Obstet Gynecol Sci.
2021 Jan;64(1):90-98. 10.5468/ogs.20216.
Comparison of single-port laparoscopy and laparotomy in early ovarian cancer surgical staging
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Women’s Cancer Center, Yonsei Cancer Center and Institute of Women’s Life Medical Science, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Obstetrics and Gynecology, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- KMID: 2511569
- DOI: http://doi.org/10.5468/ogs.20216
Abstract
Objectives
The aims of this study were to assess the feasibility of single-port laparoscopic surgical staging (SPLS) in early ovarian cancer and to compare the surgical outcomes of SPLS with those of staging laparotomy.
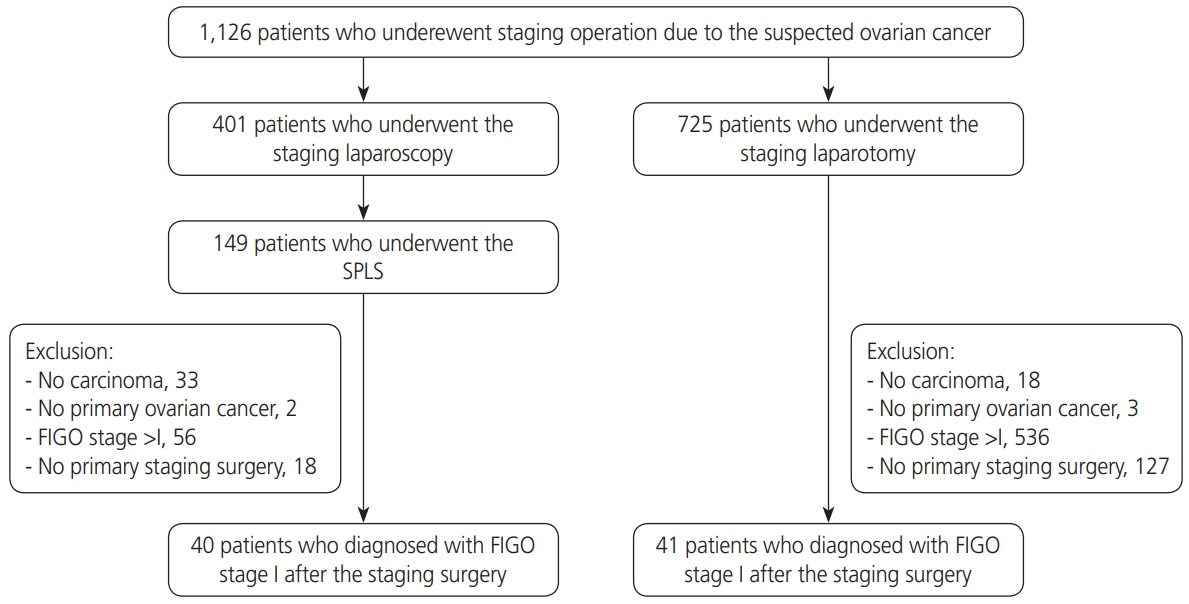
Methods
Between January 2014 and December 2018, 40 patients underwent SPLS and 41 patients underwent staging laparotomy at Yonsei Cancer Center. The patients were diagnosed with International Federation of Gynecology and Obstetrics (FIGO) stage I ovarian cancer. Variables such as patient age, body mass index (BMI), tumor size, FIGO stage, and perioperative surgical outcomes and survival outcomes of SPLS and laparotomy were compared.
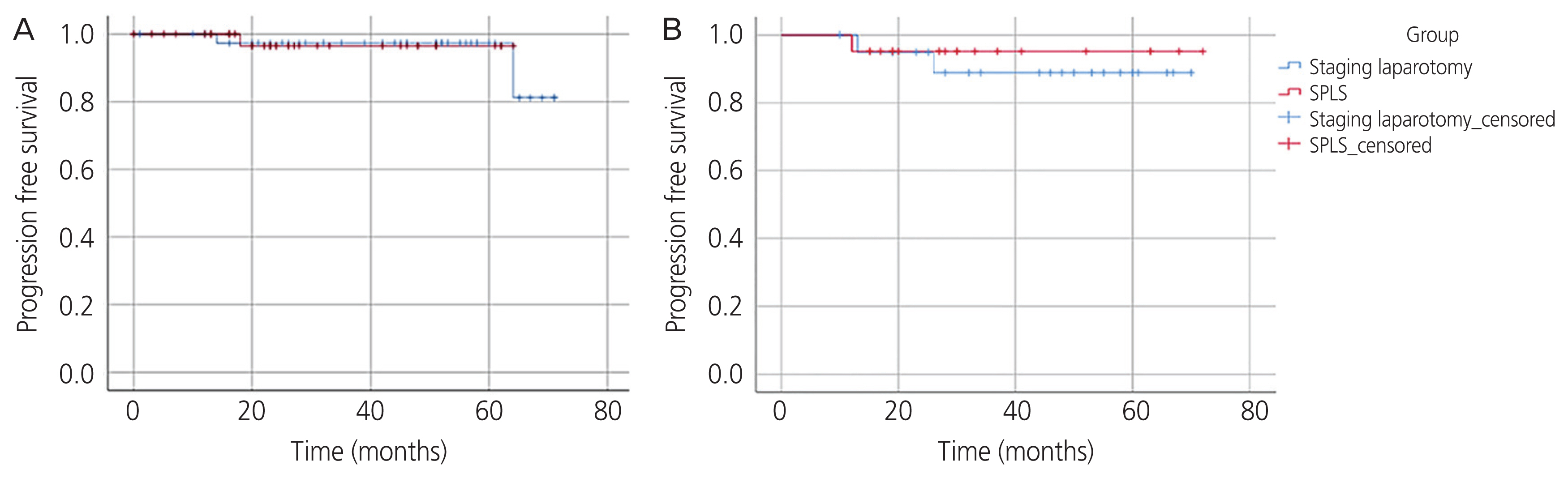
Results
The total operation time was similar between the 2 groups (SPLS: 201.4 vs. laparotomy: 203.0 minutes, P=0.806). The median tumor diameters in the SPLS and laparotomy groups were 11.0 (2.5–28 cm) and 15.4 (6–40 cm), respectively (P=0.001). The SPLS group had lower tumor spillage rate (5.0% vs. 19.5%, P=0.047), less intraoperative blood loss (102.0 vs. 371.5 mL, P<0.001), less postoperative pain, and shorter postoperative hospital stay (5 vs. 9.5 days, P<0.001). The intraoperative major complication rate was similar between groups (2.5% vs. 4.9%, P=0.571). There was no significant difference in progression-free survival between the 2 groups (P=0.945). There were no deaths in either group.
Conclusion
SPLS is feasible in early ovarian cancer and has better perioperative surgical outcomes, in some aspects, than staging laparotomy without compromising survival outcomes. SPLS could be performed in patients suspected to have early ovarian cancer.
Figure
Cited by 1 articles
-
Clinical relevance of sentinel lymph node biopsy in early ovarian cancer
Ki Eun Seon, Sang Wun Kim, Young Tae Kim
Obstet Gynecol Sci. 2023;66(6):498-508. doi: 10.5468/ogs.23114.
Reference
-
References
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article2. Howlader N, Noone A, Krapcho M, Miller D, Brest A, Yu M. SEER Cancer Statistics Review, 1975–2017. Bethesda (MD): National Cancer Institute;2020.3. Trimbos JB. Surgical treatment of early-stage ovarian cancer. Best Pract Res Clin Obstet Gynaecol. 2017; 41:60–70.
Article4. Sonoda Y, Barakat RR. Laparoscopic staging procedures. Levine DA, Barakat RR, Hoskins WJ, editors. Atlas of Procedures in Gynecologic Oncology. Boca Raton (FL): Taylor & Francis;2003. p. 103–30.5. Fagotti A, Bottoni C, Vizzielli G, Gueli Alletti S, Scambia G, Marana E, et al. Postoperative pain after conventional laparoscopy and laparoendoscopic single site surgery (LESS) for benign adnexal disease: a randomized trial. Fertil Steril. 2011; 96:255–259.e2.
Article6. Chong GO, Hong DG, Lee YS. Single-port (OctoPort) assisted extracorporeal ovarian cystectomy for the treatment of large ovarian cysts: compare to conventional laparoscopy and laparotomy. J Minim Invasive Gynecol. 2015; 22:45–9.
Article7. Schmitt A, Crochet P, Knight S, Tourette C, Loundou A, Agostini A. Single-port laparoscopy vs conventional laparoscopy in benign adnexal diseases: a systematic review and meta-analysis. J Minim Invasive Gynecol. 2017; 24:1083–95.
Article8. Lee IO, Yoon JW, Chung D, Yim GW, Nam EJ, Kim S, et al. A comparison of clinical and surgical outcomes between laparo-endoscopic single-site surgery and traditional multiport laparoscopic surgery for adnexal tumors. Obstet Gynecol Sci. 2014; 57:386–92.
Article9. Moulton L, Jernigan AM, Carr C, Freeman L, Escobar PF, Michener CM. Single-port laparoscopy in gynecologic oncology: seven years of experience at a single institution. Am J Obstet Gynecol. 2017; 217:610.e1–8.
Article10. Carbajal-Mamani SL, Schweer D, Markham MJ, Esnakula AK, Grajo JR, Castagno JC, et al. Robotic-assisted interval cytoreductive surgery in ovarian cancer: a feasibility study. Obstet Gynecol Sci. 2020; 63:150–7.
Article11. Weber S, McCann CK, Boruta DM, Schorge JO, Growdon WB. Laparoscopic surgical staging of early ovarian cancer. Rev Obstet Gynecol. 2011; 4:117–22.12. Lu Q, Qu H, Liu C, Wang S, Zhang Z, Zhang Z. Comparison of laparoscopy and laparotomy in surgical staging of apparent early ovarian cancer: 13-year experience. Medicine (Baltimore). 2016; 95:e3655.13. Yim GW, Jung YW, Paek J, Lee SH, Kwon HY, Nam EJ, et al. Transumbilical single-port access versus conventional total laparoscopic hysterectomy: surgical outcomes. Am J Obstet Gynecol. 2010; 203:26.e1–6.
Article14. Yim GW, Lee M, Nam EJ, Kim S, Kim YT, Kim SW. Is single-port access laparoscopy less painful than conventional laparoscopy for adnexal surgery? A comparison of postoperative pain and surgical outcomes. Surg Innov. 2013; 20:46–54.
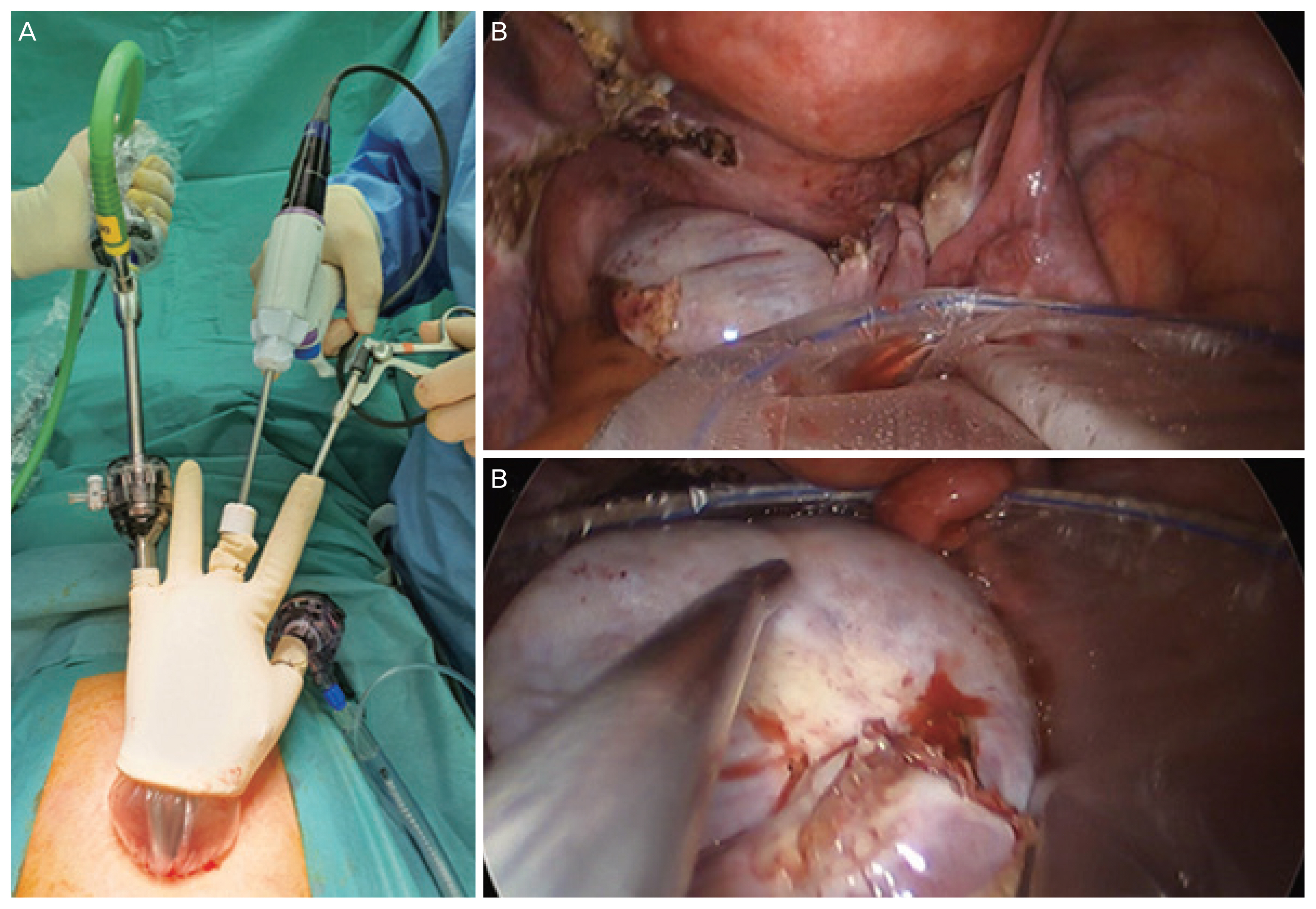
Article15. Kim JS, Lee IO, Eoh KJ, Chung YS, Lee I, Lee JY, et al. Surgical technique for single-port laparoscopy in huge ovarian tumors: SW Kim’s technique and comparison to laparotomy. Obstet Gynecol Sci. 2017; 60:178–86.
Article16. Rosenbaum PR, Rubin DB. Reducing bias in observational studies using subclassification on the propensity score. J Am Stat Assoc. 1984; 79:516–24.
Article17. Deeks JJ, Dinnes J, D’Amico R, Sowden AJ, Sakarovitch C, Song F, et al. Evaluating non-randomised intervention studies. Health Technol Assess. 2003; 7:iii–x.
Article18. Thoemmes F. Propensity score matching in SPSS. arXiv. 2012:1201.6385.19. Park JY, Bae J, Lim MC, Lim SY, Seo SS, Kang S, et al. Laparoscopic and laparotomic staging in stage I epithelial ovarian cancer: a comparison of feasibility and safety. Int J Gynecol Cancer. 2008; 18:1202–9.
Article20. Figurelli J, Bresson L, Narducci F, Katdare N, Coulon P, Fournier C, et al. Single-port access laparoscopic surgery in gynecologic oncology: outcomes and feasibility. Int J Gynecol Cancer. 2014; 24:1126–32.
Article21. Gallotta V, Petrillo M, Conte C, Vizzielli G, Fagotti A, Ferrandina G, et al. Laparoscopic versus laparotomic surgical staging for early-stage ovarian cancer: a case-control study. J Minim Invasive Gynecol. 2016; 23:769–74.
Article22. Kim MS, Choi CH, Lee JW, Kim BG, Bae DS, Kim TJ. Comparison between laparoendoscopic single-site and conventional laparoscopic surgery in mature cystic teratoma of the ovary. Gynecol Minim Invasive Ther. 2019; 8:155–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single-port access laparoscopic staging operation for a borderline ovarian tumor
- Comparison of laparoscopy and laparotomy for the management of early-stage ovarian cancer: surgical and oncological outcomes
- Surgical technique for single-port laparoscopy in huge ovarian tumors: SW Kim's technique and comparison to laparotomy
- Early port-site metastasis during neoadjuvant chemotherapy in advanced stage ovarian cancer: report of two cases
- Single-port laparoscopic transperitoneal infrarenal para-aortic lymphadenectomy as part of staging operation for early ovarian cancer and high grade endometrial cancer