Clin Endosc.
2020 Nov;53(6):719-726. 10.5946/ce.2019.149.
Positive Fecal Occult Blood Test is a Predictive Factor for Gastrointestinal Bleeding after Capsule Endoscopy in Patients with Unexplained Iron Deficiency Anemia: A Korean Multicenter CAPENTRY Study
- Affiliations
-
- 1Department of Internal Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea
- 3Department of Internal Medicine, School of Medicine, Kyungpook National University, Kyungpook National University Hospital, Daegu, Korea
- 4Department of Internal Medicine, Dongguk University Ilsan Hospital, Goyang, Korea
- 5Department of Internal Medicine, Soonchunhyang University College of Medicine, Seoul, Korea
- 6Department of Internal Medicine and Institute of Gastroenterology, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 8Department of Internal Medicine, Jeju National University School of Medicine, Jeju, Korea
- 9Department of Internal Medicine, Hallym University College of Medicine, Hwasung, Korea
- 10Department of Internal Medicine, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
- KMID: 2511232
- DOI: http://doi.org/10.5946/ce.2019.149
Abstract
- Background/Aims
Capsule endoscopy (CE) is recommended as the primary method for the evaluation of unexplained anemia. This study aimed to assess the diagnostic yield of CE in patients with unexplained iron deficiency anemia (IDA) without overt bleeding, and to evaluate their long-term outcomes and related clinical factors.
Methods
Data of patients who underwent CE for the evaluation of IDA were reviewed from a CE registry in Korea. Additional clinical data were collected by the involved investigators of each hospital through a review of medical records.
Results
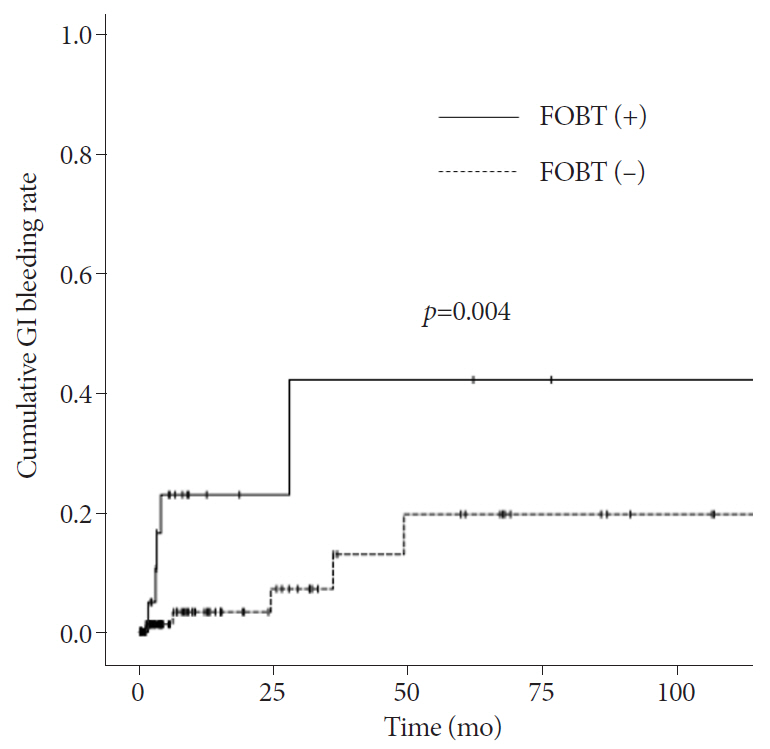
Among a total of 144 patients, the diagnostic yield of CE was 34%. Gastrointestinal (GI) bleeding was found in 6.3% (n=9) of the patients (occult bleeding in four patients and overt bleeding in five patients) during a mean follow-up of 17.8 months. Patients with a positive fecal occult blood test (FOBT) result at the initial diagnosis had a higher rate of GI bleeding after CE (p=0.004). In addition, a positive FOBT result was the only independent predictive factor for GI bleeding (hazard ratio, 5.30; 95% confidence interval, 1.41–19.85; p=0.013).
Conclusions
Positive FOBT is a predictive factor for GI bleeding during follow-up after CE in patients with unexplained IDA without overt bleeding. Thus, patients with positive FOBT need to be more closely followed up.
Keyword
Figure
Reference
-
1. Guralnik JM, Eisenstaedt RS, Ferrucci L, Klein HG, Woodman RC. Prevalence of anemia in persons 65 years and older in the United States: evidence for a high rate of unexplained anemia. Blood. 2004; 104:2263–2268.
Article2. Nissenson AR, Goodnough LT, Dubois RW. Anemia: not just an innocent bystander? Arch Intern Med. 2003; 163:1400–1404.3. Shim KN, Moon JS, Chang DK, et al. Guideline for capsule endoscopy: obscure gastrointestinal bleeding. Clin Endosc. 2013; 46:45–53.
Article4. De Franceschi L, Iolascon A, Taher A, Cappellini MD. Clinical management of iron deficiency anemia in adults: systemic review on advances in diagnosis and treatment. Eur J Intern Med. 2017; 42:16–23.
Article5. Fireman Z, Kopelman Y. The role of video capsule endoscopy in the evaluation of iron deficiency anaemia. Dig Liver Dis. 2004; 36:97–102.
Article6. Zuckerman GR, Prakash C, Askin MP, Lewis BS. AGA technical review on the evaluation and management of occult and obscure gastrointestinal bleeding. Gastroenterology. 2000; 118:201–221.
Article7. Holleran GE, Barry SA, Thornton OJ, Dobson MJ, McNamara DA. The use of small bowel capsule endoscopy in iron deficiency anaemia: low impact on outcome in the medium term despite high diagnostic yield. Eur J Gastroenterol Hepatol. 2013; 25:327–332.8. Min YW, Kim JS, Jeon SW, et al. Long-term outcome of capsule endoscopy in obscure gastrointestinal bleeding: a nationwide analysis. Endoscopy. 2014; 46:59–65.
Article9. Niv Y, Niv G, Wiser K, Demarco DC. Capsule endoscopy - comparison of two strategies of bowel preparation. Aliment Pharmacol Ther. 2005; 22:957–962.
Article10. Arakawa D, Ohmiya N, Nakamura M, et al. Outcome after enteroscopy for patients with obscure GI bleeding: diagnostic comparison between double-balloon endoscopy and videocapsule endoscopy. Gastrointest Endosc. 2009; 69:866–874.
Article11. Pennazio M, Santucci R, Rondonotti E, et al. Outcome of patients with obscure gastrointestinal bleeding after capsule endoscopy: report of 100 consecutive cases. Gastroenterology. 2004; 126:643–653.
Article12. McIntyre AS, Long RG. Prospective survey of investigations in outpatients referred with iron deficiency anaemia. Gut. 1993; 34:1102–1107.
Article13. Milano A, Balatsinou C, Filippone A, et al. A prospective evaluation of iron deficiency anemia in the GI endoscopy setting: role of standard endoscopy, videocapsule endoscopy, and CT-enteroclysis. Gastrointest Endosc. 2011; 73:1002–1008.
Article14. Bermejo F, García-López S. A guide to diagnosis of iron deficiency and iron deficiency anemia in digestive diseases. World J Gastroenterol. 2009; 15:4638–4643.
Article15. Rockey DC. Occult and obscure gastrointestinal bleeding: causes and clinical management. Nat Rev Gastroenterol Hepatol. 2010; 7:265–279.
Article16. Raju GS, Gerson L, Das A, Lewis B. American Gastroenterological Association (AGA) institute medical position statement on obscure gastrointestinal bleeding. Gastroenterology. 2007; 133:1694–1696.
Article17. Law R, Varayil JE, WongKeeSong LM, et al. Assessment of multi-modality evaluations of obscure gastrointestinal bleeding. World J Gastroenterol. 2017; 23:614–621.
Article18. ASGE Standards of Practice Committee, Fisher L, Lee Krinsky M, et al. The role of endoscopy in the management of obscure GI bleeding. Gastrointest Endosc. 2010; 72:471–479.
Article19. Carey EJ, Leighton JA, Heigh RI, et al. A single-center experience of 260 consecutive patients undergoing capsule endoscopy for obscure gastrointestinal bleeding. Am J Gastroenterol. 2007; 102:89–95.
Article20. Ell C, Remke S, May A, Helou L, Henrich R, Mayer G. The first prospective controlled trial comparing wireless capsule endoscopy with push enteroscopy in chronic gastrointestinal bleeding. Endoscopy. 2002; 34:685–689.
Article21. Kobayashi Y, Watabe H, Yamada A, et al. Impact of fecal occult blood on obscure gastrointestinal bleeding: observational study. World J Gastroenterol. 2015; 21:326–332.
Article22. Concha R, Amaro R, Barkin JS. Obscure gastrointestinal bleeding: diagnostic and therapeutic approach. J Clin Gastroenterol. 2007; 41:242–251.23. Calabrese C, Liguori G, Gionchetti P, et al. Obscure gastrointestinal bleeding: single centre experience of capsule endoscopy. Intern Emerg Med. 2013; 8:681–687.
Article24. Katsinelos P, Lazaraki G, Gkagkalis A, et al. The role of capsule endoscopy in the evaluation and treatment of obscure-overt gastrointestinal bleeding during daily clinical practice: a prospective multicenter study. Scand J Gastroenterol. 2014; 49:862–870.
Article25. Koulaouzidis A, Rondonotti E, Giannakou A, Plevris JN. Diagnostic yield of small-bowel capsule endoscopy in patients with iron-deficiency anemia: a systematic review. Gastrointest Endosc. 2012; 76:983–992.
Article26. Tong J, Svarta S, Ou G, Kwok R, Law J, Enns R. Diagnostic yield of capsule endoscopy in the setting of iron deficiency anemia without evidence of gastrointestinal bleeding. Can J Gastroenterol. 2012; 26:687–690.
Article27. Sidhu R, Sanders DS, Kapur K, Leeds JS, McAlindon ME. Factors predicting the diagnostic yield and intervention in obscure gastrointestinal bleeding investigated using capsule endoscopy. J Gastrointestin Liver Dis. 2009; 18:273–278.28. Viazis N, Papaxoinis K, Vlachogiannakos J, Efthymiou A, Theodoropoulos I, Karamanolis DG. Is there a role for second-look capsule endoscopy in patients with obscure GI bleeding after a nondiagnostic first test? Gastrointest Endosc. 2009; 69:850–856.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laparoscopy-assisted Surgical Removal of a Retained Wireless Capsule Endoscopy: A case report
- H. pylori-associated Iron-Deficiency Anemia
- A rare cause of obscure gastrointestinal bleeding: Chronic enteropathy associated with SLCO2A1 mutation in a case from India
- A Case of Small Bowel Polyp Bleeding Diagnosed by Capsule Endoscopy
- Laparoscopic Resection of a Jejunal Inflammatory Fibroid Polyp that Caused Occult Gastrointestinal Bleeding, Diagnosed via Capsule Endoscopy and Double-Balloon Enteroscopy: A Case Report