Ann Hepatobiliary Pancreat Surg.
2021 Feb;25(1):112-121. 10.14701/ahbps.2021.25.1.112.
Standard and modified techniques for parenchyma-preserving hepatectomy focused on segments I+IV resection in patients with perihilar cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2513184
- DOI: http://doi.org/10.14701/ahbps.2021.25.1.112
Abstract
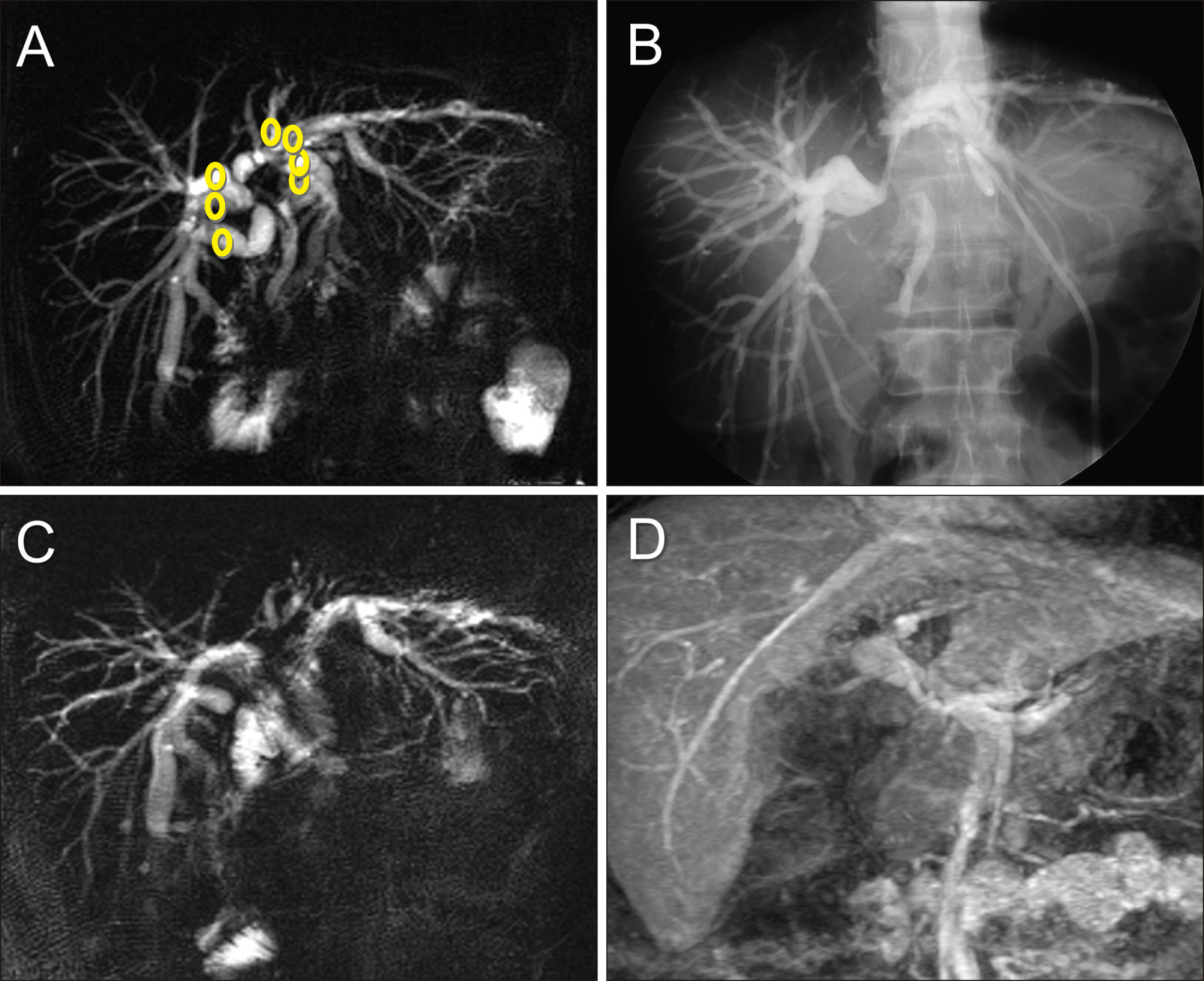
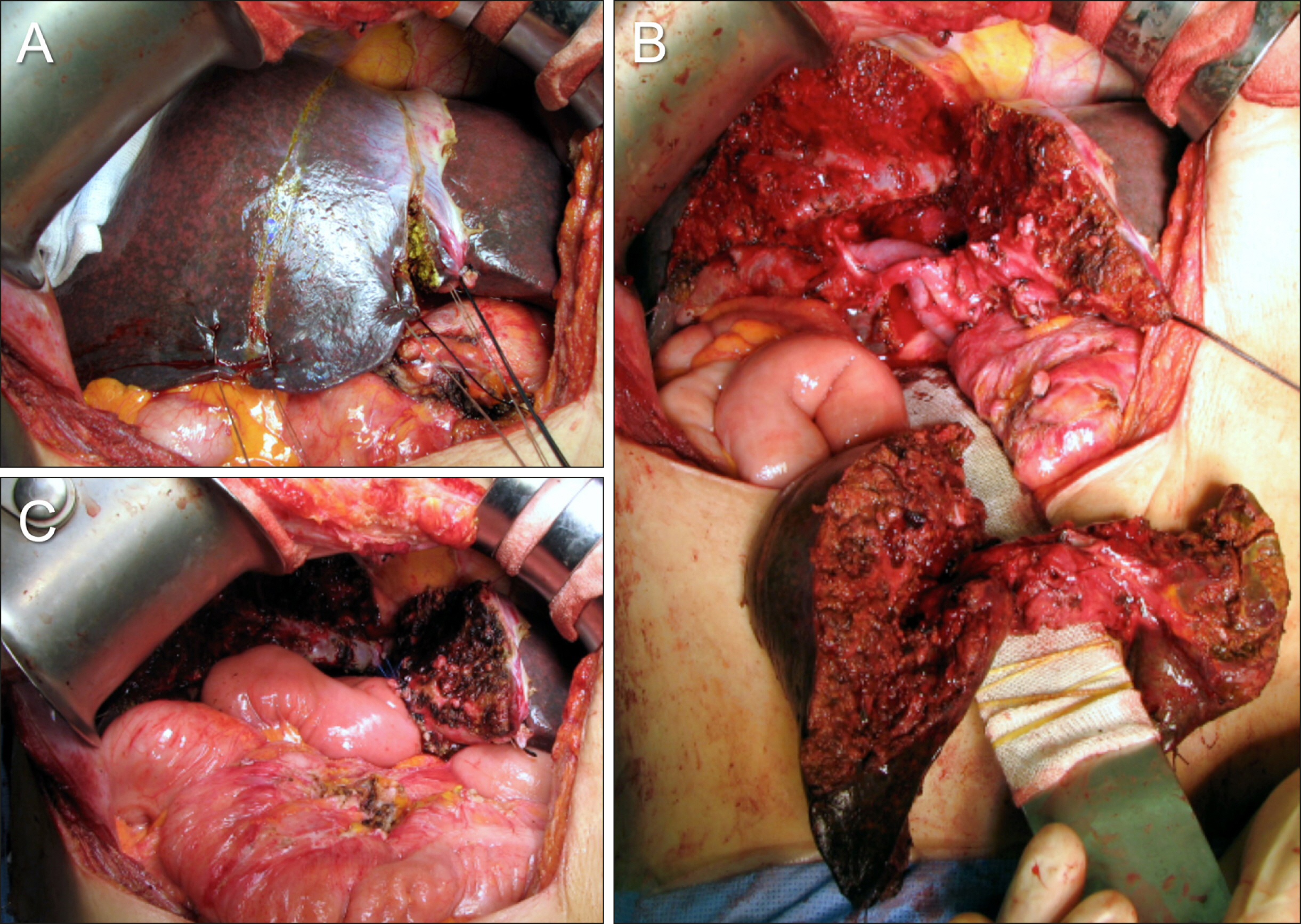
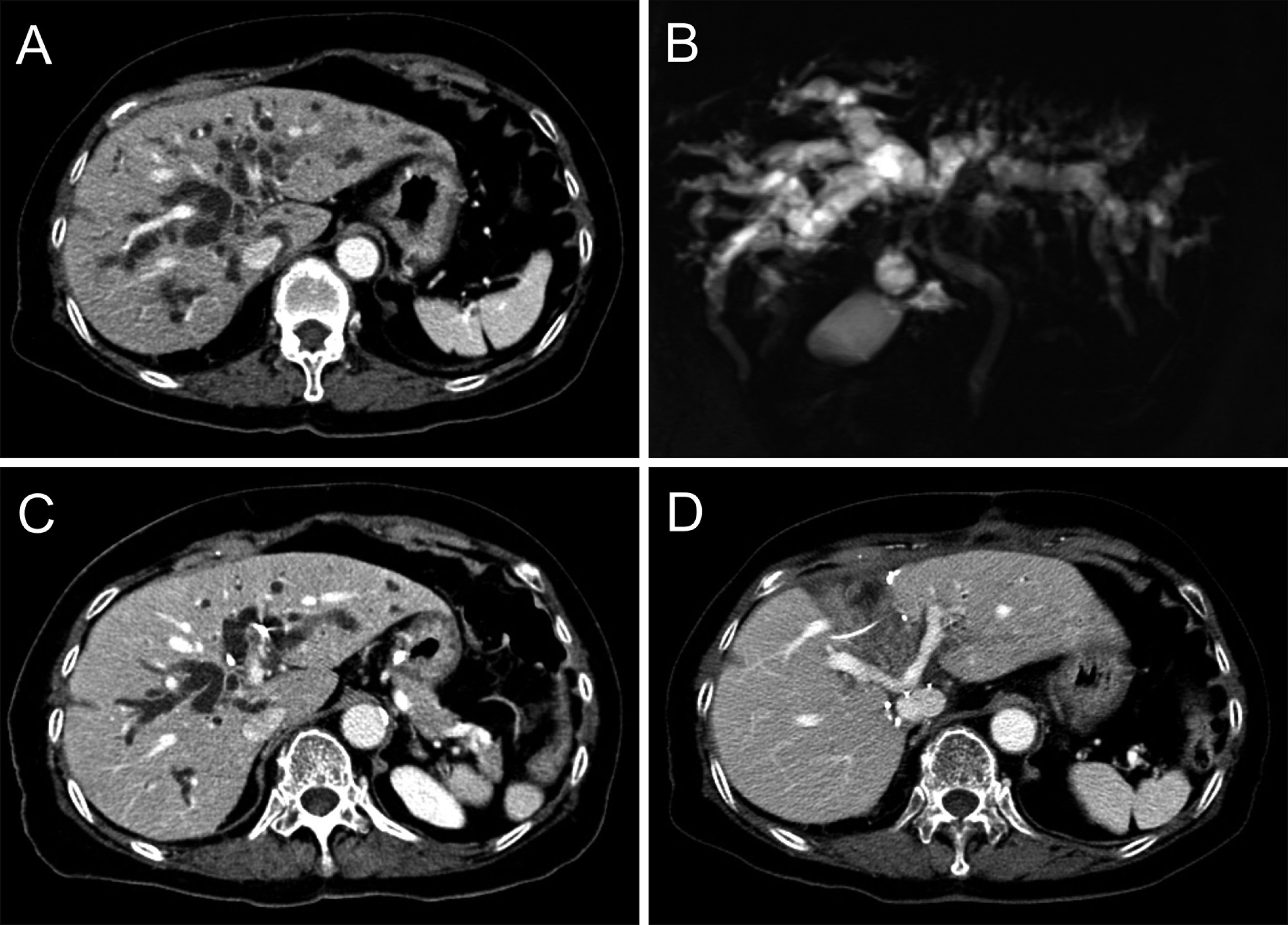
- Resection of the hepatic segments I+IV (S1+S4) is the most common type of parenchyma-preserving hepatectomy (PPH) for perihilar cholangiocarcinoma (PHCC). The author describes personal experience on the standard and modified techniques for PPH focused on S1+S4 resection in patients with PHCC. 1) Isolated caudate lobectomy with bile duct resection (BDR) is the minimal type of PPH, but not currently recommended due to technical difficulty. 2) Partial hepatectomy of S1+S4a±segment V (S5) with BDR provides wide operative field, but extension of BDR is limited and resection of S1 paracaval portion is still difficult. 3) Resection of S1+S4+S5 with BDR provides wider operative field for complete S1 resection and multiple biliary reconstruction. 4) Resection of S1+S4 with BDR offers very wide operative field and allows wider extent of hilar BDR, and thus presents the most common type of PPH. A supplementary video clip presents the detailed standard surgical procedure for resection of S1+S4 with BDR in a patient with type IIIA PHCC. 5) Modified resection of S1+S4±S5 or segment VIII (S8) with BDR facilitates additional resection of tumor-involved S5 or S8 ducts. 6) Major hilar vascular invasion is usually contraindicated for PPH and only small portal vein invasion requiring wedge resection and patch venoplasty is allowed. In conclusion, PPH can achieve curative resection and improved outcomes in patients with PHCC via reasonable modification of the extent of hepatectomy and hilar BDR. PPH may have advantages in selected patients depending on the extent of tumor, and in patients with high operative risk
Keyword
Figure
Cited by 1 articles
-
Intraductal tubulopapillary neoplasms of the pancreas and biliary tract: The black swan of hepatobiliary surgery
Jilyan Decker, Amanda Cavanaugh, Megan Brown, Saverio Ligato, Oscar Kenneth Serrano
Ann Hepatobiliary Pancreat Surg. 2021;25(4):556-561. doi: 10.14701/ahbps.2021.25.4.556.
Reference
-
1. Baer HU, Stain SC, Dennison AR, Eggers B, Blumgart LH. 1993; Improvements in survival by aggressive resections of hilar cholangiocarcinoma. Ann Surg. 217:20–27. DOI: 10.1097/00000658-199301000-00005. PMID: 8380975. PMCID: PMC1242729.
Article2. Childs T, Hart M. 1993; Aggressive surgical therapy for Klatskin tumors. Am J Surg. 165:554–557. DOI: 10.1016/S0002-9610(05)80433-7. PMID: 7683844.
Article3. Tsuzuki T, Ueda M, Kuramochi S, Iida S, Takahashi S, Iri H. 1990; Carcinoma of the main hepatic duct junction: indications, operative morbidity and mortality, and long-term survival. Surgery. 108:495–501. PMID: 2396193.4. Nimura Y, Hayakawa N, Kamiya J, Kondo S, Shionoya S. 1990; Hepatic segmentectomy with caudate lobe resection for bile duct carcinoma of the hepatic hilus. World J Surg. 14:535–543. discussion 544DOI: 10.1007/BF01658686. PMID: 2166381.
Article5. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, et al. 1998; Aggressive surgical approaches to hilar cholangiocarcinoma: hepatic or local resection? Surgery. 123:131–136. DOI: 10.1016/S0039-6060(98)70249-1. PMID: 9481397.
Article6. Iida S, Tsuzuki T, Ogata Y, Yoneyama K, Iri H, Watanabe K. 1987; The long-term survival of patients with carcinoma of the main hepatic duct junction. Cancer. 60:1612–1619. DOI: 10.1002/1097-0142(19871001)60:7<1612::AID-CNCR2820600732>3.0.CO;2-1. PMID: 3621131.
Article7. Hayashi S, Miyazaki M, Kondo Y, Nakajima N. 1994; Invasive growth patterns of hepatic hilar ductal carcinoma. A histologic analysis of 18 surgical cases. Cancer. 73:2922–2929. DOI: 10.1002/1097-0142(19940615)73:12<2922::AID-CNCR2820731208>3.0.CO;2-K. PMID: 8199989.
Article8. Blumgart LH, Hadjis NS, Benjamin IS, Beazley R. 1984; Surgical approaches to cholangiocarcinoma at confluence of hepatic ducts. Lancet. 1:66–70. DOI: 10.1016/S0140-6736(84)90002-3. PMID: 6197596.
Article9. Miyazaki M, Itoh H, Ambiru S, Shimizu H, Togawa A, Gohchi E, et al. 1996; Radical surgery for advanced gallbladder carcinoma. Br J Surg. 83:478–481. DOI: 10.1002/bjs.1800830413. PMID: 8665234.
Article10. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. 1999; Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. J Am Coll Surg. 189:575–583. DOI: 10.1016/S1072-7515(99)00219-7. PMID: 10589594.
Article11. Hwang S. Parenchyma-preserving hepatectomy including segment IV+I resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip. [in press].
Article12. Hwang S, Ha TY, Kim JS, Kim KH, Lee SG, Lee YJ. 2003; Isolated caudate lobectomy with bile duct resection performed in a patient with type IV hilar bile duct cancer. J Korean Surg Soc. 64:441–446.13. Kawarada Y, Isaji S, Taoka H, Tabata M, Das BC, Yokoi H. 1999; S4a+S5 with caudate lobe (S1) resection using the Taj Mahal liver parenchymal resection for carcinoma of the biliary tract. J Gastrointest Surg. 3:369–373. DOI: 10.1016/S1091-255X(99)80052-3. PMID: 10482688.14. Hwang S, Moon DB, Park EH, Kim MH, Lee YJ, Lee SG. 2003; S4a+S5 with caudate lobe (S1) resection as a parenchyma-preserving liver resection for a patient with type IIIb hilar bile duct cancer. J Korean Surg Soc. 64:515–520.15. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Shimizu Y, et al. 1998; Segments I and IV resection as a new approach for hepatic hilar cholangiocarcinoma. Am J Surg. 175:229–231. DOI: 10.1016/S0002-9610(97)00295-X. PMID: 9560126.
Article16. Klempnauer J, Ridder GJ, Werner M, Weimann A, Pichlmayr R. 1997; What constitutes long-term survival after surgery for hilar cholangiocarcinoma? Cancer. 79:26–34. DOI: 10.1002/(SICI)1097-0142(19970101)79:1<26::AID-CNCR5>3.0.CO;2-K. PMID: 8988723.17. Lee SG, Hwang S. 2005; How I do it: assessment of hepatic functional reserve for indication of hepatic resection. J Hepatobiliary Pancreat Surg. 12:38–43. DOI: 10.1007/s00534-004-0949-9. PMID: 15754098.
Article18. Hwang S, Ha TY, Ko GY, Kwon DI, Song GW, Jung DH, et al. 2015; Preoperative sequential portal and hepatic vein embolization in patients with hepatobiliary malignancy. World J Surg. 39:2990–2998. DOI: 10.1007/s00268-015-3194-2. PMID: 26304608.
Article19. Hwang S, Ko GY, Kim MH, Lee SK, Gwon DI, Ha TY, et al. 2016; Preoperative left portal vein embolization for left liver resection in high-risk hepatobiliary malignancy patients. World J Surg. 40:2758–2765. DOI: 10.1007/s00268-016-3618-7. PMID: 27384172.
Article20. Mizumoto R, Kawarada Y, Suzuki H. 1986; Surgical treatment of hilar carcinoma of the bile duct. Surg Gynecol Obstet. 162:153–158. PMID: 3945893.21. Chen XP, Lau WY, Huang ZY, Zhang ZW, Chen YF, Zhang WG, et al. 2009; Extent of liver resection for hilar cholangiocarcinoma. Br J Surg. 96:1167–1175. DOI: 10.1002/bjs.6618. PMID: 19705374.
Article22. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. 2010; Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 17:476–489. DOI: 10.1007/s00534-009-0204-5. PMID: 19851704.
Article23. Hwang S, Ha TY, Song GW, Jung DH, Ahn CS, Moon DB, et al. 2015; Quantified risk assessment for major hepatectomy via the indocyanine green clearance rate and liver volumetry combined with standard liver volume. J Gastrointest Surg. 19:1305–1314. DOI: 10.1007/s11605-015-2846-8. PMID: 25947549.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parenchyma-preserving hepatectomy including segments I + IV resection and bile duct resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip
- Resection or transplantation for perihilar cholangiocarcinoma
- Surgery for Perihilar Cholangiocarcinoma
- Development of perihilar cholangiocarcinoma at 29 years after first hepatectomy for hepatolithiasis
- Necrosectomy of hepatic left lateral section after blunt abdominal trauma in a patient who underwent central hepatectomy and bile duct resection for perihilar cholangiocarcinoma