Ann Surg Treat Res.
2020 Dec;99(6):337-343. 10.4174/astr.2020.99.6.337.
Neutrophil-to-lymphocyte ratio predicts early acute cellular rejection in living donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Surgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2508933
- DOI: http://doi.org/10.4174/astr.2020.99.6.337
Abstract
- Purpose
The aim of this study was to evaluate the predictive value of neutrophil-to-lymphocyte ratio (NLR) in acute cellular rejection (ACR) after living donor liver transplantation (LDLT).
Methods
All consecutive patients who underwent ABO-compatible (ABOc) LDLT from September 2014 to December 2017 were retrospectively reviewed. NLR was calculated on 3 occasions; (1) 4 weeks prior to liver transplantation (LT), (2) the day of LT, and (3) the day before liver biopsy.
Results
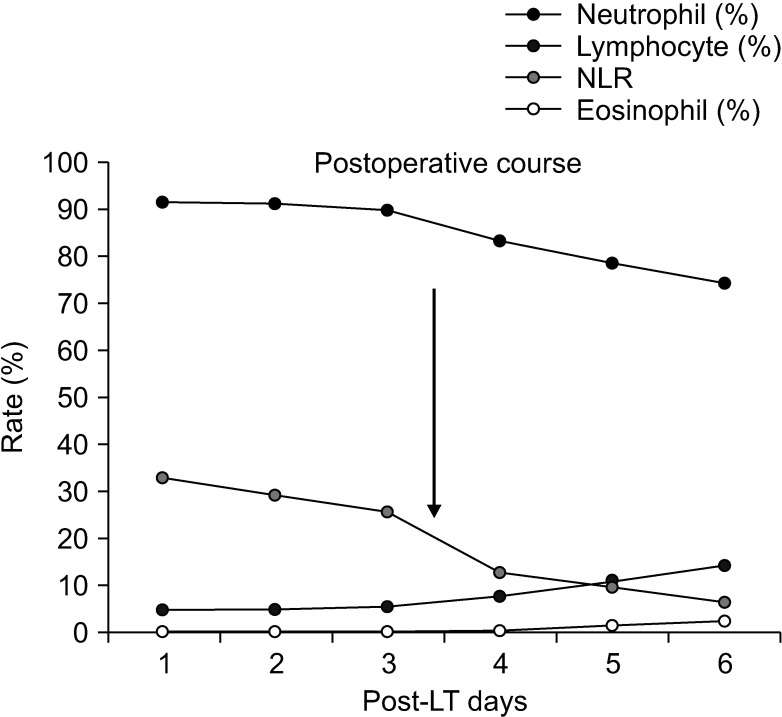
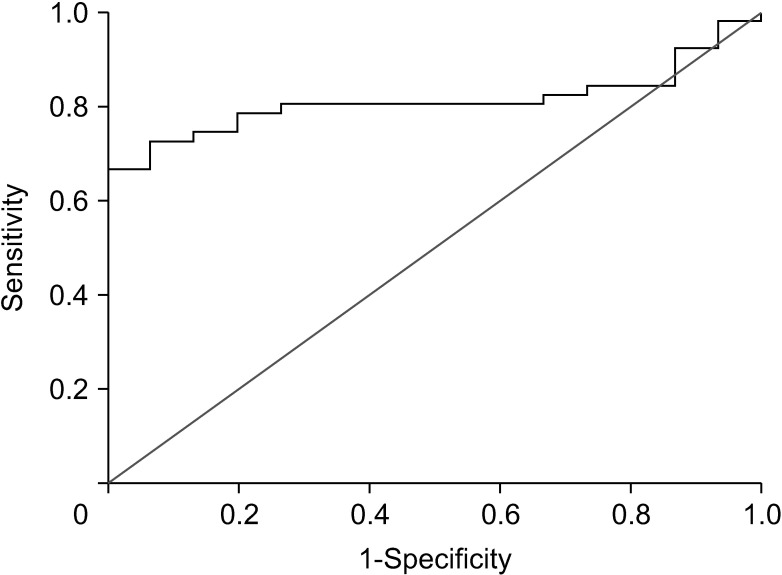
Among 66 patients who underwent ABOc LDLT, ACR was identified in 15 patients (22.7%) on protocol liver biopsy performed routinely on the postoperative day 7. There was no significant difference in NLR at 4 weeks prior to LT and the day of LT between no-ACR and ACR group (2.98 ± 1.92 vs. 2.54 ± 1.15, P = 0.433; 17.9 ± 8.31 vs. 20.5 ± 13.4, P = 0.393). However, NLR was significantly lower in ACR group compared to non-ACR group just prior to liver biopsy (5.82 ± 3.42 vs. 18.4 ± 17.2, P = 0.035). NLR tends to decrease 3.5 days before the onset of ACR. The area under the receiver operating characteristic curve for optimal cut-off value of NLR was 6.49, with sensitivity and specificity of 80.4% and 73.3% respectively.
Conclusion
NLR has a potential as a noninvasive predictor of early ACR in ABOc LDLT.
Keyword
Figure
Reference
-
1. Maluf DG, Stravitz RT, Cotterell AH, Posner MP, Nakatsuka M, Sterling RK, et al. Adult living donor versus deceased donor liver transplantation: a 6-year single center experience. Am J Transplant. 2005; 5:149–156. PMID: 15636624.2. Gruttadauria S, Vasta F, Mandalà L, Cintorino D, Piazza T, Spada M, et al. Basiliximab in a triple-drug regimen with tacrolimus and steroids in liver transplantation. Transplant Proc. 2005; 37:2611–2613. PMID: 16182762.3. Emond JC, Rouch D, Thistlethwaite J, Whitington P, Baker A, Ferrari M, et al. Rejection in liver allograft recipients: clinical characterization and management. Clin transplant. 1987; 1:143–150.4. Soin AS, Rasmussen A, Jamieson NV, Watson CJ, Friend PJ, Wight DG, et al. CsA levels in the early posttransplant period: predictive of chronic rejection in liver transplantation? Transplantation. 1995; 59:1119–1123. PMID: 7732557.5. Neil DA, Hubscher SG. Delay in diagnosis: a factor in the poor outcome of late acute rejection of liver allografts. Transplant Proc. 2001; 33:1525–1526. PMID: 11267407.6. Thurairajah PH, Carbone M, Bridgestock H, Thomas P, Hebbar S, Gunson BK, et al. Late acute liver allograft rejection; a study of its natural history and graft survival in the current era. Transplantation. 2013; 95:955–959. PMID: 23442806.7. Hultcrantz R, Gabrielsson N. Patients with persistent elevation of aminotransferases: investigation with ultrasonography, radionuclide imaging and liver biopsy. J Intern Med. 1993; 233:7–12. PMID: 8429291.8. Colonna JO 2nd, Brems JJ, Goldstein LI, Millis JM, Vargas JH, Berquist WE, et al. The importance of percutaneous liver biopsy in the management of the liver transplant recipient. Transplant Proc. 1988; 20 1 Suppl 1:682–684. PMID: 3279660.9. Kis B, Pamarthi V, Fan CM, Rabkin D, Baum RA. Safety and utility of transjugular liver biopsy in hematopoietic stem cell transplant recipients. J Vasc Interv Radiol. 2013; 24:85–89. PMID: 23200125.10. Lebrec D, Goldfarb G, Degott C, Rueff B, Benhamou JP. Transvenous liver biopsy: an experience based on 1000 hepatic tissue samplings with this procedure. Gastroenterology. 1982; 83:338–340. PMID: 7084612.11. Van Ha TG. Liver biopsy in liver transplant recipients. Semin Intervent Radiol. 2004; 21:271–274. PMID: 21331138.12. Sanada Y, Matsumoto K, Urahashi T, Ihara Y, Wakiya T, Okada N, et al. Protocol liver biopsy is the only examination that can detect mid-term graft fibrosis after pediatric liver transplantation. World J Gastroenterol. 2014; 20:6638–6650. PMID: 24914389.13. Bathgate AJ, Lee P, Hayes PC, Simpson KJ. Pretransplantation tumor necrosis factor-alpha production predicts acute rejection after liver transplantation. Liver Transpl. 2000; 6:721–727. PMID: 11084058.14. Boleslawski E, Conti F, Sanquer S, Podevin P, Chouzenoux S, Batteux F, et al. Defective inhibition of peripheral CD8+ T cell IL-2 production by anti-calcineurin drugs during acute liver allograft rejection. Transplantation. 2004; 77:1815–1820. PMID: 15223897.15. Foster PF, Sankary HN, Hart M, Ashmann M, Williams JW. Blood and graft eosinophilia as predictors of rejection in human liver transplantation. Transplantation. 1989; 47:72–74. PMID: 2643234.16. Nagral A, Ben-Ari Z, Dhillon AP, Burroughs AK. Eosinophils in acute cellular rejection in liver allografts. Liver Transpl Surg. 1998; 4:355–362. PMID: 9724472.17. De Groen PC, Kephart GM, Gleich GJ, Ludwig J. The eosinophil as an effector cell of the immune response during hepatic allograft rejection. Hepatology. 1994; 20:654–662. PMID: 7521317.18. Verhelst XP, Troisi RI, Colle I, Geerts A, van Vlierberghe H. Biomarkers for the diagnosis of acute cellular rejection in liver transplant recipients: a review. Hepatol Res. 2013; 43:165–178. PMID: 23186289.19. Kim H, Jung HI, Kwon SH, Bae SH, Kim HC, Baek MJ, et al. Preoperative neutrophil-lymphocyte ratio and CEA is associated with poor prognosis in patients with synchronous colorectal cancer liver metastasis. Ann Surg Treat Res. 2019; 96:191–200. PMID: 30941323.20. Ingulli E. Mechanism of cellular rejection in transplantation. Pediatr Nephrol. 2010; 25:61–74. PMID: 21476231.21. Taner T. Liver transplantation: rejection and tolerance. Liver Transpl. 2017; 23(S1):S85–S88. PMID: 28779559.22. Wang D, Matsumoto R, You Y, Che T, Lin XY, Gaffen SL, et al. CD3/CD28 cost imulat ion-induced NF-kappaB activation is mediated by recruitment of protein kinase C-theta, Bcl10, and IkappaB kinase beta to the immunological synapse through CARMA1. Mol Cell Biol. 2004; 24:164–171. PMID: 14673152.23. Kumar S, Mohapatra N, Borle DP, Choudhury A, Sarin S, Gupta E. Non invasive diagnosis of acute cellular rejection after liver transplantation: current opinion. Transpl Immunol. 2018; 47:1–9. PMID: 29452168.24. Henley KS, Lucey MR, Appelman HD, Baliga P, Brown KA, Burtch GD, et al. Biochemical and histopathological correlation in liver transplant: the first 180 days. Hepatology. 1992; 16:688–693. PMID: 1505912.25. Shalev O, Rubinger D, Barlatzky Y, Kopolovic J, Drukker A. Eosinophilia associated with acute allograft kidney rejection. Nephron. 1982; 31:182–183. PMID: 6750422.26. Hughes VF, Trull AK, Joshi O, Alexander GJ. Monitoring eosinophil activation and liver function after liver transplantation. Transplantation. 1998; 65:1334–1339. PMID: 9625015.27. Wang YC, Wu TJ, Wu TH, Lee CF, Chou HS, Chan KM, et al. The risk factors to predict acute rejection in liver transplantation. Transplant Proc. 2012; 44:526–528. PMID: 22410062.28. Wiesner RH, Demetris AJ, Belle SH, Seaberg EC, Lake JR, Zetterman RK, et al. Acute hepatic allograft rejection: incidence, risk factors, and impact on outcome. Hepatology. 1998; 28:638–645. PMID: 9731552.29. Clatworthy MR. Targeting B cells and antibody in transplantation. Am J Transplant. 2011; 11:1359–1367. PMID: 21668625.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liver retransplantation for adult recipients
- The Results of Spousal Donor Kidney Transplantation Via Exchange Donor Program and Direct Spousal Donor Kidney Transplantation in Living Donor Kidney Transplantation: Single Center Experience
- The Risk Factors of Acute Cellular Rejection in Adult Living Donor Liver Transplantation:Doubting the Value of Positive Lymphocytotoxic Cross-match Results
- Overcoming high pre-transplant isoagglutinin titers using high-dose intravenous immunoglobulin, salvage plasmapheresis, and booster rituximab without splenectomy in ABO-incompatible living donor liver transplantation: a case report
- The Impact of Acute Rejection on Long-Term Graft Outcome in Renal Allograft Recipient