Korean J Transplant.
2020 Dec;34(4):293-301. 10.4285/kjt.20.0027.
Unification venoplasty of the outflow hepatic vein for laparoscopically harvested left liver grafts in pediatric living donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2510269
- DOI: http://doi.org/10.4285/kjt.20.0027
Abstract
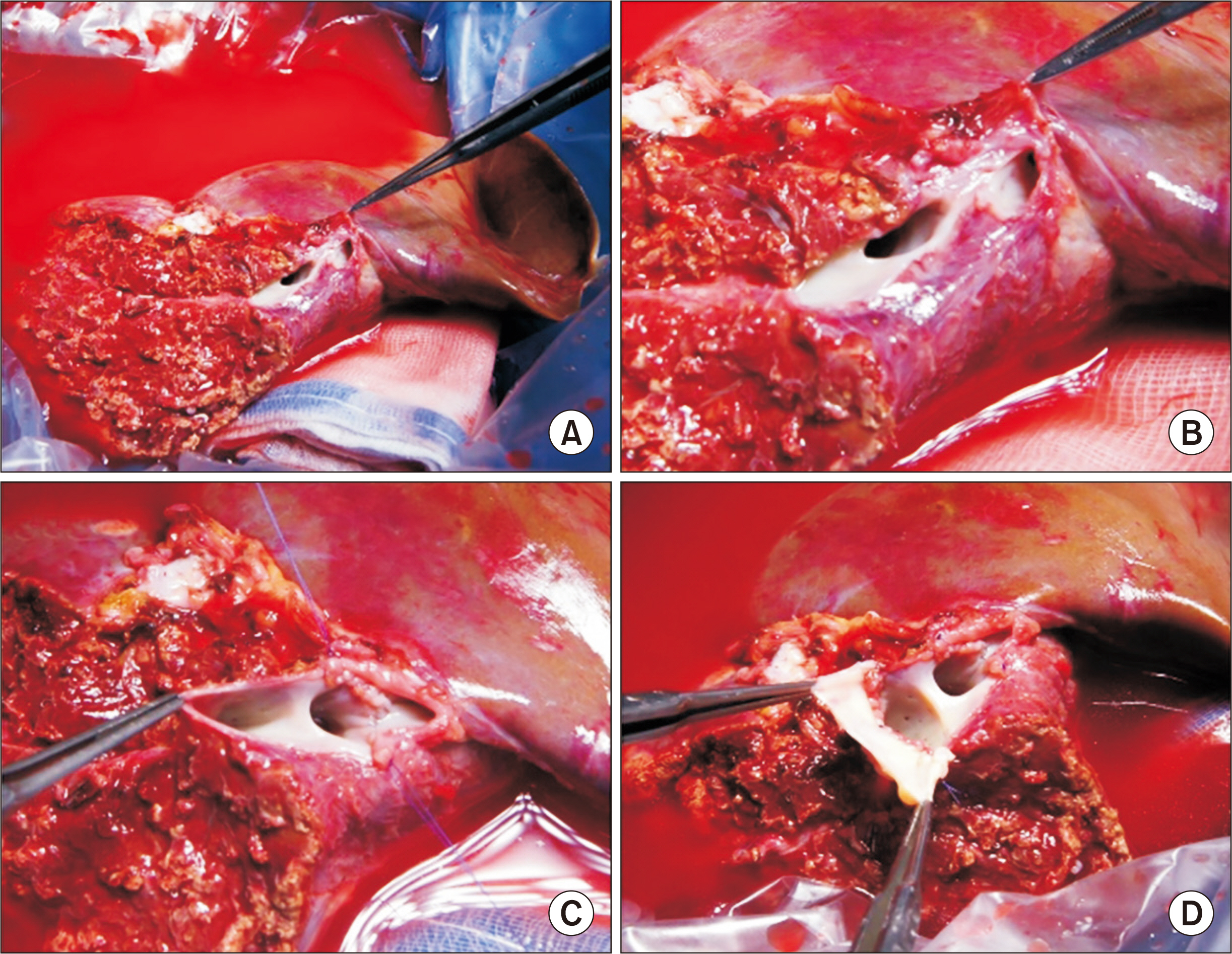
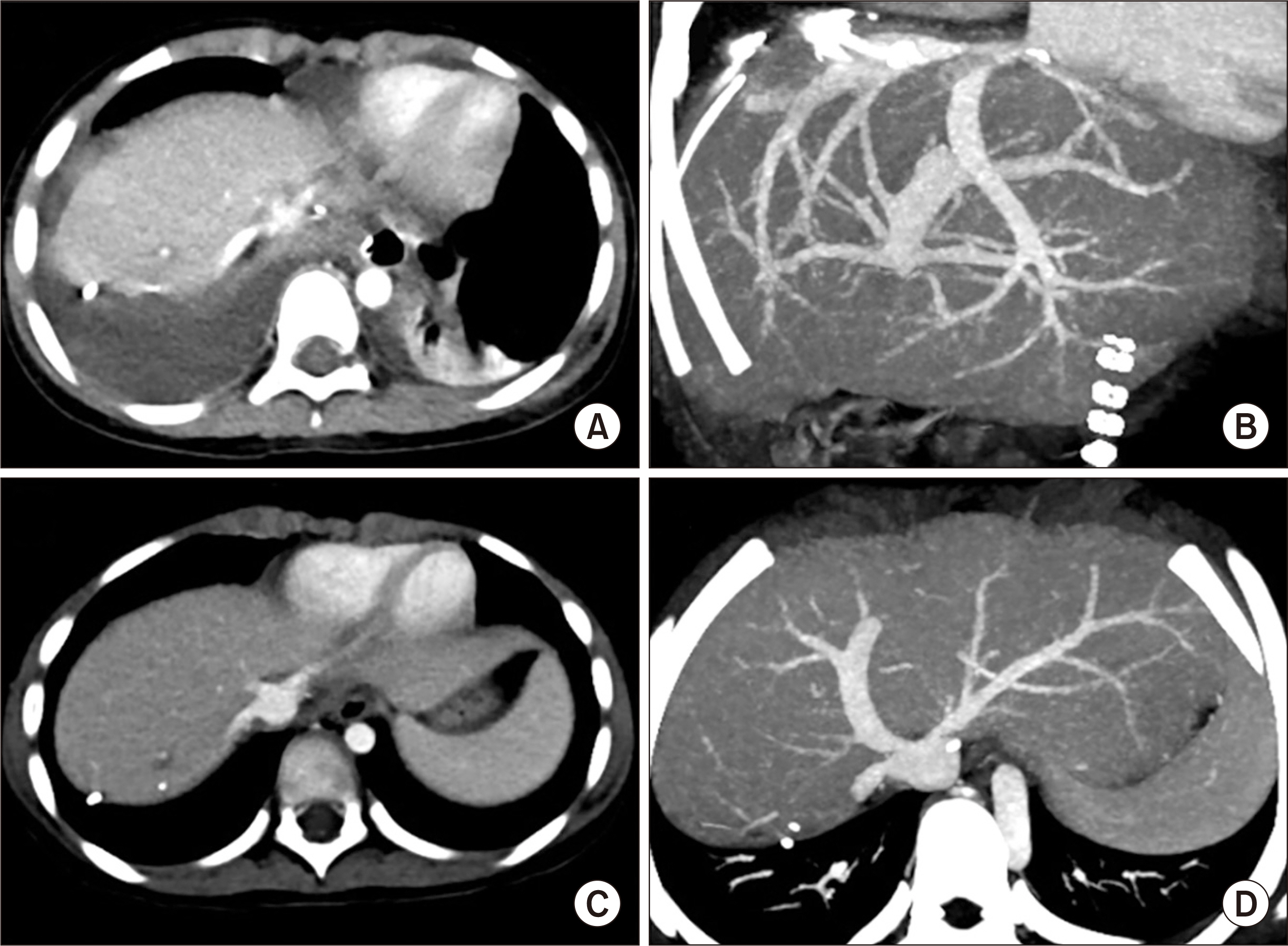
- Laparoscopically harvested left liver (LL) grafts have drawbacks with respect to the size and shape of graft hepatic vein orifices. We present two cases of pediatric living donor liver transplantation (LDLT) using laparoscopically harvested LL grafts and describe refined surgical techniques for graft hepatic vein venoplasty. The first case was a boy aged 4 years and 5 months, with hepatoblastoma. The donor was his 35-year-old mother, and LL graft weighed 315 g. Two separate openings of the graft at the left hepatic vein (LHV) and middle hepatic vein (MHV) were unified through septotomy and septoplasty, and cryopreserved vein homograft patch was attached. Standard procedures of LDLT were performed. This patient recovered uneventfully and has been doing well for 4 years with-out tumor recurrence. The second case was a 6-year-old girl with ornithine transcarbam-ylase deficiency. The donor was her 35-year-old mother, and the LL graft weighed 310 g. Two separate openings of graft MHV, with segment III and segment II veins, were unified through septoplasty, and vein patch was attached. Standard procedures of LDLT were performed. This patient has been doing well for 4 years. In conclusion, separate graft he-patic vein openings are a drawback of laparoscopically harvested LL grafts, which thus require unification venoplasty of customized design individually tailored for LL graft and pediatric recipient.
Figure
Reference
-
1. Scatton O, Katsanos G, Boillot O, Goumard C, Bernard D, Stenard F, et al. 2015; Pure laparoscopic left lateral sectionectomy in living donors: from innovation to development in France. Ann Surg. 261:506–12. DOI: 10.1097/SLA.0000000000000642. PMID: 24646560.2. Broering DC, Elsheikh Y, Shagrani M, Abaalkhail F, Troisi RI. 2018; Pure laparoscopic living donor left lateral sectionectomy in pediatric transplantation: a propensity score analysis on 220 consecutive patients. Liver Transpl. 24:1019–30. DOI: 10.1002/lt.25043. PMID: 29489071.
Article3. Gautier S, Monakhov A, Gallyamov E, Tsirulnikova O, Zagaynov E, Dzhanbekov T, et al. 2018; Laparoscopic left lateral section procurement in living liver donors: a single center propensity score-matched study. Clin Transplant. 32:e13374. DOI: 10.1111/ctr.13374. PMID: 30080281.
Article4. Soubrane O, de Rougemont O, Kim KH, Samstein B, Mamode N, Boillot O, et al. 2015; Laparoscopic living donor left lateral sectionectomy: a new standard practice for donor hepatectomy. Ann Surg. 262:757–61. DOI: 10.1097/SLA.0000000000001485. PMID: 26583663.5. Almodhaiberi H, Kim SH, Kim KH. 2018; Totally laparoscopic living donor left hepatectomy for liver transplantation in a child. Surg Endosc. 32:513. DOI: 10.1007/s00464-017-5692-9. PMID: 28717867.
Article6. Kim KH, Jung DH, Park KM, Lee YJ, Kim DY, Kim KM, et al. 2011; Comparison of open and laparoscopic live donor left lateral sectionectomy. Br J Surg. 98:1302–8. DOI: 10.1002/bjs.7601. PMID: 21717424.
Article7. Hwang S, Ha TY, Ahn CS, Moon DB, Kim KH, Song GW, et al. 2016; Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion. Korean J Hepatobiliary Pancreat Surg. 20:97–101. DOI: 10.14701/kjhbps.2016.20.3.97. PMID: 27621745. PMCID: PMC5018955.
Article8. Hwang S, Lee SG, Ahn CS, Moon DB, Kim KH, Sung KB, et al. 2010; Morphometric and simulation analyses of right hepatic vein reconstruction in adult living donor liver transplantation using right lobe grafts. Liver Transpl. 16:639–48. DOI: 10.1002/lt.22045. PMID: 20440773.
Article9. Hwang S, Lee SG, Ha TY, Ahn CS, Park KM, Kim KH, et al. 2004; Simplified standardized technique for living donor liver transplantation using left liver graft plus caudate lobe. Liver Transpl. 10:1398–405. DOI: 10.1002/lt.20241. PMID: 15497157.
Article10. Hwang S, Lee SG, Ha TY, Ahn CS, Park KM, Kim KH, et al. 2006; Feasibility assessment for tailoring preservation of segment VIII hepatic vein during left liver graft procurement. Hepatogastroenterology. 53:928–32. PMID: 17153455.11. Imamura H, Makuuchi M, Sakamoto Y, Sugawara Y, Sano K, Nakayama A, et al. 2000; Anatomical keys and pitfalls in living donor liver transplantation. J Hepatobiliary Pancreat Surg. 7:380–94. DOI: 10.1007/s005340070033. PMID: 11180859.
Article12. Namgoong JM, Hwang S, Park GC, Kwon H, Kwon YJ, Kim SH. 2020; Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft. Ann Hepatobiliary Pancreat Surg. 24:326–32. DOI: 10.14701/ahbps.2020.24.3.326. PMID: 32843600. PMCID: PMC7452796.
Article13. Kwon H, Kwon H, Hong JP, Han Y, Park H, Song GW, et al. 2015; Use of cryopreserved cadaveric arterial allograft as a vascular conduit for peripheral arterial graft infection. Ann Surg Treat Res. 89:51–4. DOI: 10.4174/astr.2015.89.1.51. PMID: 26131446. PMCID: PMC4481033.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center
- Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Graft outflow vein venoplasty for a laparoscopically harvested left lateral section graft in pediatric living donor liver transplantation
- Modified left liver graft with funneling venoplasty of middle hepatic vein branches for pediatric living donor liver transplantation
- Quilt unification venoplasty of the right hepatic veins enabling double inferior vena cava anastomosis in living donor liver transplantation using a right liver graft