Obstet Gynecol Sci.
2021 Jan;64(1):13-26. 10.5468/ogs.20205.
Role of vitamin D and calcium in the relief of primary dysmenorrhea: a systematic review
- Affiliations
-
- 1Non-communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 2Department of Midwifery, Faculty of Nursing and Midwifery, Tehran Medical Sciences, Islamic Azad University, Tehran, Iran
- 3Midwifery Department, Kurdistan University of Medical Sciences, Sanandaj, Iran
- 4Student Research Committee, School of Nursing and Midwifery, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- KMID: 2511561
- DOI: http://doi.org/10.5468/ogs.20205
Abstract
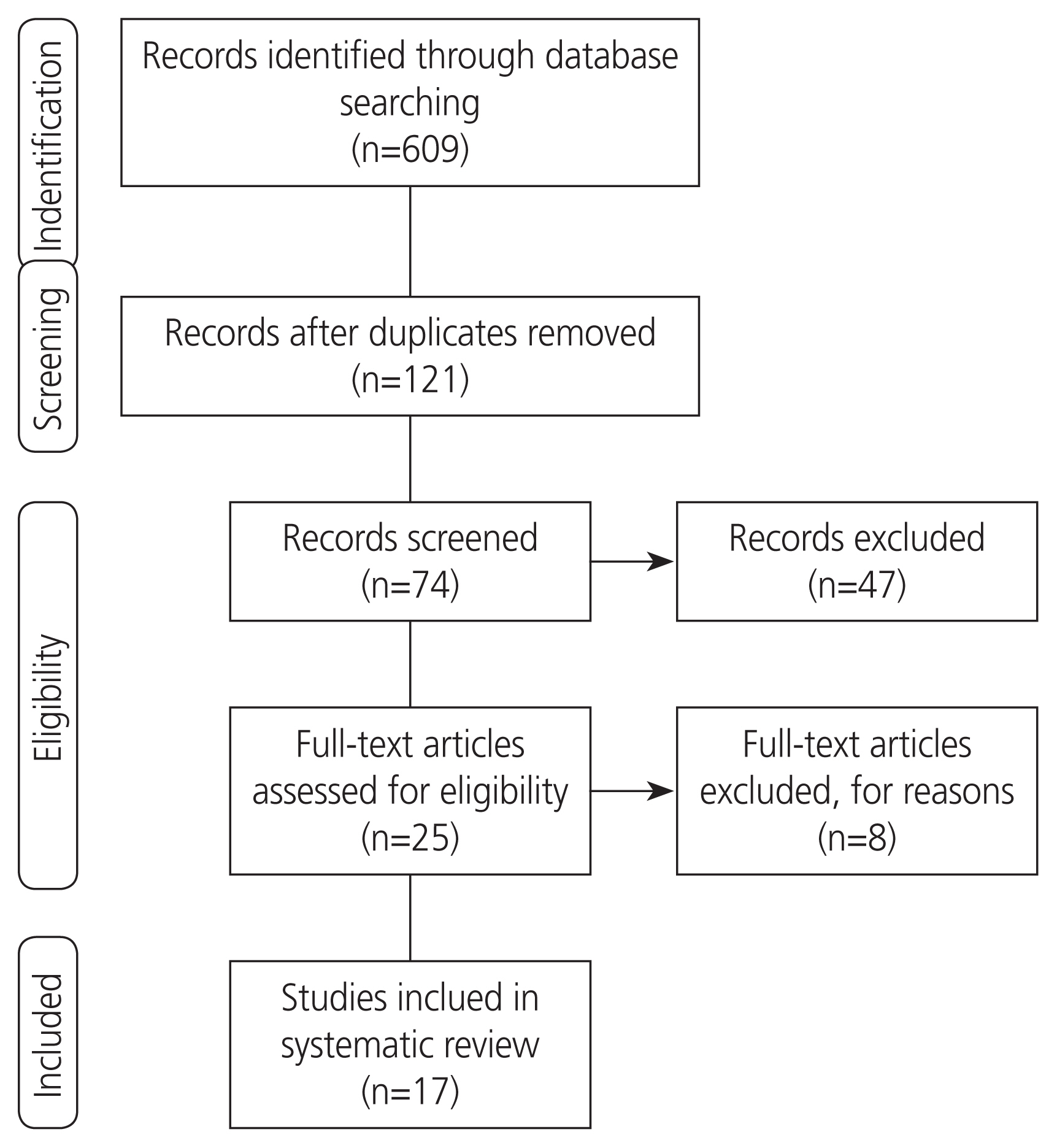
- Dysmenorrhea is one of the well-established problems among women of reproductive age and can have adverse effects on the quality of life of the individual. Some studies suggest a relationship between vitamin D (Vit D) and calcium deficiency and the emergence of early dysmenorrhea. Accordingly, a systematic study was performed to investigate the role of calcium and Vit D in the relief of primary dysmenorrhea. A systematic literature search was performed in PubMed, Web of Science, Scopus, Science Direct, and Google Scholar for papers published between 2010 and 2020. The Consolidated Standards of Reporting Trials and Strengthening the Reporting of Observational Studies in Epidemiology checklists were used to assess the quality of the studies. The risk of bias was assessed using the Cochrane risk-of-bias assessment tool. Low calcium levels lead to an increase in uterine muscle contraction and can cause pain after decreased uterine blood flow. Furthermore, low levels of Vit D can increase primary dysmenorrhea by increasing prostaglandin production or reducing intestinal calcium absorption. That being the case, Vit D and calcium intake can be effective in reducing the severity of primary dysmenorrhea and in reducing the rate of analgesic use. Low levels of Vit D and calcium are inversely related to the severity of primary dysmenorrhea, and Vit D and calcium intake can reduce the severity of primary dysmenorrhea and its associated systemic symptoms. Therefore, the use of calcium and Vit D supplements can be recommended to relieve dysmenorrhea.
Keyword
Figure
Cited by 2 articles
-
Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial
Fatemeh Alsadat Rahnemaei, Ali Gholamrezaei, Maryam Afrakhteh, Farid Zayeri, Mohammad Reza Vafa, Arian Rashidi, Giti Ozgoli
Obstet Gynecol Sci. 2021;64(4):353-363. doi: 10.5468/ogs.20316.Effect of vitamin D vaginal suppository on sexual functioning among postmenopausal women: A three-arm randomized controlled clinical trial
Zinat Sarebani, Venus Chegini, Hui Chen, Ehsan Aali, Monirsadat Mirzadeh, Mohammadreza Abbaspour, Mark D. Griffiths, Zainab Alimoradi
Obstet Gynecol Sci. 2023;66(3):208-220. doi: 10.5468/ogs.22038.
Reference
-
References
1. Bajalan Z, Alimoradi Z, Moafi F. Nutrition as a potential factor of primary dysmenorrhea: a systematic review of observational studies. Gynecol Obstet Invest. 2019; 84:209–24.
Article2. Moini A, Ebrahimi T, Shirzad N, Hosseini R, Radfar M, Bandarian F, et al. The effect of vitamin D on primary dysmenorrhea with vitamin D deficiency: a randomized double-blind controlled clinical trial. Gynecol Endocrinol. 2016; 32:502–5.
Article3. Firouzi M, Zahedifard T, Salari P, Mazlom S. Comparing the pattern of primary dysmenorrhea before and after childbirth. J Midwifery Reprod Health. 2019; 7:1514–21.4. Azagew AW, Kassie DG, Walle TA. Prevalence of primary dysmenorrhea, its intensity, impact and associated factors among female students’ at Gondar town preparatory school, Northwest Ethiopia. BMC Womens Health. 2020; 20:5.
Article5. Monday I, Anthony P, Olunu E, Otohinoyi D, Abiodun S, Owolabi A, et al. Prevalence and correlation between diet and dysmenorrhea among high-school and college students in Saint Vincent and Grenadines. Open Access Maced J Med Sci. 2019; 7:920–4.6. Chen L, Tang L, Guo S, Kaminga AC, Xu H. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019; 9:e026813.
Article7. Vlachou E, Owens DA, Lavdaniti M, Kalemikerakis J, Evagelou E, Margari N, et al. Prevalence, wellbeing, and symptoms of dysmenorrhea among university nursing students in Greece. Diseases. 2019; 7:1–14.
Article8. Femi-Agboola DM, Sekoni OO, Goodman OO. Dysmenorrhea and its effects on school absenteeism and school activities among adolescents in selected secondary schools in Ibadan, Nigeria. Niger Med J. 2017; 58:143–8.
Article9. Acheampong K, Baffour-Awuah D, Ganu D, Appiah S, Pan X, Kaminga A, et al. Prevalence and predictors of dysmenorrhea, its effect, and coping mechanisms among adolescents in Shai Osudoku District, Ghana. Obstet Gynecol Int. 2019; 2019:5834159.
Article10. Kazama M, Maruyama K, Nakamura K. Prevalence of dysmenorrhea and its correlating lifestyle factors in Japanese female junior high school students. Tohoku J Exp Med. 2015; 236:107–13.
Article11. Al-Matouq S, Al-Mutairi H, Al-Mutairi O, Abdulaziz F, Al-Basri D, Al-Enzi M, et al. Dysmenorrhea among high-school students and its associated factors in Kuwait. BMC Pediatr. 2019; 19:80.
Article12. Sidi I, Hounkpatin B, Obossou AAA, Salifou K, Vodouhe M, Denakpo J, et al. Primary dysmenorrhea in the schools of Parakou: prevalence, impact and therapeutic approach. Gynecol Obstet (Sunnyvale). 2016; 6:376.13. Aktaş D. Prevalence and factors affecting dysmenorrhea in female university students: effect on general comfort level. Pain Manag Nurs. 2015; 16:534–43.
Article14. Arafa AE, Senosy SA, Helmy HK, Mohamed AA. Prevalence and patterns of dysmenorrhea and premenstrual syndrome among Egyptian girls (12–25 years). Middle East Fertil Soc J. 2018; 23:486–90.15. Habibi N, Huang MS, Gan WY, Zulida R, Safavi SM. Prevalence of primary dysmenorrhea and factors with its intensity among undergraduate students: a cross sectional study. Pain Manag Nurs. 2015; 16:855–61.16. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015; 21:762–78.
Article17. Salehi A, Marzban M. Effect of foeniculum vulgare on primary dysmenorrhea: a systematic review and meta-analysis. Womens Health Bull Forthcoming. 2018.18. Karacin O, Mutlu I, Kose M, Celik F, Kanat-Pektas M, Yilmazer M. Serum vitamin D concentrations in young Turkish women with primary dysmenorrhea: a randomized controlled study. Taiwan J Obstet Gynecol. 2018; 57:58–63.
Article19. Zarei S, Mohammad-Alizadeh-Charandabi S, Mirghafourvand M, Javadzadeh Y, Effati-Daryani F. Effects of calcium-vitamin d and calcium-alone on pain intensity and menstrual blood loss in women with primary dysmenorrhea: a randomized controlled trial. Pain Med. 2017; 18:3–13.
Article20. Pakniat H, Chegini V, Ranjkesh F, Hosseini MA. Comparison of the effect of vitamin E, vitamin D and ginger on the severity of primary dysmenorrhea: a single-blind clinical trial. Obstet Gynecol Sci. 2019; 62:462–8.
Article21. Abdul-Razzak KK, Ayoub NM, Abu-Taleb AA, Obeidat BA. Influence of dietary intake of dairy products on dysmenorrhea. J Obstet Gynaecol Res. 2010; 36:377–83.
Article22. Rahnemaie FS, Afrakhteh M, Nasiri M, Zayeri F, Vafa M, Ozgoli G. Relationship between serum vitamin D with severity of primary dysmenorrhea and associated systemic symptoms in dormitories students of Shahid Beheshti University of Medical Sciences. Iran J Obstet Gynecol Infertil. 2019; 22:44–53.23. Abdi F, Ozgoli G, Rahnemaie FS. A systematic review of the role of vitamin D and calcium in premenstrual syndrome. Obstet Gynecol Sci. 2019; 62:73–86.
Article24. Rahnemaie FS, Zare E, Zaheri F, Abdi F. Effects of complementary medicine on successful breastfeeding and its associated issues in the postpartum period. Iran J Pediatr. 2019; 29:e80180.
Article25. Zeynali M, Haghighian HK. Is there a relationship between serum vitamin D with dysmenorrhea pain in young women? J Gynecol Obstet Hum Reprod. 2019; 48:711–4.
Article26. Abdul-Razzak KK, Obeidat BA, Al-Farras MI, Dauod AS. Vitamin D and PTH status among adolescent and young females with severe dysmenorrhea. J Pediatr Adolesc Gynecol. 2014; 27:78–82.
Article27. Kucukceran H, Ozdemir O, Kiral S, Berker DS, Kahveci R, Ozkara A, et al. The impact of circulating 25-hydroxyvitamin and oral cholecalciferol treatment on menstrual pain in dysmenorrheic patients. Gynecol Endocrinol. 2019; 35:53–7.
Article28. Bahrami A, Avan A, Sadeghnia HR, Esmaeili H, Tayefi M, Ghasemi F, et al. High dose vitamin D supplementation can improve menstrual problems, dysmenorrhea, and premenstrual syndrome in adolescents. Gynecol Endocrinol. 2018; 34:659–63.
Article29. Ayşegül Ö, Seda A, Şevket O, Özdemir M, İlhan G, Davutoğlu E. A randomized controlled study of vitamin D in the treatment of primary dysmenorrhea. Duzce Med J. 2019; 21:32–6.30. Lama A, Najla A, Azah A, Areej A, Alaa E, Salem A. Vitamin D supplements as adjunctive therapy with analgesics for primary dysmenorrhea: a randomized clinical trial. Int J Reprod Med Gynecol. 2019; 5:004–14.31. Mehrpooya M, Eshraghi A, Rabiee S, Larki-Harchegani A, Ataei S. Comparison the effect of fish-oil and calcium supplementation on treatment of primary dysmenorrhea. Rev Recent Clin Trials. 2017; 12:148–53.
Article32. Charandabi SM, Mirghafourvand M, Chegini S, Javadzadeh Y. Calcium with and without magnesium for primary dysmenorrhea: a double-blind randomized placebo controlled trial. Int J Women Health Reprod Sci. 2017; 5:332–8.33. Fareena Begum A. Study of prevalence of vitamin D deficiency in primary dysmenorrhea and administration of a single oral dose of vitamin D to improve primary dysmenorrhea. Coimbatore: Coimbatore Medical College;2017.34. Ataee M, Zangeneh M, Mahboubi M. Cholecalciferol for Primary Dysmenorrhea in a College aged Population—A Clinical Trial. J Biol Todays World. 2015; 4:54–7.
Article35. Zangene M, Veisi F, Nankali A, Rezaei M, Ataee M. Evaluation of the effects of oral vitamin-d for pelvic pain reduction in primary dysmenorrhea. Iran J Obstet Gynecol Infertil. 2014; 16:14–20.36. Lasco A, Catalano A, Benvenga S. Improvement of primary dysmenorrhea caused by a single oral dose of vitamin D: results of a randomized, double-blind, placebo-controlled study. Arch Intern Med. 2012; 172:366–7.
Article37. Thys-Jacobs S. Micronutrients and the premenstrual syndrome: the case for calcium. J Am Coll Nutr. 2000; 19:220–7.
Article38. Thys-Jacobs S, McMahon D, Bilezikian JP. Cyclical changes in calcium metabolism across the menstrual cycle in women with premenstrual dysphoric disorder. J Clin Endocrinol Metab. 2007; 92:2952–9.
Article39. DeLuca HF. Overview of general physiologic features and functions of vitamin D. Am J Clin Nutr. 2004; 80:1689S–1696S.
Article40. Anagnostis P, Karras S, Goulis DG. Vitamin D in human reproduction: a narrative review. Int J Clin Pract. 2013; 67:225–35.
Article41. Moreno J, Krishnan AV, Swami S, Nonn L, Peehl DM, Feldman D. Regulation of prostaglandin metabolism by calcitriol attenuates growth stimulation in prostate cancer cells. Cancer Res. 2005; 65:7917–25.
Article42. Proctor ML, Murphy PA. Herbal and dietary therapies for primary and secondary dysmenorrhoea. Cochrane Database Syst Rev. 2001; CD002124.
Article43. Das B, Prasanna Chandra M, Samanta S, Mallick AK, Sowmya MK. Serum inorganic phosphorus, uric acid, calcium, magnesium and sodium status during uterine changes of menstrual cycle. Int J Biomed Res. 2012; 3:209–13.
Article44. Thys-Jacobs S, Starkey P, Bernstein D, Tian J. Premenstrual Syndrome Study Group. Calcium carbonate and the premenstrual syndrome: effects on premenstrual and menstrual symptoms. Am J Obstet Gynecol. 1998; 179:444–52.
Article45. Marshall WJ, Bangert SK. Clinical chemistry. Edinburgh: Mosby;2008.46. Bertone-Johnson ER. Vitamin D and the occurrence of depression: causal association or circumstantial evidence? Nutr Rev. 2009; 67:481–92.
Article47. Holick MF. Vitamin D: a D-lightful health perspective. Nutr Rev. 2008; 66:S182–94.
Article48. Hashemipour S, Larijani B, Adibi H, Javadi E, Sedaghat M, Pajouhi M, et al. Vitamin D deficiency and causative factors in the population of Tehran. BMC Public Health. 2004; 4:38.
Article49. Krishnan AV, Feldman D. Mechanisms of the anti-cancer and anti-inflammatory actions of vitamin D. Annu Rev Pharmacol Toxicol. 2011; 51:311–36.
Article50. Bertone-Johnson ER, Manson JE. Vitamin d for menstrual and pain-related disorders in women: comment on “improvement of primary dysmenorrhea caused by a single oral dose of vitamin D”. Arch Intern Med. 2012; 172:367–9.51. Maïmoun L, Sultan C. Effect of physical activity on calcium homeostasis and calciotropic hormones: a review. Calcif Tissue Int. 2009; 85:277–86.
Article52. Baird DD, Hill MC, Schectman JM, Hollis BW. Vitamin D and the risk of uterine fibroids. Epidemiology. 2013; 24:447–53.
Article53. Latthe PM, Champaneria R, Khan KS. Dysmenorrhoea. BMJ Clin Evid. 2011; 2011:0813.54. Zamani M, Arab M, Nasrollahi S, Manikashani K. The evaluation of fish oil (Omega-3 fatty acids) efficacy in treatment of primary dysmenorrhea in high school female students in Hamadan. J Gorgan Univ Med Sci. 2005; 7:39–42.55. Sadeghi N, Paknezhad F, Rashidi Nooshabadi M, Kavianpour M, Jafari Rad S, Khadem Haghighian H. Vitamin E and fish oil, separately or in combination, on treatment of primary dysmenorrhea: a double-blind, randomized clinical trial. Gynecol Endocrinol. 2018; 34:804–8.
Article56. Daily JW, Zhang X, Kim DS, Park S. Efficacy of ginger for alleviating the symptoms of primary dysmenorrhea: a systematic review and meta-analysis of randomized clinical trials. Pain Med. 2015; 16:2243–55.
Article57. Rahnama P, Montazeri A, Huseini HF, Kianbakht S, Naseri M. Effect of Zingiber officinale R. rhizomes (ginger) on pain relief in primary dysmenorrhea: a placebo randomized trial. BMC Complement Altern Med. 2012; 12:92.
Article58. Abdi F, Daryani NE, Khorvash F, Yousefi Z. Experiences of individuals with liver cirrhosis a qualitative study. Gastroenterol Nurs. 2015; 38:252–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Concepts of Vitamin D and Calcium in the Healing of Fractures
- Cardiovascular Impact of Calcium and Vitamin D Supplements: A Narrative Review
- Vitamin D and atopic dermatitis
- Dysmenorrhea and Relief Methods in Woman Nursing Students
- Vitamin D supplementation for primary dysmenorrhea: a double-blind, randomized, placebo-controlled trial