Inside Plastic Stents versus Metal Stents for Treating Unresectable Malignant Perihilar Biliary Obstructions: A Retrospective Comparative Study
- Affiliations
-
- 1Department of Gastroenterology, Sendai City Medical Center, Sendai, Japan
- 2Natori Chuo Clinic, Sendai, Japan
- KMID: 2511234
- DOI: http://doi.org/10.5946/ce.2020.003
Abstract
- Background/Aims
The aim of this study was to evaluate outcomes of inside plastic stents (iPSs) versus those of metal stents (MSs) for treating unresectable perihilar malignant obstructions.
Methods
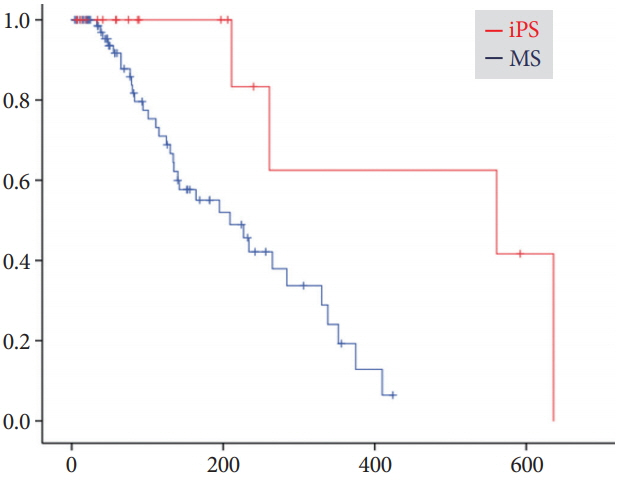
For all patients who underwent endoscopic suprapapillary placement of iPS(s) or MS(s) as the first permanent biliary drainage for unresectable malignant perihilar obstructions between January 2014 and August 2019, clinical outcomes using iPSs (n=20) and MSs (n=85), including clinical efficacy, adverse events, and time to recurrence of biliary obstruction (RBO), were retrospectively evaluated.
Results
There were no differences in clinical effectiveness (95% for the iPS group vs. 92% for the MS group, p=1.00). Procedure-related adverse events, including pancreatitis, acute cholangitis, acute cholecystitis, and death, were observed for 8% of the MS group, although no patient in the iPS group developed such adverse events. The median time to RBO was 561 days (95% confidence interval, 0–1,186 days) for iPSs and 209 days (127–291 days) for MSs, showing a significant difference (p=0.008).
Conclusions
Time to RBO after iPS placement was significantly longer than that after MS placement. IPSs, which are removable, unlike MSs, were an acceptable option.
Keyword
Figure
Cited by 3 articles
-
Editors' Choice of Noteworthy Clinical Endoscopy Publications in the First Decade
Gwang Ha Kim, Kwang An Kwon, Do Hyun Park, Jimin Han
Clin Endosc. 2021;54(5):633-640. doi: 10.5946/ce.2021.216.Changing Trends in Biliary Stenting for Unresectable Malignant Perihilar Obstructions
Lubna Kamani, Muhammad Arshad
Clin Endosc. 2020;53(6):636-637. doi: 10.5946/ce.2020.165.The feasibility of percutaneous transhepatic gallbladder aspiration for acute cholecystitis after self-expandable metallic stent placement for malignant biliary obstruction: a 10-year retrospective analysis in a single center
Akihisa Ohno, Nao Fujimori, Toyoma Kaku, Masayuki Hijioka, Ken Kawabe, Naohiko Harada, Makoto Nakamuta, Takamasa Oono, Yoshihiro Ogawa
Clin Endosc. 2022;55(6):784-792. doi: 10.5946/ce.2021.244.
Reference
-
1. Wagner HJ, Knyrim K, Vakil N, Klose KJ. Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy. 1993; 25:213–218.
Article2. Sangchan A, Kongkasame W, Pugkhem A, Jenwitheesuk K, Mairiang P. Efficacy of metal and plastic stents in unresectable complex hilar cholangiocarcinoma: a randomized controlled trial. Gastrointest Endosc. 2012; 76:93–99.
Article3. Mukai T, Yasuda I, Nakashima M, et al. Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J Hepatobiliary Pancreat Sci. 2013; 20:214–222.
Article4. Zorrón Pu L, de Moura EG, Bernardo WM, et al. Endoscopic stenting for inoperable malignant biliary obstruction: a systematic review and meta-analysis. World J Gastroenterol. 2015; 21:13374–13385.5. Kurita A, Kodama Y, Minami R, et al. Endoscopic stent placement above the intact sphincter of Oddi for biliary strictures after living donor liver transplantation. J Gastroenterol. 2013; 48:1097–1104.
Article6. Tsujino T, Isayama H, Kogure H, Sato T, Nakai Y, Koike K. Endoscopic management of biliary strictures after living donor liver transplantation. Clin J Gastroenterol. 2017; 10:297–311.
Article7. Kobayashi N, Watanabe S, Hosono K, et al. Endoscopic inside stent placement is suitable as a bridging treatment for preoperative biliary tract cancer. BMC Gastroenterol. 2015; 15:8.
Article8. Kaneko T, Sugimori K, Shimizu Y, et al. Efficacy of plastic stent placement inside bile ducts for the treatment of unresectable malignant hilar obstruction (with videos). J Hepatobiliary Pancreat Sci. 2014; 21:349–355.
Article9. Ishiwatari H, Hayashi T, Ono M, Sato T, Kato J. Newly designed plastic stent for endoscopic placement above the sphincter of Oddi in patients with malignant hilar biliary obstruction. Dig Endosc. 2013; 25 Suppl 2:94–99.
Article10. Inatomi O, Bamba S, Shioya M, et al. Threaded biliary inside stents are a safe and effective therapeutic option in cases of malignant hilar obstruction. BMC Gastroenterol. 2013; 13:31.
Article11. Kanno Y, Ito K, Koshita S, et al. Soft surface irregularity of malignant perihilar biliary strictures in cholangiography as a risk factor for early dysfunction of multiple metal stents. Dig Liver Dis. 2017; 49:1014–1021.
Article12. Kanno Y, Ito K, Fujita N, et al. Single-session endoscopic bilateral y-configured placement of metal stents for hilar malignant biliary obstruction. Dig Endosc. 2011; 23:91–96.
Article13. Kanno Y, Ito K, Koshita S, et al. EUS-guided biliary drainage for malignant perihilar biliary strictures after further transpapillary intervention has been judged to be impossible or ineffective. Intern Med. 2017; 56:3145–3151.
Article14. Geoghegan JG, Branch MS, Costerton JW, Pappas TN, Cotton PB. Placement of biliary stents above the sphincter of Oddi prolongs stent patency in dogs. Gut. 1991; 32:A1232.15. Pedersen FM, Lassen AT, Schaffalitzky de Muckadell OB. Randomized trial of stent placed above and across the sphincter of Oddi in malignant bile duct obstruction. Gastrointest Endosc. 1998; 48:574–579.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Technical Tips and Issues of Biliary Stenting, Focusing on Malignant Hilar Obstruction
- A Comparative Study on the Efficacy of Covered Metal Stent and Plastic Stent in Malignant Biliary Obstruction
- Bilateral Metallic Stenting in Malignant Hilar Obstruction
- Mechanisms of Biliary Plastic Stent Occlusion and Efforts at Prevention