Int J Stem Cells.
2021 Feb;14(1):94-102. 10.15283/ijsc20070.
The Effects of Human Bone Marrow-Derived Mesenchymal Stem Cell Conditioned Media Produced with Fetal Bovine Serum or Human Platelet Lysate on Skin Rejuvenation Characteristics
- Affiliations
-
- 1Research Institute, SCM Lifesciences Co. Ltd., Incheon, Korea
- 2Department of Biomedical Sciences, Inha University College of Medicine, Incheon, Korea
- KMID: 2513086
- DOI: http://doi.org/10.15283/ijsc20070
Abstract
- Background and Objectives
Human mesenchymal stem cell-conditioned medium (MSC-CM) is produced using mesenchymal stem cell culture technology and has various benefits for the skin, including wrinkle removal, skin regeneration, and increased antioxidant activity. Its popularity is thus increasing in the field of functional cosmetics.
Methods and Results
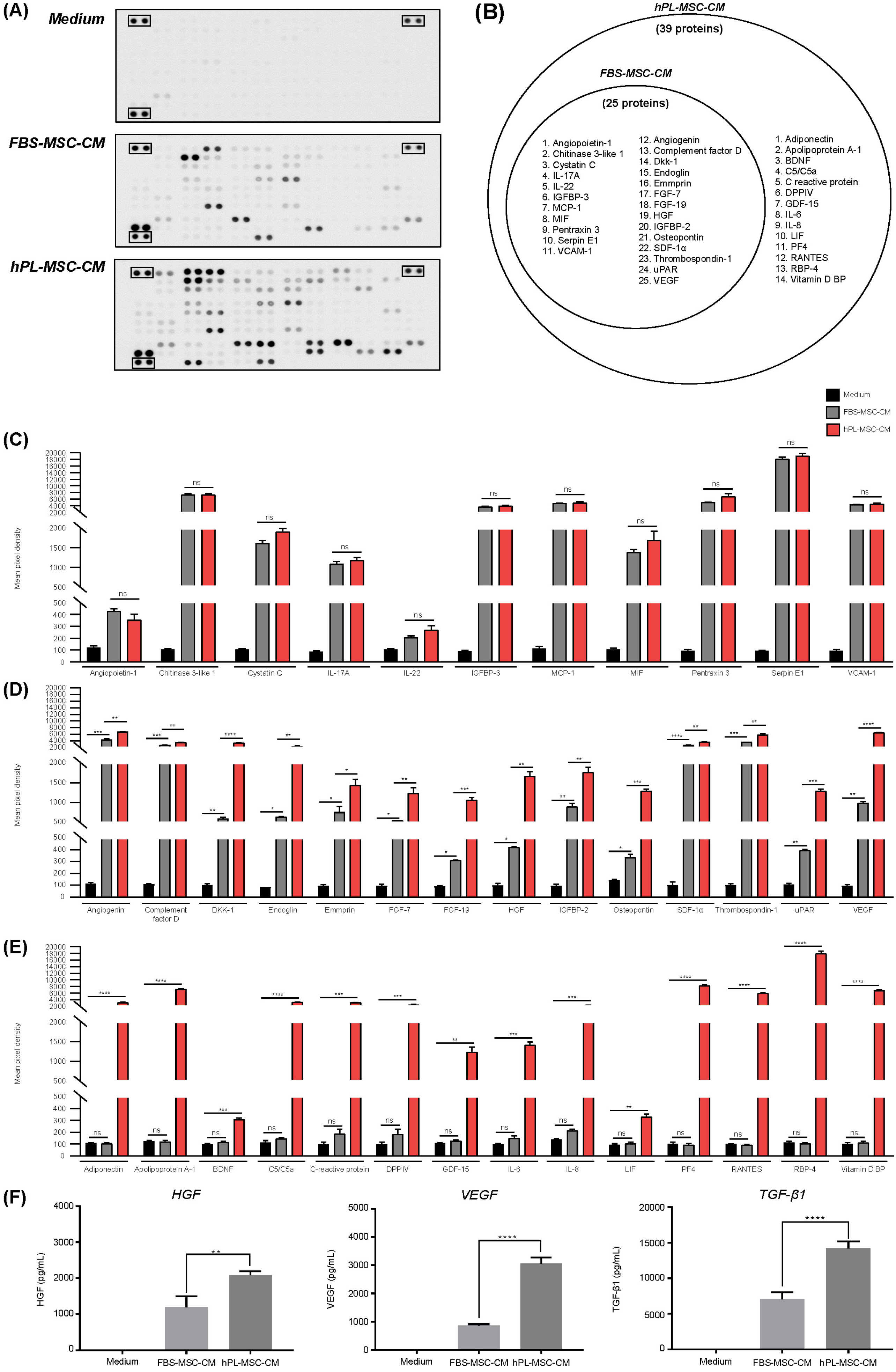
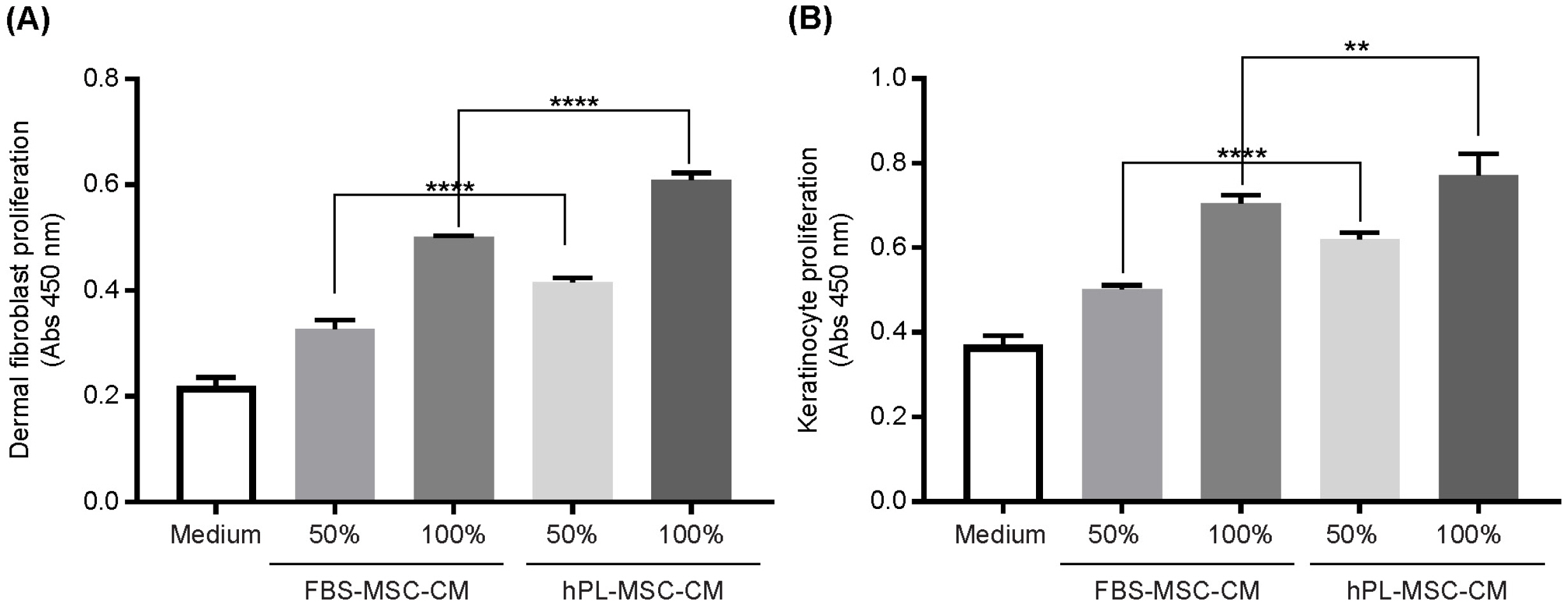
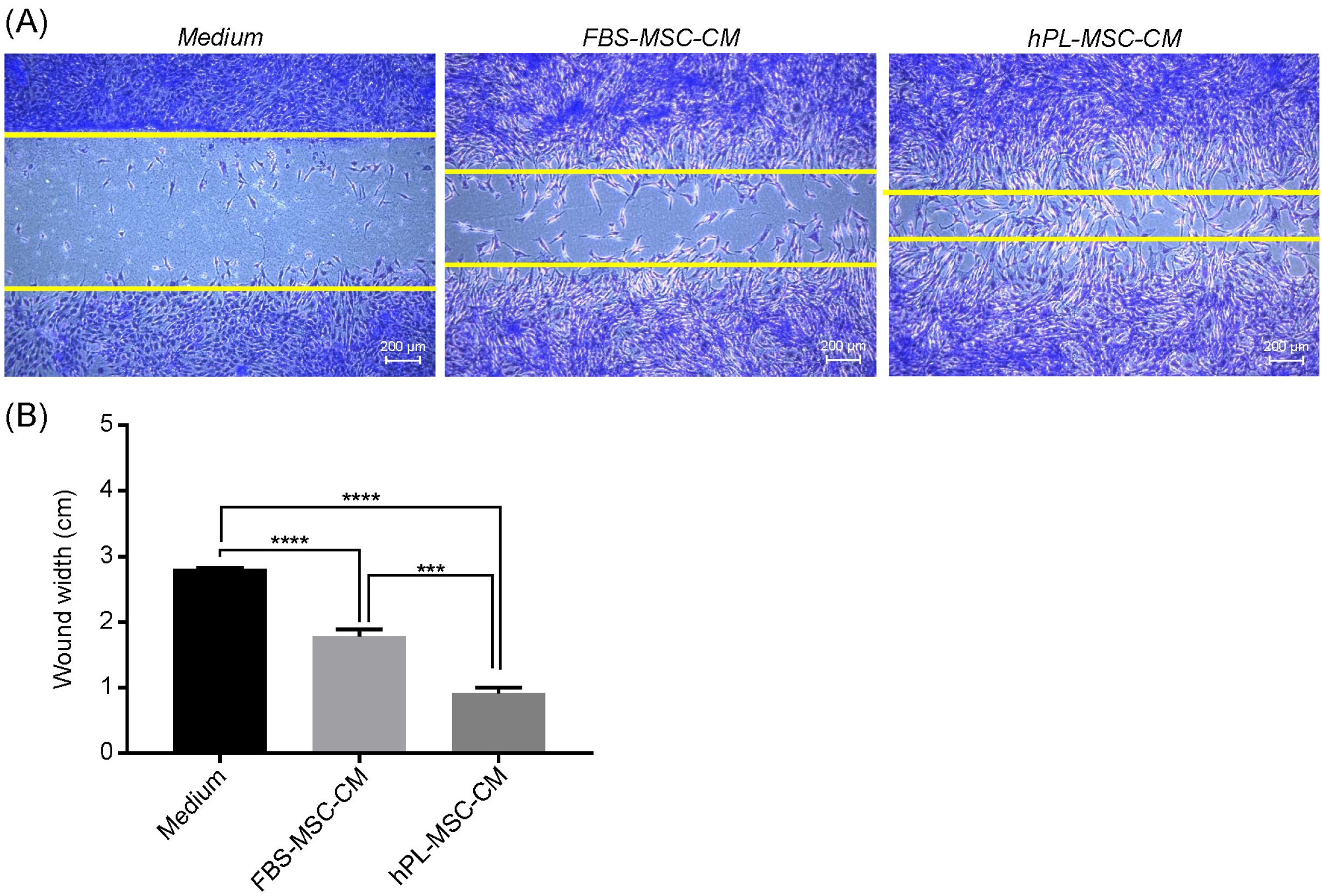
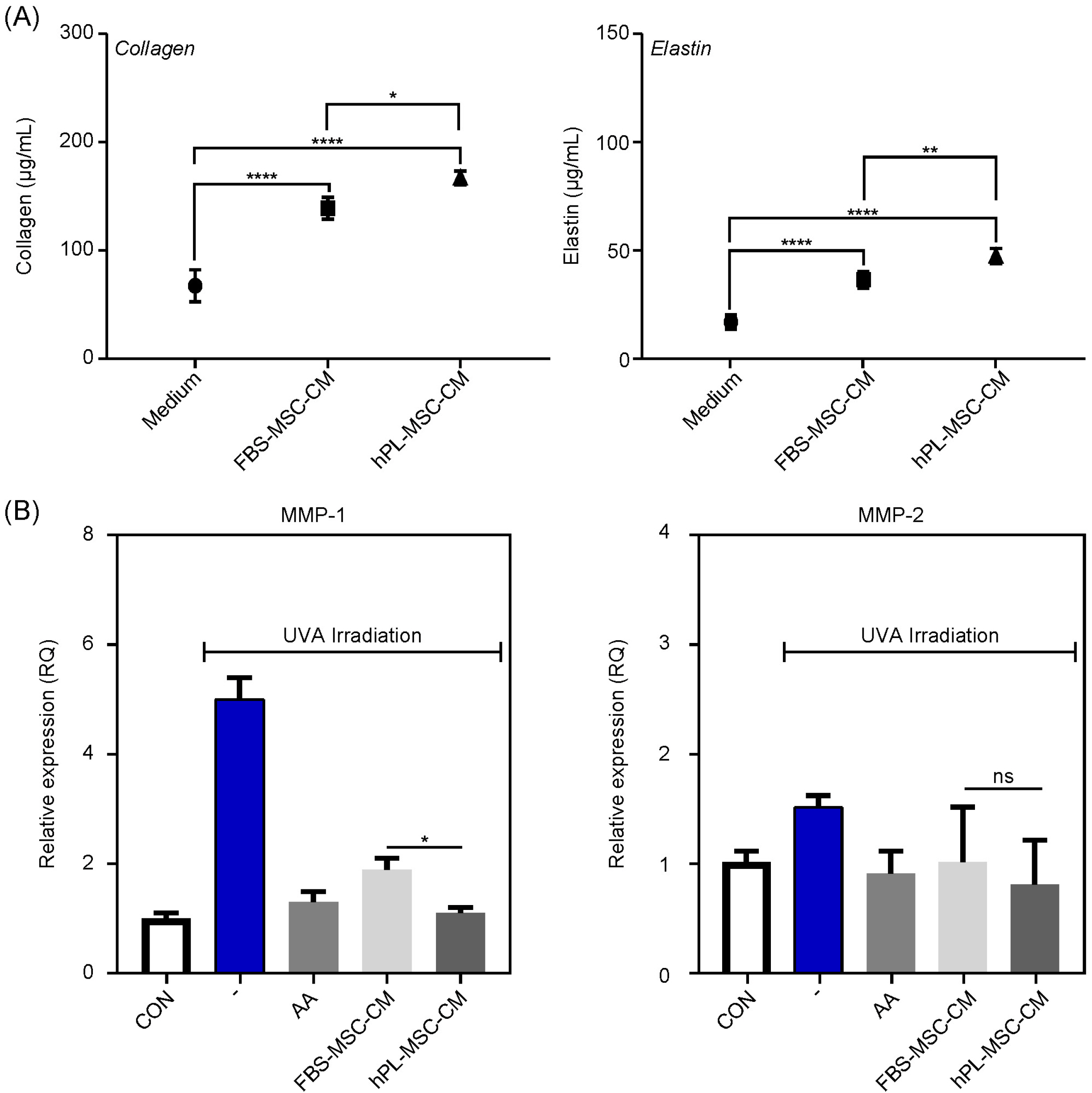
In this study, we analyzed the effects of fetal bovine serum-supplemented MSC-CM (FBSMSC-CM) and human platelet lysate-supplemented MSC-CM (hPL-MSC-CM) on skin rejuvenation characteristics. We found that the concentrations of important growth factors (VEGF, TGF-β1, and HGF) and secretory proteins for skin regeneration were significantly higher in hPL-MSC-CM than in FBS-MSC-CM. Furthermore, the capacity for inducing proliferation of human dermal fibroblast (HDF) and keratinocytes, the migration ability of HDF, extracellular matrix (ECM) production such as collagen and elastin was higher in hPL-MSC-CM than that in FBSMSC-CM.
Conclusions
These results support the usefulness and high economic value of hPL-MSC-CM as an alternative source of FBS-MSC-CM in the cosmetic industry for skin rejuvenation.
Figure
Reference
-
References
1. Muthukumar A, Seetharam RN. 2016; Stem cell derived cosmetic products: an overview. Manipal J Med Sci. 1:46–52.2. Vizoso FJ, Eiro N, Cid S, Schneider J, Perez-Fernandez R. 2017; Mesenchymal stem cell secretome: toward cell-free therapeutic strategies in regenerative medicine. Int J Mol Sci. 18:1852. DOI: 10.3390/ijms18091852. PMID: 28841158. PMCID: PMC5618501.
Article3. Barrientos S, Brem H, Stojadinovic O, Tomic-Canic M. 2014; Clinical application of growth factors and cytokines in wound healing. Wound Repair Regen. 22:569–578. DOI: 10.1111/wrr.12205. PMID: 24942811. PMCID: PMC4812574.
Article4. Van Pham P. Van Pham P, editor. 2016. Mesenchymal stem cells in clinical applications. Stem Cell Processing. Stem Cells in Clinical Applications. Springer;Cham: p. 37–69. DOI: 10.1007/978-3-319-40073-0_2.
Article5. Becherucci V, Piccini L, Casamassima S, Bisin S, Gori V, Gentile F, Ceccantini R, De Rienzo E, Bindi B, Pavan P, Cunial V, Allegro E, Ermini S, Brugnolo F, Astori G, Bambi F. 2018; Human platelet lysate in mesenchymal stromal cell expansion according to a GMP grade protocol: a cell factory experience. Stem Cell Res Ther. 9:124. DOI: 10.1186/s13287-018-0863-8. PMID: 29720245. PMCID: PMC5930506.
Article6. Hemeda H, Giebel B, Wagner W. 2014; Evaluation of human platelet lysate versus fetal bovine serum for culture of mesenchymal stromal cells. Cytotherapy. 16:170–180. DOI: 10.1016/j.jcyt.2013.11.004. PMID: 24438898.
Article7. Griffiths S, Baraniak PR, Copland IB, Nerem RM, McDevitt TC. 2013; Human platelet lysate stimulates high-passage and senescent human multipotent mesenchymal stromal cell growth and rejuvenation in vitro. Cytotherapy. 15:1469–1483. DOI: 10.1016/j.jcyt.2013.05.020. PMID: 23981539.
Article8. Schallmoser K, Bartmann C, Rohde E, Reinisch A, Kashofer K, Stadelmeyer E, Drexler C, Lanzer G, Linkesch W, Strunk D. 2007; Human platelet lysate can replace fetal bovine serum for clinical-scale expansion of functional mesenchymal stromal cells. Transfusion. 47:1436–1446. DOI: 10.1111/j.1537-2995.2007.01220.x. PMID: 17655588.
Article9. Kim WS, Park SH, Ahn SJ, Kim HK, Park JS, Lee GY, Kim KJ, Whang KK, Kang SH, Park BS, Sung JH. 2008; Whitening effect of adipose-derived stem cells: a critical role of TGF-beta 1. Biol Pharm Bull. 31:606–610. DOI: 10.1248/bpb.31.606. PMID: 18379050.
Article10. Song SU, Kim CS, Yoon SP, Kim SK, Lee MH, Kang JS, Choi GS, Moon SH, Choi MS, Cho YK, Son BK. 2008; Variations of clonal marrow stem cell lines established from human bone marrow in surface epitopes, differentiation potential, gene expression, and cytokine secretion. Stem Cells Dev. 17:451–461. DOI: 10.1089/scd.2007.0167. PMID: 18513161.
Article11. Korpela E, Yohan D, Chin LC, Kim A, Huang X, Sade S, Van Slyke P, Dumont DJ, Liu SK. 2014; Vasculotide, an Angiopoietin-1 mimetic, reduces acute skin ionizing radiation damage in a preclinical mouse model. BMC Cancer. 14:614. DOI: 10.1186/1471-2407-14-614. PMID: 25159192. PMCID: PMC4159535.
Article12. Lecron JC, Paris I, Bernard FX, Morel F. Quesniaux V, Ryffel B, Padova F, editors. 2013. Contribution of IL-22 to experimental skin inflammation. IL-17, IL-22 and Their Producing Cells: Role in Inflammation and Autoimmunity. Springer Basel;Basel: p. 305–317. DOI: 10.1007/978-3-0348-0522-3_22.
Article13. Liu J, Guo Y, Huang Y, Xue H, Bai S, Zhu J, Xia X, Shen B, Fang W. 2018; Effects of insulin-like growth factor binding protein 3 on apoptosis of cutaneous squamous cell carcinoma cells. Onco Targets Ther. 11:6569–6577. DOI: 10.2147/OTT.S167187. PMID: 30323629. PMCID: PMC6178943.
Article14. Shallo H, Plackett TP, Heinrich SA, Kovacs EJ. 2003; Monocyte chemoattractant protein-1 (MCP-1) and macrophage infiltration into the skin after burn injury in aged mice. Burns. 29:641–647. DOI: 10.1016/S0305-4179(03)00070-6. PMID: 14556721.
Article15. Shimizu T. 2005; Role of macrophage migration inhibitory factor (MIF) in the skin. J Dermatol Sci. 37:65–73. DOI: 10.1016/j.jdermsci.2004.08.007. PMID: 15659324.
Article16. Cappuzzello C, Doni A, Dander E, Pasqualini F, Nebuloni M, Bottazzi B, Mantovani A, Biondi A, Garlanda C, D'Amico G. 2016; Mesenchymal stromal cell-derived PTX3 promotes wound healing via fibrin remodeling. J Invest Dermatol. 136:293–300. DOI: 10.1038/JID.2015.346. PMID: 26763449.
Article17. Simone TM, Longmate WM, Law BK, Higgins PJ. 2015; Targeted inhibition of PAI-1 activity impairs epithelial migration and wound closure following cutaneous injury. Adv Wound Care (New Rochelle). 4:321–328. DOI: 10.1089/wound.2014.0611. PMID: 26029482. PMCID: PMC4440983.
Article18. Archer NK, Adappa ND, Palmer JN, Cohen NA, Harro JM, Lee SK, Miller LS, Shirtliff ME. 2016; Interleukin-17A (IL-17A) and IL-17F are critical for antimicrobial peptide production and Clearance of Staphylococcus aureus nasal colonization. Infect Immun. 84:3575–3583. DOI: 10.1128/IAI.00596-16. PMID: 27736775. PMCID: PMC5116734.
Article19. Blankenvoorde MF, van't Hof W, Walgreen-Weterings E, van Steenbergen TJ, Brand HS, Veerman EC, Nieuw Amerongen AV. 1998; Cystatin and cystatin-derived peptides have antibacterial activity against the pathogen Porphyromonas gingivalis. Biol Chem. 379:1371–1375. PMID: 9865612.20. Yamaguchi Y, Morita A, Maeda A, Hearing VJ. 2009; Regulation of skin pigmentation and thickness by Dickkopf 1 (DKK1). J Investig Dermatol Symp Proc. 14:73–75. DOI: 10.1038/jidsymp.2009.4. PMID: 19675559. PMCID: PMC2793095.
Article21. Valluru M, Staton CA, Reed MW, Brown NJ. 2011; Transforming growth factor-β and endoglin signaling orchestrate wound healing. Front Physiol. 2:89. DOI: 10.3389/fphys.2011.00089. PMID: 22164144. PMCID: PMC3230065.
Article22. Huet E, Vallée B, Szul D, Verrecchia F, Mourah S, Jester JV, Hoang-Xuan T, Menashi S, Gabison EE. 2008; Extracellular matrix metalloproteinase inducer/CD147 promotes myofibroblast differentiation by inducing alpha-smooth muscle actin expression and collagen gel contraction: implications in tissue remodeling. FASEB J. 22:1144–1154. DOI: 10.1096/fj.07-8748com. PMID: 17965264.
Article23. Nunes QM, Li Y, Sun C, Kinnunen TK, Fernig DG. 2016; Fibroblast growth factors as tissue repair and regeneration therapeutics. PeerJ. 4:e1535. DOI: 10.7717/peerj.1535. PMID: 26793421. PMCID: PMC4715458.
Article24. Shim JH, Park JY, Lee MG, Kang HH, Lee TR, Shin DW. 2013; Human dermal stem/progenitor cell-derived conditioned medium ameliorates ultraviolet a-induced damage of normal human dermal fibroblasts. PLoS One. 8:e67604. DOI: 10.1371/journal.pone.0067604. PMID: 23874431. PMCID: PMC3708938.
Article25. Guo R, Chai L, Chen L, Chen W, Ge L, Li X, Li H, Li S, Cao C. 2015; Stromal cell-derived factor 1 (SDF-1) accelerated skin wound healing by promoting the migration and proliferation of epidermal stem cells. In Vitro Cell Dev Biol Anim. 51:578–585. DOI: 10.1007/s11626-014-9862-y. PMID: 25636237.
Article26. Weber CE, Li NY, Wai PY, Kuo PC. 2012; Epithelial-mesenchymal transition, TGF-β, and osteopontin in wound healing and tissue remodeling after injury. J Burn Care Res. 33:311–318. DOI: 10.1097/BCR.0b013e318240541e. PMID: 22561306. PMCID: PMC5207477.
Article27. Detmar M. 2000; The role of VEGF and thrombospondins in skin angiogenesis. J Dermatol Sci. 24(Suppl 1):S78–S84. DOI: 10.1016/S0923-1811(00)00145-6. PMID: 11137400.
Article28. Gulyaev A, Piven V. Osman NAA, Abas WABW, Wahab AKA, Ting HN, editors. 2011. Rat model of healing the skin wounds and joint inflammations by recombinant human angiogenin, erythropoietin and tumor necrosis factor-α. 5th Kuala Lumpur International Conference on Biomedical Engineering 2011. IFMBE Proceedings, vol 35. Springer;Berlin, Heidelberg: p. 854–857. DOI: 10.1007/978-3-642-21729-6_208.
Article29. D'Alessio S, Gerasi L, Blasi F. 2008; uPAR-deficient mouse keratinocytes fail to produce EGFR-dependent laminin-5, affecting migration in vivo and in vitro. J Cell Sci. 121(Pt 23):3922–3932. DOI: 10.1242/jcs.037549. PMID: 19001498.30. Shibata S, Tada Y, Asano Y, Hau CS, Kato T, Saeki H, Yamauchi T, Kubota N, Kadowaki T, Sato S. 2012; Adiponectin regulates cutaneous wound healing by promoting keratinocyte proliferation and migration via the ERK signaling pathway. J Immunol. 189:3231–3241. DOI: 10.4049/jimmunol.1101739. PMID: 22904306.
Article31. Palazzo E, Marconi A, Truzzi F, Dallaglio K, Petrachi T, Humbert P, Schnebert S, Perrier E, Dumas M, Pincelli C. 2012; Role of neurotrophins on dermal fibroblast survival and differentiation. J Cell Physiol. 227:1017–1025. DOI: 10.1002/jcp.22811. PMID: 21503896.
Article32. Eisman R, Surrey S, Ramachandran B, Schwartz E, Poncz M. 1990; Structural and functional comparison of the genes for human platelet factor 4 and PF4alt. Blood. 76:336–344. DOI: 10.1182/blood.V76.2.336.336. PMID: 1695112.
Article33. van den Broek LJ, Kroeze KL, Waaijman T, Breetveld M, Sampat-Sardjoepersad SC, Niessen FB, Middelkoop E, Scheper RJ, Gibbs S. 2014; Differential response of human adipose tissue-derived mesenchymal stem cells, dermal fibroblasts, and keratinocytes to burn wound exudates: potential role of skin-specific chemokine CCL27. Tissue Eng Part A. 20:197–209. DOI: 10.1089/ten.tea.2013.0123. PMID: 23980822. PMCID: PMC3875150.
Article34. Stephensen CB. 2001; Vitamin A, infection, and immune function. Annu Rev Nutr. 21:167–192. DOI: 10.1146/annurev.nutr.21.1.167. PMID: 11375434.
Article35. Rennekampff HO, Hansbrough JF, Kiessig V, Doré C, Sticherling M, Schröder JM. 2000; Bioactive interleukin-8 is expressed in wounds and enhances wound healing. J Surg Res. 93:41–54. DOI: 10.1006/jsre.2000.5892. PMID: 10945942.
Article36. Gorman S, Geldenhuys S, Judge M, Weeden CE, Waithman J, Hart PH. 2016; Dietary vitamin D increases percentages and function of regulatory T cells in the skin-draining lymph nodes and suppresses dermal inflammation. J Immunol Res. 2016:1426503. DOI: 10.1155/2016/1426503. PMID: 27672666. PMCID: PMC5031886.
Article37. Lee EG, Mickle-Kawar BM, Gallucci RM. 2013; IL-6 deficiency exacerbates skin inflammation in a murine model of irritant dermatitis. J Immunotoxicol. 10:192–200. DOI: 10.3109/1547691X.2012.707700. PMID: 22966985.
Article38. Duncan MR, Berman B. 1991; Stimulation of collagen and glycosaminoglycan production in cultured human adult dermal fibroblasts by recombinant human interleukin 6. J Invest Dermatol. 97:686–692. DOI: 10.1111/1523-1747.ep12483971. PMID: 1940439.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differentiation of adipose-derived stem cells into Schwann-like cells: fetal bovine serum or human serum?
- Influences of Xeno-Free Media on Mesenchymal Stem Cell Expansion for Clinical Application
- The Effect of Human Joint Fluid in the Surviviorship and Proliferation of Bone-Marrow Derived Progenitor Cell
- Efficacy of Microneedling Plus Human Stem Cell Conditioned Medium for Skin Rejuvenation: A Randomized, Controlled, Blinded Split-Face Study
- Clinical Safety and Efficacy of Autologous Bone Marrow-Derived Mesenchymal Stem Cell Transplantation in Sensorineural Hearing Loss Patients