Graft outflow vein unification venoplasty with superficial left hepatic vein branch in pediatric living donor liver transplantation using a left lateral section graft
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2505346
- DOI: http://doi.org/10.14701/ahbps.2020.24.3.326
Abstract
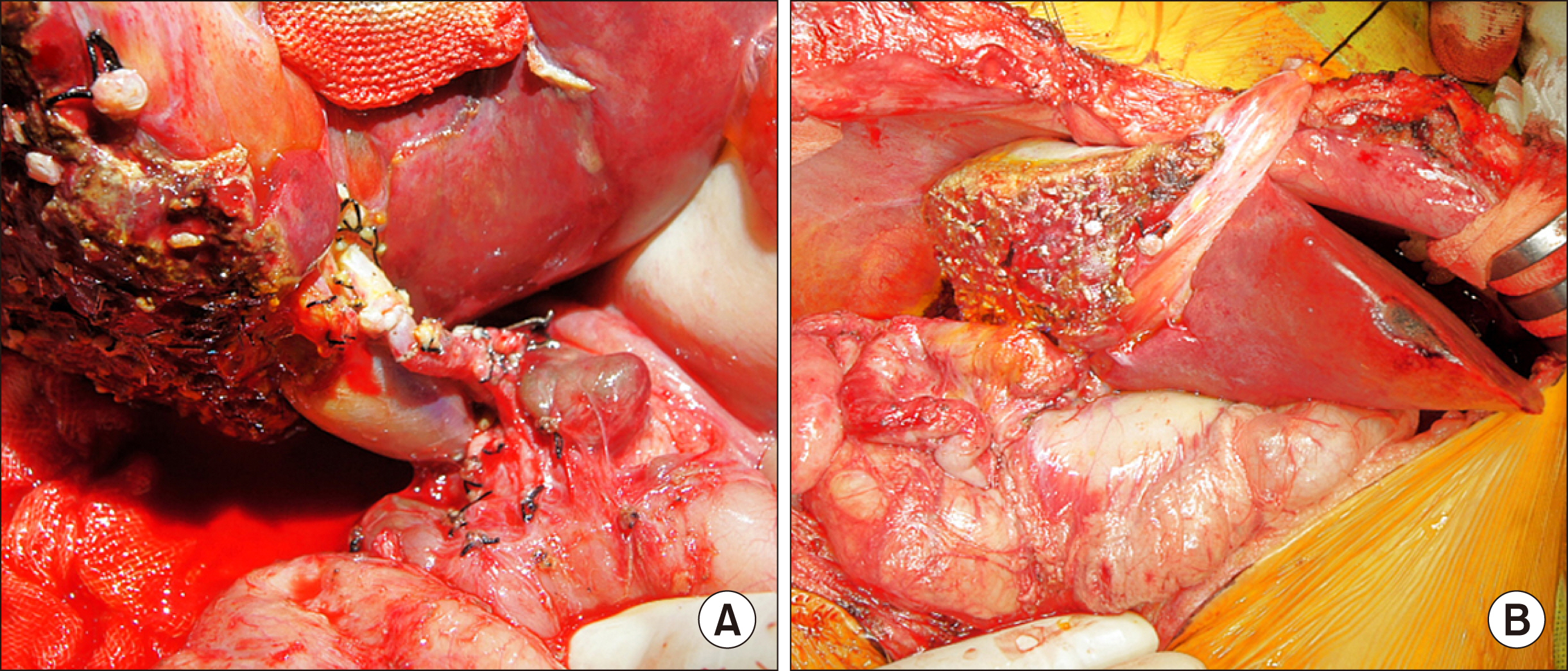
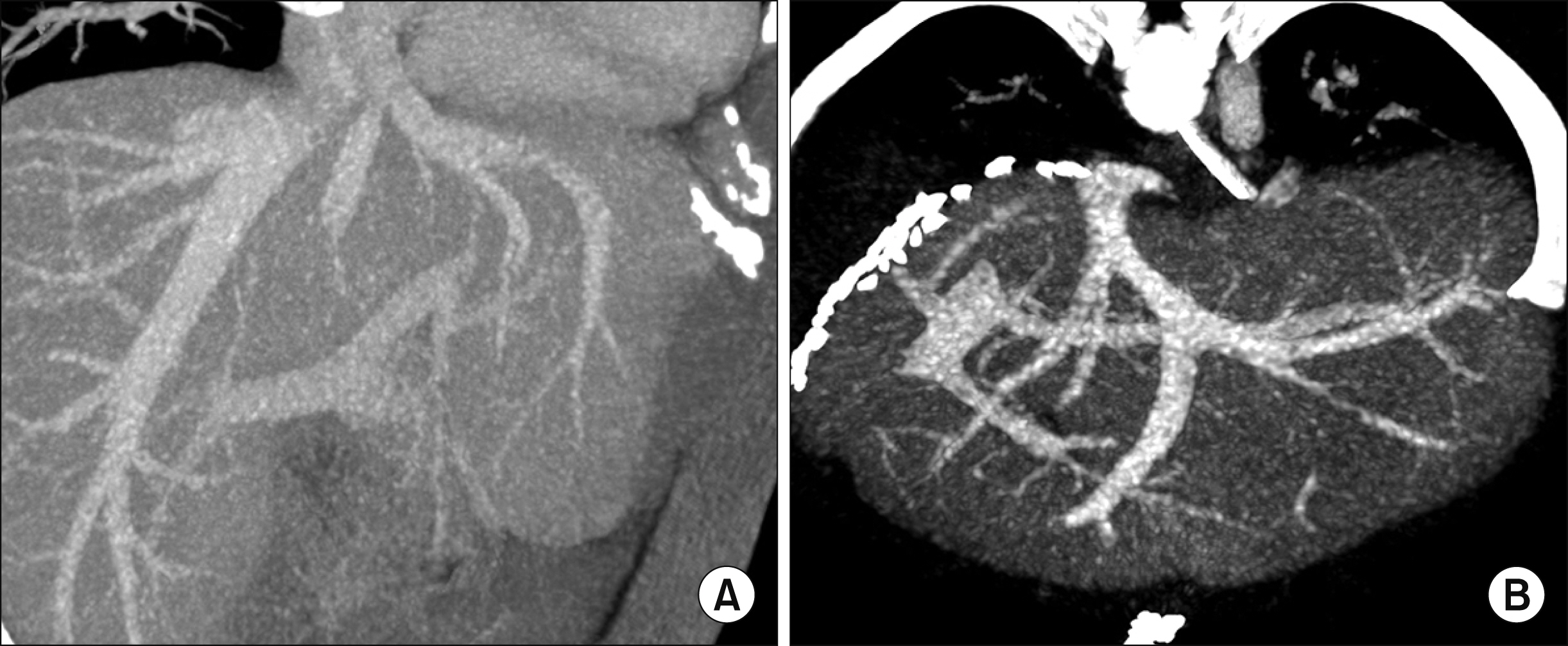
- Orifice size of the left hepatic vein trunk (LHV) in left lateral segment (LLS) grafts is often too small to perform direct anastomosis. A small superficial branch of LHV is encountered in approximately 30% of LLS grafts. Unification venoplasty of the LHV trunk and its superficial vein branch makes the orifice size of LLS outflow vein larger than the original size. We present refined surgical techniques for LHV unification venoplasty with a superficial LHV branch. The patient was a 5-month-old 9 kg-weighing girl with biliary atresia. Her general condition deteriorated, but there was low possibility of deceased donor liver allocation, thus living donor liver transplantation was performed using her mother’s LLS. The graft hepatic vein was widened through unification venoplasty of LHV and its superficial branch. Recipient hepatic vein orifice was widened through unification of three hepatic veins. The graft and recipient hepatic vein orifices were well matched in size, and they were anastomosed with 5-0 continuous sutures. The portal vein was reconstructed with interposition of cold-preserved external iliac vein homograft. The graft left hepatic artery was reconstructed using the recipient right hepatic artery and hepaticojejunostomy was performed. This patient recovered uneventfully and is doing well for 3 months to date. The unification venoplasty with LHV trunk and its superficial vein branch makes the size of LLS outflow vein definitely larger than the original size, thus it can be a useful technical option to reduce the risk of hepatic vein outflow obstruction in pediatric liver transplantation using a LLS graft.
Figure
Cited by 3 articles
-
Pediatric liver transplantation with hyperreduced left lateral segment graft
Jung-Man Namgoong, Shin Hwang, Gi-Won Song, Dae-Yeon Kim, Tae-Yong Ha, Dong-Hwan Jung, Gil-Chun Park, Chul-Soo Ahn, Kyung Mo Kim, Seak Hee Oh, Hyunhee Kwon, Yong Jae Kwon
Ann Hepatobiliary Pancreat Surg. 2020;24(4):503-512. doi: 10.14701/ahbps.2020.24.4.503.Unification venoplasty of the outflow hepatic vein for laparoscopically harvested left liver grafts in pediatric living donor liver transplantation
Jung-Man Namgoong, Shin Hwang, Ki-Hun Kim, Gil-Chun Park, Kyung Mo Kim, Seak Hee Oh, Hwui-Dong Cho, Hyunhee Kwon, Yong Jae Kwon
Korean J Transplant. 2020;34(4):293-301. doi: 10.4285/kjt.20.0027.Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation
Jung-Man Namgoong, Shin Hwang, Young-In Yoon, Yong-Pil Cho, Woo-Hyoung Kang, Yong Jae Kwon, Hyunhee Kwon, Sang Hoon Kim, Kyung Mo Kim, Seak Hee Oh
Ann Hepatobiliary Pancreat Surg. 2021;25(2):299-306. doi: 10.14701/ahbps.2021.25.2.299.
Reference
-
1. Karakayali H, Boyvat F, Coskun M, Isiklar I, Sözen H, Filik L, et al. 2006; Venous complications after orthotopic liver transplantation. Transplant Proc. 38:604–606. DOI: 10.1016/j.transproceed.2006.01.011. PMID: 16549187.
Article2. Hwang S, Lee SG, Choi ST, Moon DB, Ha TY, Lee YJ, et al. 2005; Hepatic vein anatomy of the medial segment for living donor liver transplantation using extended right lobe graft. Liver Transpl. 11:449–455. DOI: 10.1002/lt.20387. PMID: 15776411.
Article3. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–258. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article4. Galloux A, Pace E, Franchi-Abella S, Branchereau S, Gonzales E, Pariente D. 2018; Diagnosis, treatment and outcome of hepatic venous outflow obstruction in paediatric liver transplantation: 24-year experience at a single centre. Pediatr Radiol. 48:667–679. DOI: 10.1007/s00247-018-4079-y. PMID: 29468367.
Article5. Katano T, Sanada Y, Hirata Y, Yamada N, Okada N, Onishi Y, et al. 2019; Endovascular stent placement for venous complications following pediatric liver transplantation: outcomes and indications. Pediatr Surg Int. 35:1185–1195. DOI: 10.1007/s00383-019-04551-9. PMID: 31535198.
Article6. Zhang ZY, Jin L, Chen G, Su TH, Zhu ZJ, Sun LY, et al. 2017; Balloon dilatation for treatment of hepatic venous outflow obstruction following pediatric liver transplantation. World J Gastroenterol. 23:8227–8234. DOI: 10.3748/wjg.v23.i46.8227. PMID: 29290659. PMCID: PMC5739929.
Article7. Lu KT, Cheng YF, Chen TY, Tsang LC, Ou HY, Yu CY, et al. 2018; Efficiency of transluminal angioplasty of hepatic venous outflow obstruction in pediatric liver transplantation. Transplant Proc. 50:2715–2717. DOI: 10.1016/j.transproceed.2018.04.022. PMID: 30401383.
Article8. Yeh YT, Chen CY, Tseng HS, Wang HK, Tsai HL, Lin NC, et al. 2017; Enlarging vascular stents after pediatric liver transplantation. J Pediatr Surg. 52:1934–1939. DOI: 10.1016/j.jpedsurg.2017.08.060. PMID: 28927979.
Article9. Veerankutty FH, Ali TU, Manoj KS, Venugopal B. 2016; Reconstruction of a rare variant of the left hepatic vein in a left lateral segment liver graft from a living donor: technical notes. J Indian Assoc Pediatr Surg. 21:41–43. DOI: 10.4103/0971-9261.171938. PMID: 26862296. PMCID: PMC4721129.
Article10. Imamura H, Makuuchi M, Sakamoto Y, Sugawara Y, Sano K, Nakayama A, et al. 2000; Anatomical keys and pitfalls in living donor liver transplantation. J Hepatobiliary Pancreat Surg. 7:380–394. DOI: 10.1007/s005340070033. PMID: 11180859.
Article11. Matsunami H, Makuuchi M, Kawasaki S, Hashikura Y, Ikegami T, Nakazawa Y, et al. 1995; Venous reconstruction using three recipient hepatic veins in living related liver transplantation. Transplantation. 59:917–919. DOI: 10.1097/00007890-199503270-00024. PMID: 7701594.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Graft outflow vein venoplasty for a laparoscopically harvested left lateral section graft in pediatric living donor liver transplantation
- Outflow vein venoplasty of left lateral section graft for living donor liver transplantation in infant recipients
- Unification venoplasty of the outflow hepatic vein for laparoscopically harvested left liver grafts in pediatric living donor liver transplantation
- Incidence of superficial left hepatic vein and its usability for graft hepatic vein venoplasty in pediatric liver transplantation
- Standardized surgical techniques for adult living donor liver transplantation using a modified right lobe graft: a video presentation from bench to reperfusion