Korean J Urol.
2015 Aug;56(8):594-600. 10.4111/kju.2015.56.8.594.
Inpatients hypospadias care: Trends and outcomes from the American nationwide inpatient sample
- Affiliations
-
- 1Division of Urologic Surgery and Center for Surgery and Public Health, Brigham and Women's Hospital, Harvard Medical School, Boston, MA, USA. christian.p.meyer@googlemail.com
- 2Department of Urology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany.
- 3Vattikuti Urology Institute, Henry Ford Health System, Detroit, MI, USA.
- 4Department of Urology, Marienhospital Herne, Ruhr University Bochum, Bochum, Germany.
- 5Department of Urology, Children's Hospital of Michigan, Detroit, MI, USA.
- KMID: 2164411
- DOI: http://doi.org/10.4111/kju.2015.56.8.594
Abstract
- PURPOSE
Hypospadias is the most common congenital penile anomaly. Information about current utilization patterns of inpatient hypospadias repair as well as complication rates remain poorly evaluated.
MATERIALS AND METHODS
The Nationwide Inpatient Sample was used to identify all patients undergoing inpatient hypospadias repair between 1998 and 2010. Patient and hospital characteristics were attained and outcomes of interest included intra- and immediate postoperative complications. Utilization was evaluated temporally and also according to patient and hospital characteristics. Predictors of complications and excess length of stay were evaluated by logistic regression models.
RESULTS
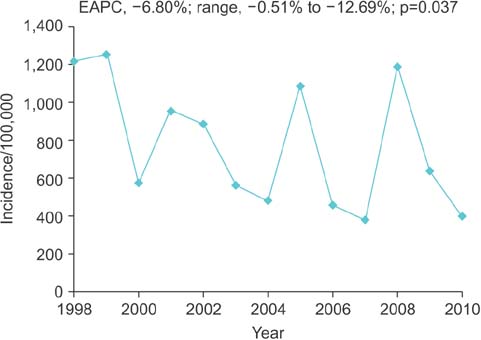
A weighted 10,201 patients underwent inpatient hypospadias repair between 1998 and 2010. Half were infants (52.2%), and were operated in urban and teaching hospitals. Trend analyses demonstrated a decline in incidence of inpatient hypospadias repair (estimated annual percentage change, -6.80%; range, -0.51% to -12.69%; p=0.037). Postoperative complication rate was 4.9% and most commonly wound-related. Hospital volume was inversely related to complication rates. Specifically, higher hospital volume (>31 cases annually) was the only variable associated with decreased postoperative complications.
CONCLUSIONS
Inpatient hypospadias repair have substantially decreased since the late 1990's. Older age groups and presumably more complex procedures constitute most of the inpatient procedures nowadays.
MeSH Terms
-
Adolescent
Adult
Age Distribution
Child
Child, Preschool
Hospitalization/statistics & numerical data/*trends
Humans
Hypospadias/epidemiology/*surgery
Infant
Length of Stay/statistics & numerical data/trends
Male
Outcome Assessment (Health Care)
Postoperative Complications/epidemiology
United States/epidemiology
Workload/statistics & numerical data
Young Adult
Figure
Reference
-
1. Pohl HG, Joyce GF, Wise M, Cilento BG Jr. Cryptorchidism and hypospadias. J Urol. 2007; 177:1646–1651.2. Nelson CP, Park JM, Wan J, Bloom DA, Dunn RL, Wei JT. The increasing incidence of congenital penile anomalies in the United States. J Urol. 2005; 174(4 Pt 2):1573–1576.3. Paulozzi LJ, Erickson JD, Jackson RJ. Hypospadias trends in two US surveillance systems. Pediatrics. 1997; 100:831–834.4. Korvald C, Stubberud K. High odds for freedom from early complications after tubularized incised-plate urethroplasty in 1-year-old versus 5-year-old boys. J Pediatr Urol. 2008; 4:452–456.5. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.6. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992; 45:613–619.7. United States Census Bureau [Internet]. Washington, DC: United States Census Bureau;c2015. cited 2014 Aug 23. Available from: http://www.census.gov.8. Budaus L, Abdollah F, Sun M, Morgan M, Johal R, Thuret R, et al. Annual surgical caseload and open radical prostatectomy outcomes: improving temporal trends. J Urol. 2010; 184:2285–2290.9. Darling DA. The Kolmogorov-Smirnov, Cramer-Von Mises tests. Ann Math Stat. 1957; 28:823–838.10. Shapiro SS, Wilk MB. An analysis of variance test for normality (complete samples). Biometrika. 1965; 52:591–611.11. Anderson WF, Camargo MC, Fraumeni JF Jr, Correa P, Rosenberg PS, Rabkin CS. Age-specific trends in incidence of noncardia gastric cancer in US adults. JAMA. 2010; 303:1723–1728.12. Panageas KS, Schrag D, Riedel E, Bach PB, Begg CB. The effect of clustering of outcomes on the association of procedure volume and surgical outcomes. Ann Intern Med. 2003; 139:658–665.13. Borer JG, Bauer SB, Peters CA, Diamond DA, Atala A, Cilento BG Jr, et al. Tubularized incised plate urethroplasty: expanded use in primary and repeat surgery for hypospadias. J Urol. 2001; 165:581–585.14. Tekgul S, Riedmiller H, Dogan HS, Hoebeke P, Kocvara R, Nijman JM, et al. Guidelines on pediatric urology. Arnhem (NL): European Association of urology;2013.15. Springer A, Baskin LS. Timing of hypospadias repair in patients with disorders of sex development. Endocr Dev. 2014; 27:197–202.16. Lu W, Tao Y, Wisniewski AB, Frimberger D, Kropp BP. Different outcomes of hypospadias surgery between north america, europe and china: is patient age a factor? Nephrourol Mon. 2012; 4:609–612.17. Bush NC, Holzer M, Zhang S, Snodgrass W. Age does not impact risk for urethroplasty complications after tubularized incised plate repair of hypospadias in prepubertal boys. J Pediatr Urol. 2013; 9:252–256.18. Flick RP, Sprung J, Harrison TE, Gleich SJ, Schroeder DR, Hanson AC, et al. Perioperative cardiac arrests in children between 1988 and 2005 at a tertiary referral center: a study of 92,881 patients. Anesthesiology. 2007; 106:226–237.19. McCann ME, Schouten AN. Beyond survival; influences of blood pressure, cerebral perfusion and anesthesia on neurodevelopment. Paediatr Anaesth. 2014; 24:68–73.20. Barbagli G, Perovic S, Djinovic R, Sansalone S, Lazzeri M. Retrospective descriptive analysis of 1,176 patients with failed hypospadias repair. J Urol. 2010; 183:207–211.21. Lee OT, Durbin-Johnson B, Kurzrock EA. Predictors of secondary surgery after hypospadias repair: a population based analysis of 5,000 patients. J Urol. 2013; 190:251–255.22. Miller DC, Saigal CS, Litwin MS. The demographic burden of urologic diseases in America. Urol Clin North Am. 2009; 36:11–27.23. Perlmutter AE, Morabito R, Tarry WF. Impact of patient age on distal hypospadias repair: a surgical perspective. Urology. 2006; 68:648–651.24. Bhat A, Mandal AK. Acute postoperative complications of hypospadias repair. Indian J Urol. 2008; 24:241–248.25. Siu W, Daignault S, Miller DC, Dunn RL, Gilbert S, Weizer AZ, et al. Understanding differences between high and low volume hospitals for radical prostatectomy. Urol Oncol. 2008; 26:260–265.26. Kelley-Quon LI, Tseng CH, Jen HC, Shew SB. Hospital type predicts surgical complications for infants with hypertrophic pyloric stenosis. Am Surg. 2012; 78:1079–1082.27. Horowitz M, Salzhauer E. The 'learning curve' in hypospadias surgery. BJU Int. 2006; 97:593–596.28. Frimberger D, Campbell J, Kropp BP. Hypospadias outcome in the first 3 years after completing a pediatric urology fellowship. J Pediatr Urol. 2008; 4:270–274.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Corrigendum: Inpatient hypospadias care: Trends and outcomes from the American nationwide inpatient sample
- The Role of Educational Nurses in Inpatient Management for Diabetes Care: 2023 ADA Practice Guidelines
- An Inpatient Group Psychotherapy Model: Integrated Model led by A Psychiatrist
- Inpatient or outpatient total elbow arthroplasty: a comparison of patient populations and 30-day surgical outcomes from the American College of Surgeons National Surgical Quality Improvement Program
- Nationwide trends in stroke hospitalization over the past decade