Ann Hepatobiliary Pancreat Surg.
2020 Aug;24(3):345-351. 10.14701/ahbps.2020.24.3.345.
Necrosectomy of hepatic left lateral section after blunt abdominal trauma in a patient who underwent central hepatectomy and bile duct resection for perihilar cholangiocarcinoma
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2505349
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.345
Abstract
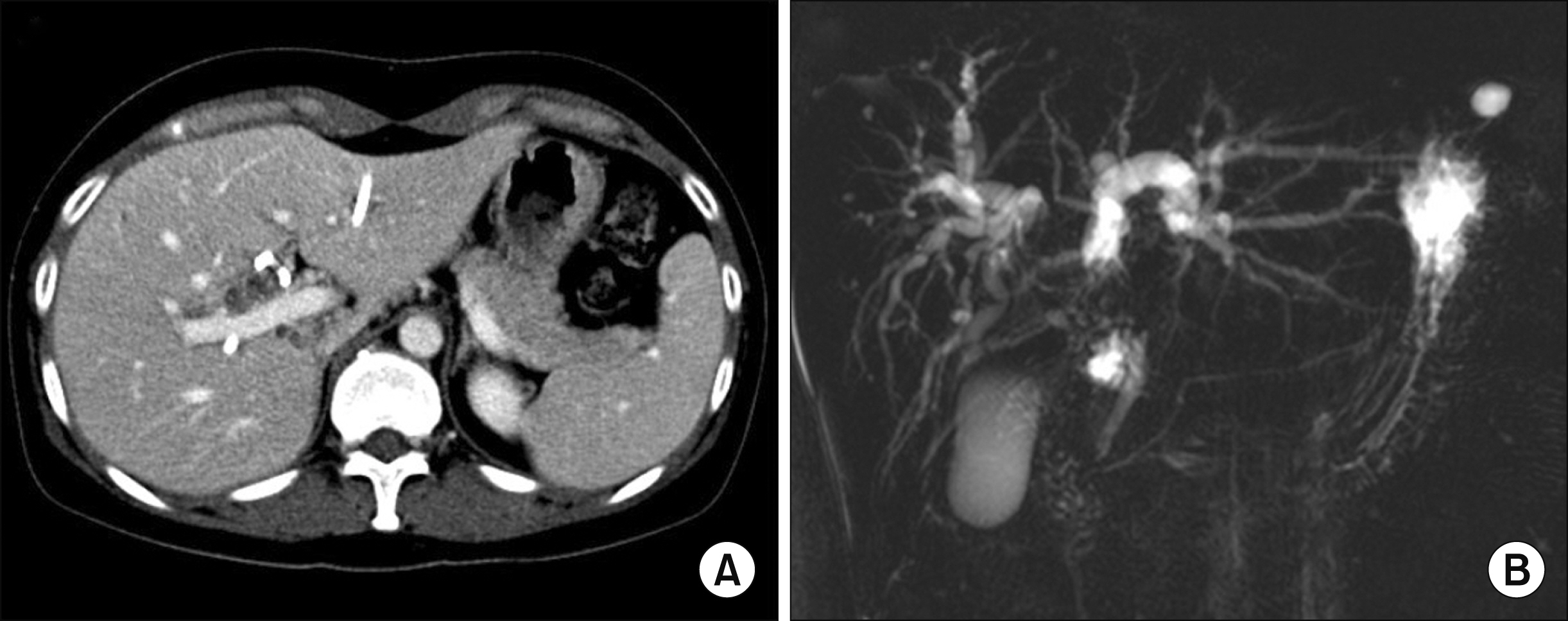
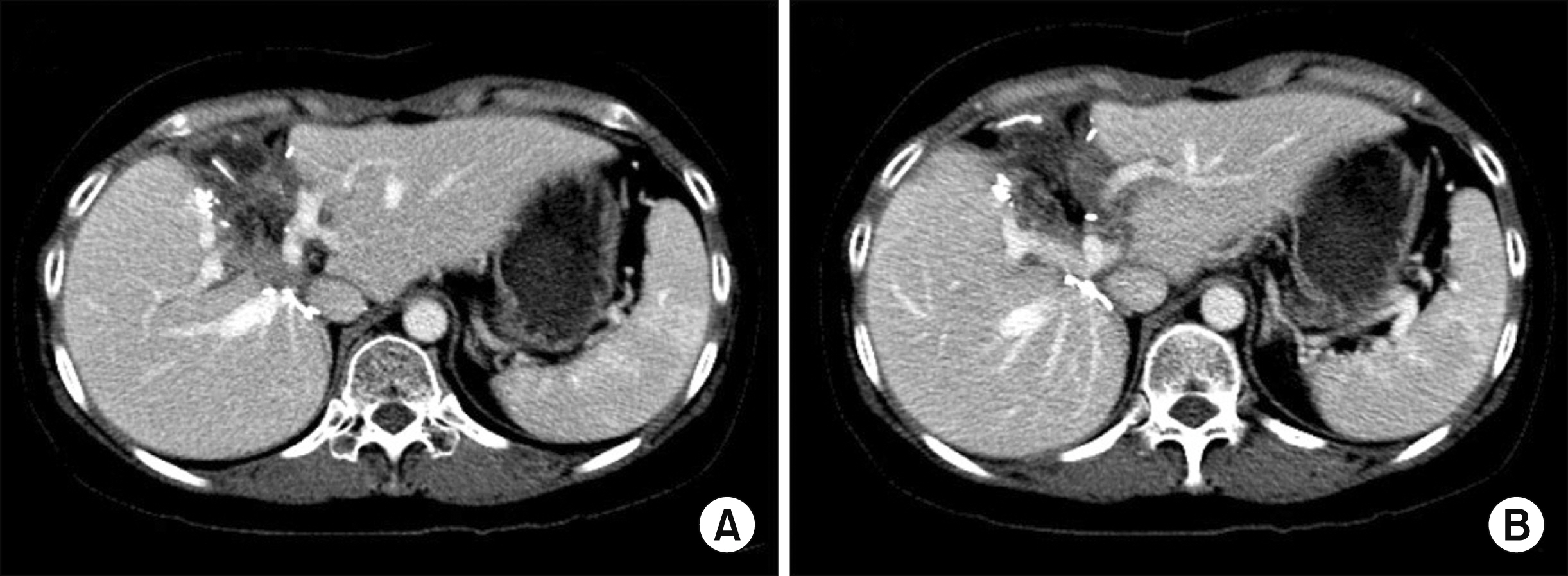
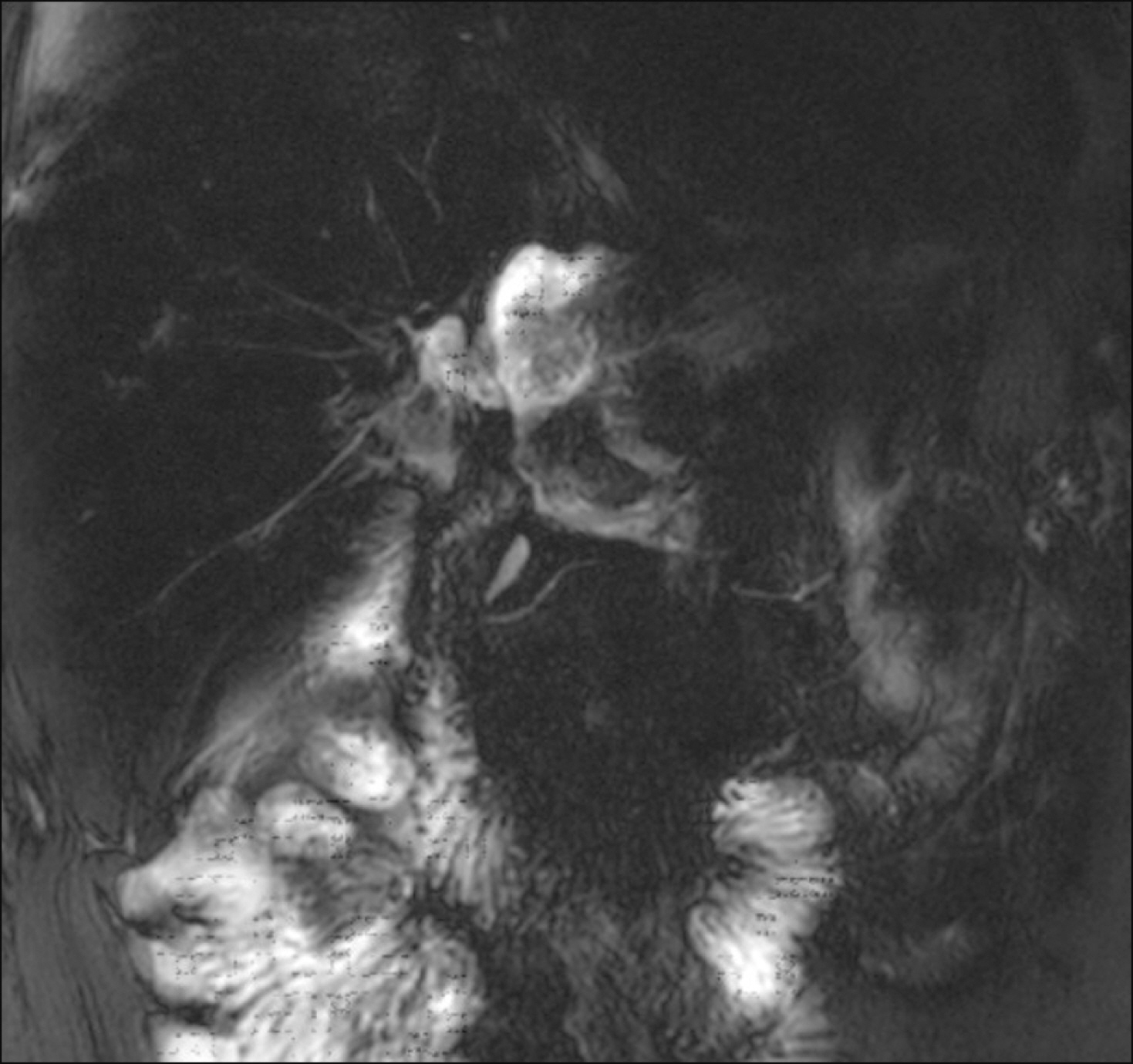
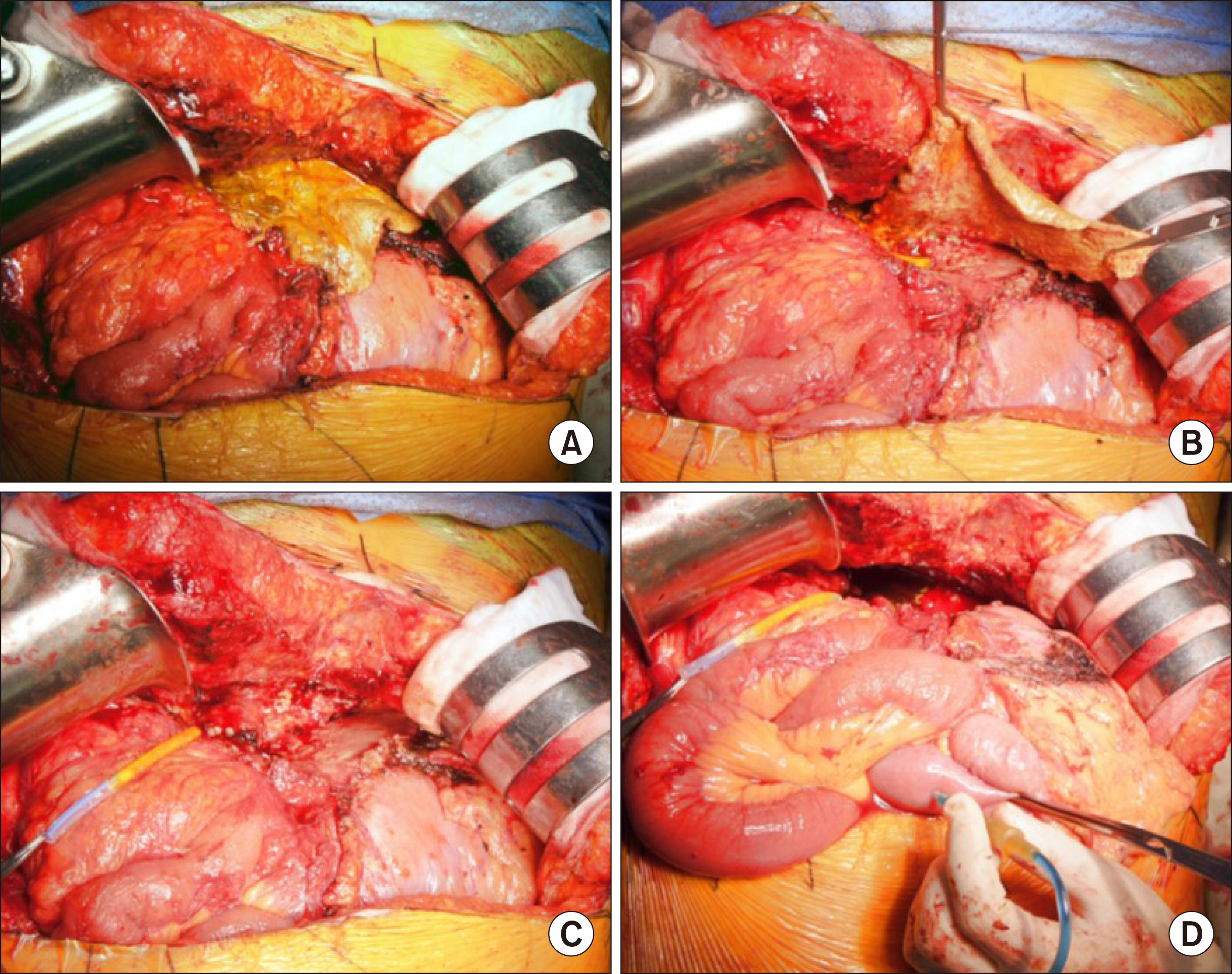
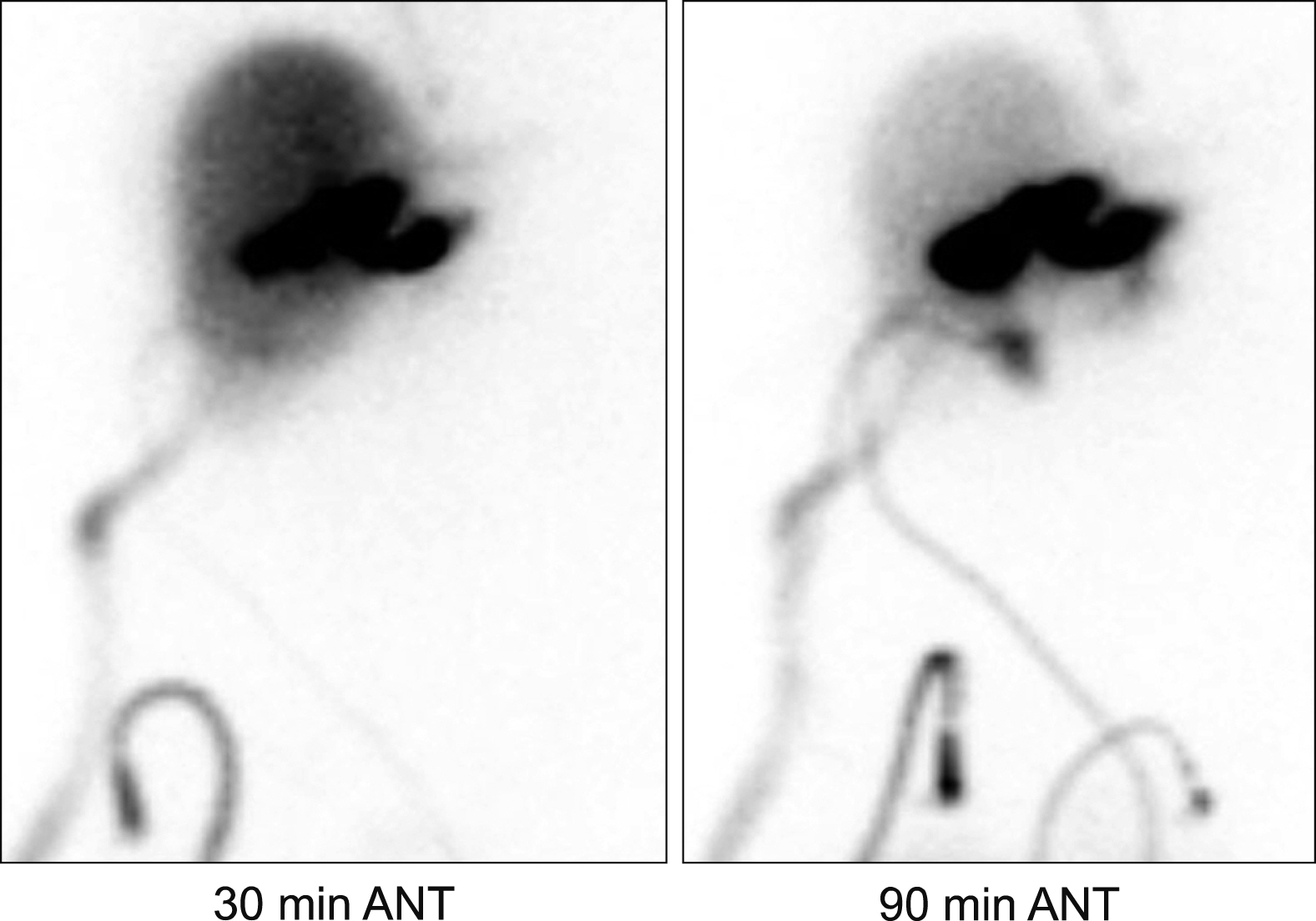
- When the liver is divided into the right and left halves after central hepatectomy, a serious injury to the one half of the liver can destroy the ipsilateral half. We report a case showing total necrosis of the hepatic left lateral section (LLS) caused by blunt abdominal trauma in a patient who had undergone central hepatectomy and bile duct resection for perihilar cholangiocarcinoma. A 47-year-old female patient was transferred because of postoperative status following blunt abdominal trauma. Five years before, she had been diagnosed with perihilar cholangiocarcinoma. Since the tumor extent was compatible with Bismuth-Corlette type IV, she underwent central hepatectomy and bile duct resection. After five years, she experienced an industrial safety accident, in which a heavy refrigerator fell over her body. She underwent emergency duodenal diversion surgery with distal gastrectomy and Roux-en-Y gastrojejunostomy. During this surgery,serious ischemic injury of the LLS with occlusion of the left portal vein and hepatic artery was identified, but not treated. After three weeks, LLS necrosectomy with repair of the jejunal limb was done. Postoperative bile leak developed and required supportive care for two months for its healing. She is currently doing well without any physical discomfort four months after the necrosectomy. Our experience with this case suggests that an injury to the afferent jejunal limb requires an individualized treatment strategy including long-standing waiting with effective drainage for spontaneous healing. The experience of this case appears to be theoretically matched with late-stage resection of LLS following central hepatectomy and bile duct resection.
Figure
Reference
-
1. Miyazaki M, Ito H, Nakagawa K, Ambiru S, Shimizu H, Okaya T, et al. 1999; Parenchyma-preserving hepatectomy in the surgical treatment of hilar cholangiocarcinoma. J Am Coll Surg. 189:575–583. DOI: 10.1016/S1072-7515(99)00219-7. PMID: 10589594.
Article2. Kawarada Y, Isaji S, Taoka H, Tabata M, Das BC, Yokoi H. 1999; S4a + S5 with caudate lobe (S1) resection using the Taj Mahal liver parenchymal resection for carcinoma of the biliary tract. J Gastrointest Surg. 3:369–373. DOI: 10.1016/S1091-255X(99)80052-3. PMID: 10482688.
Article3. Hwang S, Moon DB, Park EH, Kim MH, Lee YJ, Lee SG. 2003; S4a+S5 with caudate lobe (S1) resection as a parenchyma-preserving liver resection for a patient with type IIIb hilar bile duct cancer. J Korean Surg Soc. 64:515–520.4. Song GW, Lee SG, Moon DB, Ahn CS, Hwang S, Kim KH, et al. 2017; Dual-graft adult living donor liver transplantation: an innovative surgical procedure for live liver donor pool expansion. Ann Surg. 266:10–18. DOI: 10.1097/SLA.0000000000001776. PMID: 27192349.5. Lu CH, Chen TY, Huang TL, Tsang LL, Ou HY, Yu CY, et al. 2012; Regeneration and outcome of dual grafts in living donor liver transplantation. Clin Transplant. 26:E143–E148. DOI: 10.1111/j.1399-0012.2012.01621.x. PMID: 22432787.
Article6. Hwang S, Yoon SY, Jung SW, Namgoong JM, Park GC, Gwon DI, et al. 2011; Therapeutic induction of hepatic atrophy for isolated injury of the right posterior sectoral duct following laparoscopic cholecystectomy. Korean J Hepatobiliary Pancreat Surg. 15:189–193. DOI: 10.14701/kjhbps.2011.15.3.189. PMID: 26421038. PMCID: PMC4582538.
Article7. Hwang S, Lee SG, Lee YJ, Ha TY, Ko GY, Song GW. 2007; Delayed-onset isolated injury of the right posterior segment duct after laparoscopic cholecystectomy: a report of hepatic segmental atrophy induction. Surg Laparosc Endosc Percutan Tech. 17:203–205. DOI: 10.1097/SLE.0b013e31804d4488. PMID: 17581468.
Article8. Hwang S, Park GC, Ha TY, Ko GY, Gwon DI, Choi YI, et al. 2012; Hepatic parenchymal atrophy induction for intractable segmental bile duct injury after liver resection. Hepatogastroenterology. 59:866–868. DOI: 10.5754/hge10172. PMID: 22469733.9. Yoon YI, Hwang S, Cho YJ, Ha TY, Song GW, Jung DH. 2015; Therapeutic effect of trans-drain administration of antibiotics in patients showing intractable pancreatic leak-associated pus drainage after pancreaticoduodenectomy. Korean J Hepatobiliary Pancreat Surg. 19:17–24. DOI: 10.14701/kjhbps.2015.19.1.17. PMID: 26155272. PMCID: PMC4494091.
Article10. Lee SG, Song GW, Hwang S, Ha TY, Moon DB, Jung DH, et al. 2010; Surgical treatment of hilar cholangiocarcinoma in the new era: the Asan experience. J Hepatobiliary Pancreat Sci. 17:476–489. DOI: 10.1007/s00534-009-0204-5. PMID: 19851704.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parenchyma-preserving hepatectomy including segments I + IV resection and bile duct resection in a patient with type IV perihilar cholangiocarcinoma: A case report with video clip
- Spontaneous rupture of intrahepatic bile duct following portal vein embolization in a patient with perihilar cholangiocarcinoma: a case of successful curative resection
- Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies
- ALPPS in a patient with periductal infiltrating intrahepatic cholangiocarcinoma
- Portal vein wedge resection and patch venoplasty using autologous and homologous vein grafts during surgery for hepatobiliary malignancies