Korean J healthc assoc Infect Control Prev.
2020 Dec;25(2):79-85. 10.14192/kjicp.2020.25.2.79.
Basic Bacteriology for Infection Control
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2510133
- DOI: http://doi.org/10.14192/kjicp.2020.25.2.79
Abstract
- As bacteria are pathogens that often cause healthcare-associated infections, it is important to understand their characteristics, in order to carry out proper infection control activities. Differences in virulence and site of colonization cause differences in the distribution of major causative pathogens, and thus in the types of infection. Antimicrobial-resistant bacteria are particularly important in healthcare-associated infections because they erode the efficacy of antibiotics and lead to treatment failure. To prevent the spread of antimicrobial-resistant bacteria within healthcare facilities, infection control activities, including encouraging hand hygiene and application of contact precaution for infected patients are necessary.
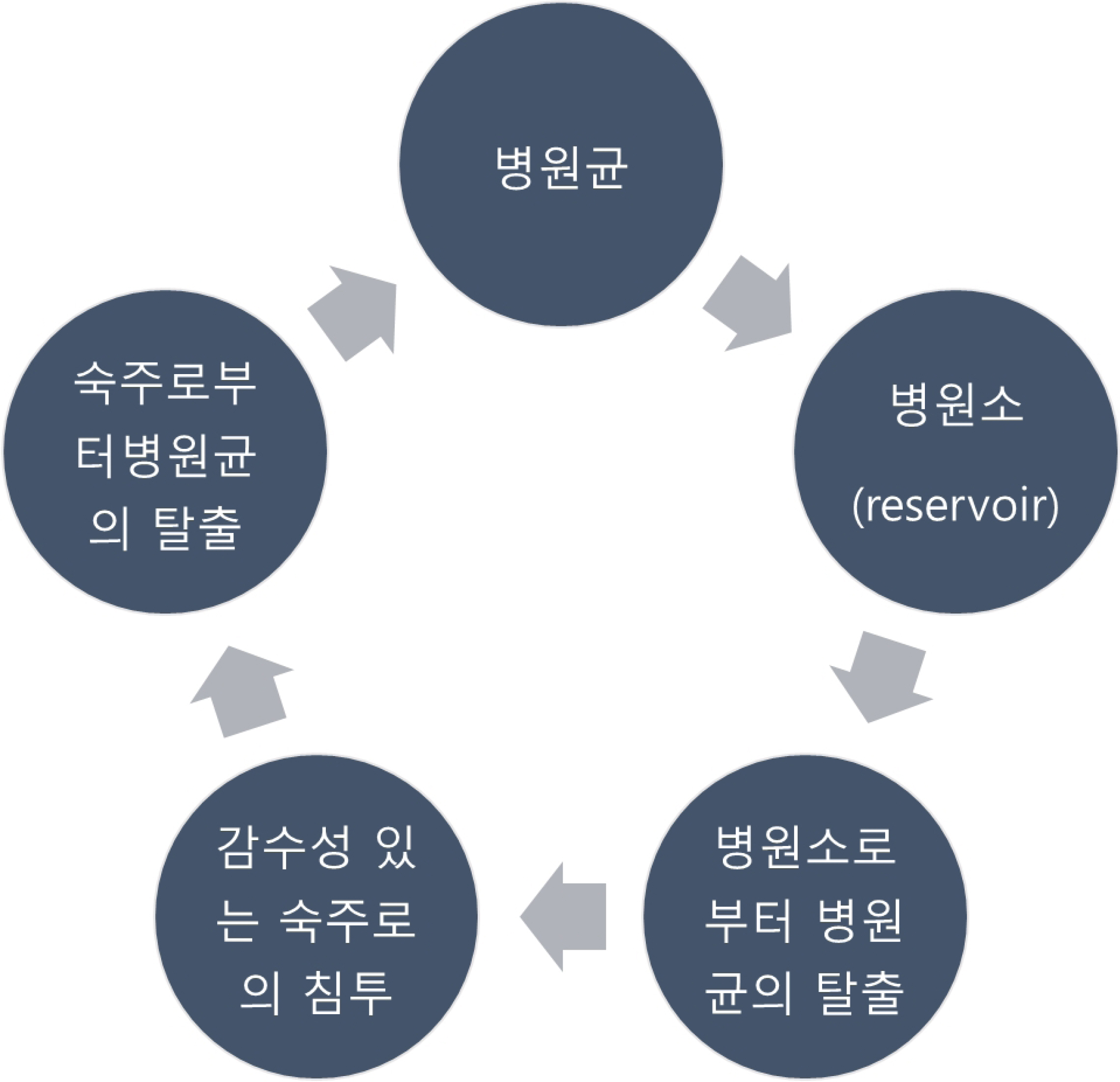
Figure
Reference
-
1. Yoo JH. 2018; Principle and perspective of healthcare-associated infection control. J Korean Med Assoc. 61:5–12. DOI: 10.5124/jkma.2018.61.1.5.
Article2. Korea Centers for Disease Control and Prevention (KCDC). 2017. Guidelines for prevention and control of Healthcare associated infections. KCDC;Cheongju: p. 1–292.3. Centers for Disease Control and Prevention. Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics. Principles of epidemiology in public health practice: an introduction to applied epidemiology and biostatistics. https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section10.html . Updated on May 18 2012.4. Kang CI. 2015; Antimicrobial therapy for infections caused by multidrug-resistant Gram-negative bacteria. Korean J Med. 88:502–8. DOI: 10.3904/kjm.2015.88.5.502.
Article5. Kim EJ, Kwak YG, Kim TH, Lee MS, Lee SO, Kim SR, et al. 2019; Korean National Healthcare-associated Infections Surveillance System, intensive care unit module report: summary of data from July 2017 through June 2018. Korean J Healthc Assoc Infect Control Prev. 24:69–80. DOI: 10.14192/kjicp.2019.24.2.69.
Article6. Kwak YG, Choi JY, Yoo H, Lee SO, Kim HB, Han SH, et al. 2016; Korean National Healthcare-associated Infections Surveillance System, intensive care unit module report: summary of data from July 2014 through June 2015. Korean J Healthc Assoc Infect Control Prev. 21:37–49. DOI: 10.14192/kjhaicp.2016.21.2.37.
Article7. Snydman DR, Jacobus NV, McDermott LA, Golan Y, Goldstein EJ, Harrell L, et al. 2011; Update on resistance of Bacteroides fragilis group and related species with special attention to carbapenems 2006-2009. Anaerobe. 17:147–51. DOI: 10.1016/j.anaerobe.2011.05.014. PMID: 21664469.
Article8. Edwards R, Hawkyard CV, Garvey MT, Greenwood D. 1999; Prevalence and degree of expression of the carbapenemase gene (cfiA) among clinical isolates of Bacteroides fragilis in Nottingham, UK. J Antimicrob Chemother. 43:273–6. DOI: 10.1093/jac/43.2.273. PMID: 11252334.
Article9. Beveridge TJ. 1999; Structures of gram-negative cell walls and their derived membrane vesicles. J Bacteriol. 181:4725–33. DOI: 10.1128/JB.181.16.4725-4733.1999. PMID: 10438737. PMCID: PMC93954.
Article10. Ryu M, Kwon N, Kim YB, Park J, Lee S. 2013; Prophylactic antibiotics therapy after splenectomy. Clin Pediatr Hematol Oncol. 20:95–101.11. Korea Centers for Disease Control and Prevention (KCDC). 2014. Guideline for disinfection and sterilization in healthcare facilities. KCDC;Cheongju: p. 1–64.12. Yigit H, Queenan AM, Anderson GJ, Domenech-Sanchez A, Biddle JW, Steward CD, et al. 2001; Novel carbapenem-hydrolyzing beta-lactamase, KPC-1, from a carbapenem-resistant strain of Klebsiella pneumoniae. Antimicrob Agents Chemother. 45:1151–61. DOI: 10.1128/AAC.45.4.1151-1161.2001. PMID: 11257029. PMCID: PMC90438.13. Wilson DN. 2014; Ribosome-targeting antibiotics and mechanisms of bacterial resistance. Nat Rev Microbiol. 12:35–48. DOI: 10.1038/nrmicro3155. PMID: 24336183.
Article14. Boyle KK, Wood S, Tarity TD. 2018; Low-virulence organisms and periprosthetic joint infection-biofilm considerations of these organisms. Curr Rev Musculoskelet Med. 11:409–19. DOI: 10.1007/s12178-018-9503-2. PMID: 29961193. PMCID: PMC6105490.
Article15. Buetti N, Lo Priore E, Atkinson A, Widmer AF, Kronenberg A, Marschall J. 2018; Catheter-related infections: does the spectrum of microbial causes change over time? A nationwide surveillance study. BMJ Open. 8:e023824. DOI: 10.1136/bmjopen-2018-023824. PMID: 30580270. PMCID: PMC6307612.
Article16. Sibbald RG, Woo K, Ayello EA. 2006; Increased bacterial burden and infection: the story of NERDS and STONES. Adv Skin Wound Care. 19:447–61. quiz 461-3. DOI: 10.1097/00129334-200610000-00012. PMID: 17008815.17. Livermore DM. 2012; Current epidemiology and growing resistance of gram-negative pathogens. Korean J Intern Med. 27:128–42. DOI: 10.3904/kjim.2012.27.2.128. PMID: 22707882. PMCID: PMC3372794.
Article18. Spellberg B, Guidos R, Gilbert D, Bradley J, Boucher HW, Scheld WM, et al. 2008; The epidemic of antibiotic-resistant infections: a call to action for the medical community from the Infectious Diseases Society of America. Clin Infect Dis. 46:155–64. DOI: 10.1086/524891. PMID: 18171244.
Article19. Kim B, Kim Y, Hwang H, Kim J, Kim SW, Bae IG, et al. 2018; Trends and correlation between antibiotic usage and resistance pattern among hospitalized patients at university hospitals in Korea, 2004 to 2012: a nationwide multicenter study. Medicine (Baltimore). 97:e13719. DOI: 10.1097/MD.0000000000013719. PMID: 30572507. PMCID: PMC6320075.20. Kim B, Lee MJ, Moon SM, Park SY, Song KH, Lee H, et al. 2020; Current status of antimicrobial stewardship programmes in Korean hospitals: results of a 2018 nationwide survey. J Hosp Infect. 104:172–80. DOI: 10.1016/j.jhin.2019.09.003. PMID: 31513880.
Article21. Sanseverino I, Navarro Cuenca A, Loos R, Marinov D, Lettieri T. 2018. State of the art on the contribution of water to antimicrobial resistance. Luxembourg;European Union: p. 1–89.22. Siegel JD, Rhinehart E, Jackson M, Chiarello L. 2007; Management of multidrug-resistant organisms in health care settings, 2006. Am J Infect Control. 35(10 Suppl 2):S165–93. DOI: 10.1016/j.ajic.2007.10.006. PMID: 18068814.
Article23. Park SH. 2018; Management of multi-drug resistant organisms in healthcare settings. J Korean Med Assoc. 61:26–35. DOI: 10.5124/jkma.2018.61.1.26.
Article24. Canny GO, McCormick BA. 2008; Bacteria in the intestine, helpful residents or enemies from within? Infect Immun. 76:3360–73. DOI: 10.1128/IAI.00187-08. PMID: 18474643. PMCID: PMC2493210.
Article25. Kim BN. 2007; Blood cultures: principles and practices. Infect Chemother. 39:111–6.26. Patel A, Parikh P, Dunn AN, Otter JA, Thota P, Fraser TG, et al. 2019; Effectiveness of daily chlorhexidine bathing for reducing gram-negative infections: a meta-analysis. Infect Control Hosp Epidemiol. 40:392–9. DOI: 10.1017/ice.2019.20. PMID: 30803462.
Article27. Huang SS, Singh R, McKinnell JA, Park S, Gombosev A, Eells SJ, et al. 2019; Decolonization to reduce postdischarge infection risk among MRSA carriers. N Engl J Med. 380:638–50. DOI: 10.1056/NEJMoa1716771. PMID: 30763195. PMCID: PMC6475519.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Essential Basic Bacteriology in Managing Musculoarticuloskeletal Infection: Bacterial Anatomy, Their Behavior, Host Phagocytic Activity, Immune System, Nutrition, And Antibiotics
- A Study on the Knowledge and Performance Status for Healthcare- Associated Infection Control and Prevention in Caregivers
- Infection Control in USA and the Study on the Efficacy of Nosocomial Infection Control
- Nurses' Perception of Accreditation, Awareness and Performance of Infection Control in an Accredited Healthcare System
- A Canadian Experience of Infection Control