and meta-analysis of effectiveness of preoperative embolization in surgery for metastatic spine disease. J Neurointerv Surg. 2018; 10:596–601.
Article4. Clausen C, Dahl B, Frevert SC, Hansen LV, Nielsen MB, Lönn L. Preoperative embolization in surgical treatment of spinal metastases: single-blind, randomized controlled clinical trial of efficacy in decreasing intraoperative blood loss. J Vasc Interv Radiol. 2015; 26:402–412. e1.
Article5. NIS overview [Internet]. Rockville: Agency for Healthcare Research and Quality;[cited 2020 May 2]. Available from: https://www.hcup-us.ahrq.gov/nisoverview.jsp.6. Malik AT, Baek J, Alexander JH, Khan SN, Scharschmidt TJ. Orthopaedic vs. neurosurgery - does a surgeon’s specialty have an influence on 90-day complications following surgical intervention of spinal metastases? Clin Neurol Neurosurg. 2020; 192:105735.
Article7. Kelly ML, Kshettry VR, Rosenbaum BP, Seicean A, Weil RJ. Effect of a randomized controlled trial on the surgical treatment of spinal metastasis, 2000 through 2010: a population-based cohort study. Cancer. 2014; 120:901–908.
Article8. Patil CG, Lad SP, Santarelli J, Boakye M. National inpatient complications and outcomes after surgery for spinal metastasis from 1993-2002. Cancer. 2007; 110:625–630.
Article9. Brandel MG, Rennert RC, Wali AR, Santiago-Dieppa DR, Steinberg JA, Ramos C, et al. Impact of preoperative endovascular embolization on immediate meningioma resection outcomes. Neurosurg Focus. 2018; 44:E6.
Article10. Sideman M, Zwolak R. Coding for vascular and endovascular surgery. In : Savarise M, Senkowski C, editors. Principles of coding and reimbursement for surgeons. Cham: Springer;2017. p. 297–310.11. Trend weights for HCUP NIS data [Internet]. Rockville: Agency for Healthcare Research and Quality;[cited 2020 Jul 30]. Available from: https://www.hcup-us.ahrq.gov/db/nation/nis/trendwghts.jsp.12. Armitage P, Berry G, Matthews JNS. Statistical methods in medical research. 4th ed. Hoboken: John Wiley & Sons;2008.13. Awad AW, Almefty KK, Ducruet AF, Turner JD, Theodore N, McDougall CG, et al. The efficacy and risks of preoperative embolization of spinal tumors. J Neurointerv Surg. 2016; 8:859–864.
Article14. Griessenauer CJ, Salem M, Hendrix P, Foreman PM, Ogilvy CS, Thomas AJ. Preoperative embolization of spinal tumors: a systematic review and meta-analysis. World Neurosurg. 2016; 87:362–371.
Article15. Ozkan E, Gupta S. Embolization of spinal tumors: vascular anatomy, indications, and technique. Tech Vasc Interv Radiol. 2011; 14:129–140.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of Coinsurance Reduction Policy on Healthcare Utilization Among Children Under 15
- Corrigendum: Inpatient hypospadias care: Trends and outcomes from the American nationwide inpatient sample
- Current and Future Trends in Hospital Utilization of Patients With Schizophrenia in Korea: A Time Series Analysis Using National Health Insurance Data
- Inpatients hypospadias care: Trends and outcomes from the American nationwide inpatient sample
- Cancer Patients' Utilization of Tertiary Hospitals in Seoul Before and After the Benefit Expansion Policy