J Gynecol Oncol.
2011 Jun;22(2):127-130. 10.3802/jgo.2011.22.2.127.
Single-port access laparoscopic staging operation for a borderline ovarian tumor
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. dsbae@skku.com
- KMID: 2288577
- DOI: http://doi.org/10.3802/jgo.2011.22.2.127
Abstract
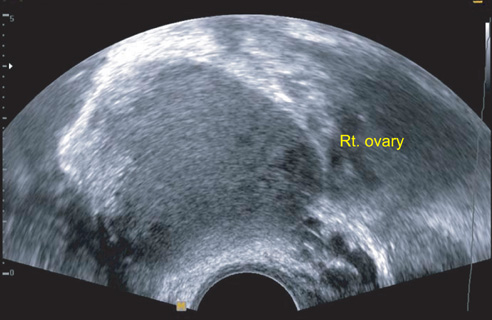
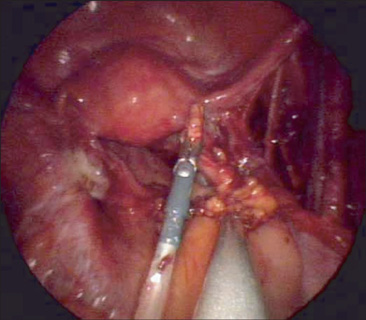
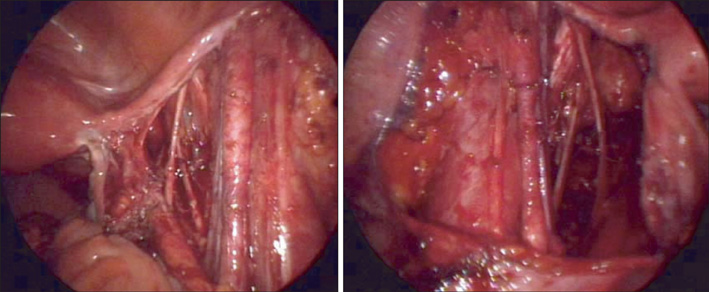
- Minimally invasive surgery is widely used in benign gynecologic diseases and may be used in malignancies. We performed a single-port access laparoscopy staging - bilateral salpingo-oophorectomy, laparoscopy-assisted vaginal hysterectomy, bilateral pelvic lymphadenectomy, infracolic omentectomy, and washing cytology - in a borderline ovarian tumor. The number of harvested pelvic lymph nodes were twenty-three and there were no intraoperative or postoperative complications. Single-port access laparoscopic staging may be performed in selected patients. The efficacy, safety, and potential benefits of this technique should be evaluated in further trials.
MeSH Terms
Figure
Reference
-
1. Leiserowitz GS, Xing G, Parikh-Patel A, Cress R, Abidi A, Rodriguez AO, et al. Laparoscopic versus abdominal hysterectomy for endometrial cancer: comparison of patient outcomes. Int J Gynecol Cancer. 2009. 19:1370–1376.2. Sobiczewski P, Bidzinski M, Derlatka P, Panek G, Danska-Bidzinska A, Gmyrek L, et al. Early cervical cancer managed by laparoscopy and conventional surgery: comparison of treatment results. Int J Gynecol Cancer. 2009. 19:1390–1395.3. Ghezzi F, Cromi A, Uccella S, Bergamini V, Tomera S, Franchi M, et al. Laparoscopy versus laparotomy for the surgical management of apparent early stage ovarian cancer. Gynecol Oncol. 2007. 105:409–413.4. Kim TJ, Lee YY, Kim MJ, Kim CJ, Kang H, Choi CH, et al. Single port access laparoscopic adnexal surgery. J Minim Invasive Gynecol. 2009. 16:612–615.5. Kim TJ, Lee YY, Cha HH, Kim CJ, Choi CH, Lee JW, et al. Single-port-access laparoscopic-assisted vaginal hysterectomy versus conventional laparoscopic-assisted vaginal hysterectomy: a comparison of perioperative outcomes. Surg Endosc. 2010. 24:2248–2252.6. Lee YY, Kim TJ, Kim CJ, Park HS, Choi CH, Lee JW, et al. Single port access laparoscopic adnexal surgery versus conventional laparoscopic adnexal surgery: a comparison of peri-operative outcomes. Eur J Obstet Gynecol Reprod Biol. 2010. 151:181–184.7. Fader AN, Escobar PF. Laparoendoscopic single-site surgery (LESS) in gynecologic oncology: technique and initial report. Gynecol Oncol. 2009. 114:157–161.8. Querleu D, LeBlanc E. Laparoscopic infrarenal paraaortic lymph node dissection for restaging of carcinoma of the ovary or fallopian tube. Cancer. 1994. 73:1467–1471.9. Paek J, Nam EJ, Jung YW, Lee SH, Kim JH, Kim YT, et al. Two-port access staging laparoscopy for gynecologic cancers: a pilot study. J Laparoendosc Adv Surg Tech A. 2010. 20:347–353.10. Charoenkwan K, Kietpeerakool C. Retroperitoneal drainage versus no drainage after pelvic lymphadenectomy for the prevention of lymphocyst formation in patients with gynaecological malignancies. Cochrane Database Syst Rev. 2010. (1):CD007387.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Techniques of gynecologic single-port access laparoscopic surgery
- A case of port site implantation of borderline mucinous tumor of ovary after the laparoscopic operation
- Two-port access versus four-port access laparoscopic ovarian cystectomy
- Single port transumbilical total laparoscopic hysterectomy (TLH): initial experience in Korea
- Current management of borderline ovarian tumor