Obstet Gynecol Sci.
2017 Mar;60(2):178-186. 10.5468/ogs.2017.60.2.178.
Surgical technique for single-port laparoscopy in huge ovarian tumors: SW Kim's technique and comparison to laparotomy
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Women's Cancer Center, Yonsei Cancer Center, Institute of Women's Life Medical Science, Yonsei University College of Medicine, Seoul, Korea. san1@yuhs.ac
- KMID: 2372802
- DOI: http://doi.org/10.5468/ogs.2017.60.2.178
Abstract
OBJECTIVE
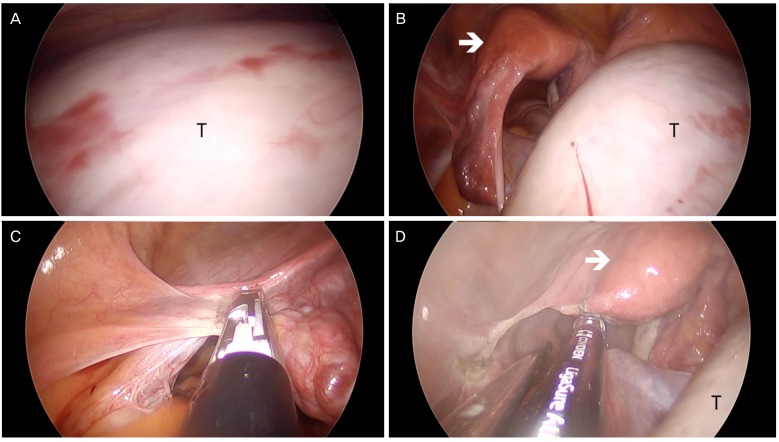
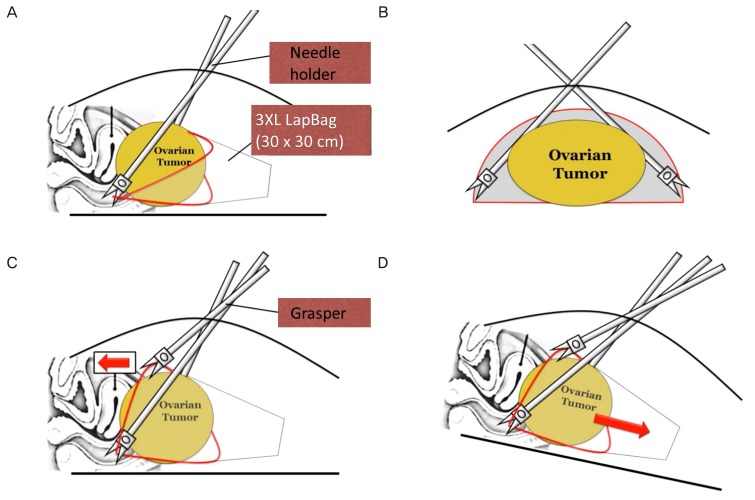
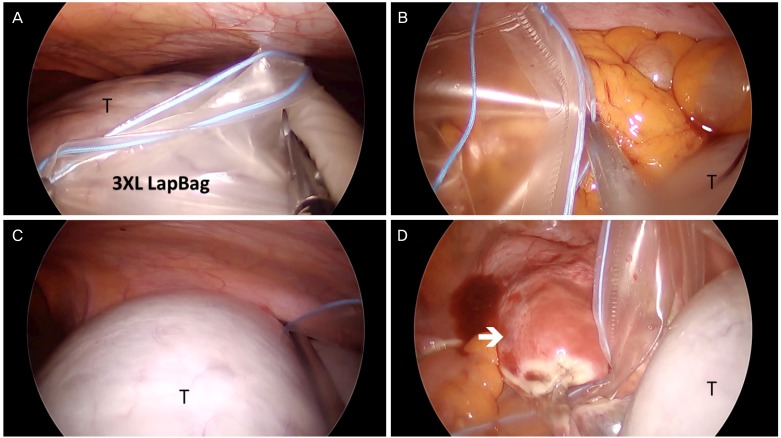
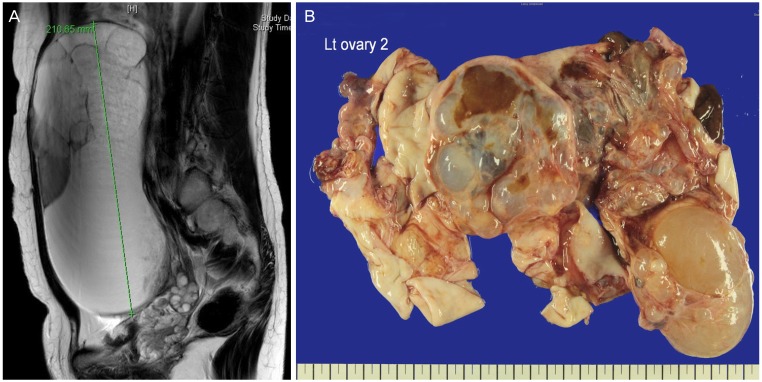
This study aimed to introduce a method to remove huge ovarian tumors (≥15 cm) intact with single-port laparoscopic surgery (SPLS) using SW Kim's technique and to compare the surgical outcomes with those of laparotomy.
METHODS
Medical records were retrospectively reviewed for patients who underwent either SPLS (n=21) with SW Kim's technique using a specially designed 30×30-cm²-sized 3XL LapBag or laparotomy (n=22) for a huge ovarian tumor from December 2008 to May 2016. Perioperative surgical outcomes were compared.
RESULTS
In 19/21 (90.5%) patients, SPLS was successfully performed without any tumor spillage or conversion to multi-port laparoscopy or laparotomy. There was no significant difference in patient characteristics, including tumor diameter and total operation time, between both groups. The postoperative hospital stay was significantly shorter for the SPLS group than for the laparotomy group (median, 2 [1 to 5] vs. 4 [3 to 17] days; P<0.001). The number of postoperative general diet build-up days was also significantly shorter for the SPLS group (median, 1 [1 to 4] vs. 3 [2 to 16] days; P<0.001). Immediate post-operative pain score was lower in the SPLS group (median, 2.0 [0 to 8] vs. 4.0 [0 to 8]; P=0.045). Patient-controlled anesthesia was used less in the SPLS group (61.9% vs. 100%).
CONCLUSION
SPLS was successful in removing most large ovarian tumors without rupture and showed quicker recovery and less immediate post-operative pain in comparison to laparotomy. SPLS using SW Kim's technique could be a feasible solution to removing huge ovarian tumors.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of single-port laparoscopy and laparotomy in early ovarian cancer surgical staging
Kyu Hee Cho, Yeon Ju Lee, Kyung Jin Eoh, Yong Jae Lee, Jung-Yun Lee, Eun Ji Nam, Sunghoon Kim, Young Tae Kim, Sang Wun Kim
Obstet Gynecol Sci. 2021;64(1):90-98. doi: 10.5468/ogs.20216.
Reference
-
1. Fagotti A, Bottoni C, Vizzielli G, Gueli Alletti S, Scambia G, Marana E, et al. Postoperative pain after conventional laparoscopy and laparoendoscopic single site surgery (LESS) for benign adnexal disease: a randomized trial. Fertil Steril. 2011; 96:255–259. PMID: 21565338.
Article2. Nieboer TE, Johnson N, Lethaby A, Tavender E, Curr E, Garry R, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2009; (3):CD003677. PMID: 19588344.
Article3. Sassone AM, Timor-Tritsch IE, Artner A, Westhoff C, Warren WB. Transvaginal sonographic characterization of ovarian disease: evaluation of a new scoring system to predict ovarian malignancy. Obstet Gynecol. 1991; 78:70–76. PMID: 2047071.4. Chong GO, Hong DG, Lee YS. Single-port (OctoPort) assisted extracorporeal ovarian cystectomy for the treatment of large ovarian cysts: compare to conventional laparoscopy and laparotomy. J Minim Invasive Gynecol. 2015; 22:45–49. PMID: 24928739.
Article5. Chua YD, Ng YW, Fong YF. Laparoendoscopic single-site surgery (LESS) for a large ovarian tumour: first clinical case report. Minim Invasive Surg. 2011; 2011:105643. PMID: 22091357.
Article6. Garg P, Misra S, Thakur JD, Song J. Single incision laparoscopic surgery ovarian cystectomy in large benign ovarian cysts using conventional instruments. J Minim Access Surg. 2011; 7:232–235. PMID: 22022112.
Article7. Roh HJ, Lee SJ, Ahn JW, Kwon YS, Cho HJ, Kim DY. Single-port-access, hand-assisted laparoscopic surgery for benign large adnexal tumors versus single-port pure laparoscopic surgery for adnexal tumors. Surg Endosc. 2012; 26:693–703. PMID: 22038160.
Article8. Song T, Kim MK, Kim ML, Yoon BS, Seong SJ. Laparoendoscopic single-site surgery for extremely large ovarian cysts: a feasibility, safety, and patient satisfaction study. Gynecol Obstet Invest. 2014; 78:81–87. PMID: 24969078.
Article9. Takeda A, Imoto S, Mori M, Yamada J, Nakamura H. Management of large adnexal tumors by isobaric laparoendoscopic single-site surgery with a wound retractor. Eur J Obstet Gynecol Reprod Biol. 2013; 166:185–189. PMID: 23122034.
Article10. Fagotti A, Bottoni C, Vizzielli G, Rossitto C, Tortorella L, Monterossi G, et al. Laparoendoscopic single-site surgery (LESS) for treatment of benign adnexal disease: single-center experience over 3-years. J Minim Invasive Gynecol. 2012; 19:695–700. PMID: 23084672.
Article11. Yim GW, Lee M, Nam EJ, Kim S, Kim YT, Kim SW. Is single-port access laparoscopy less painful than conventional laparoscopy for adnexal surgery? A comparison of postoperative pain and surgical outcomes. Surg Innov. 2013; 20:46–54. PMID: 22410390.
Article12. Goh SM, Yam J, Loh SF, Wong A. Minimal access approach to the management of large ovarian cysts. Surg Endosc. 2007; 21:80–83. PMID: 16960678.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single-port access laparoscopic staging operation for a borderline ovarian tumor
- A Prospective Comparison Study of the Two-port and Three Port Techniques for Performing Laparoscopic Cholecystectomy
- Laparoscopic Conservative Surgery of One Case of Ovarian Pregnancy
- Two-port access versus four-port access laparoscopic ovarian cystectomy
- Single port laparoscopic surgery in gynecologic field