J Korean Med Sci.
2020 Oct;35(40):e360. 10.3346/jkms.2020.35.e360.
Incidence and Mortality Rates of Thoracic Aortic Dissection in Korea – Inferred from the Nationwide Health Insurance Claims
- Affiliations
-
- 1Department of Thoracic and Cardiovascular Surgery, Hanyang University Seoul Hospital, Hanyang University College of Medicine, Seoul, Korea
- 2Department of Emergency Medicine, Hanyang University Seoul Hospital, Hanyang University College of Medicine, Seoul, Korea
- 3Department of Thoracic and Cardiovascular Surgery, Samsung Medical Center, School of Medicine, Sungkyunkwan University, Seoul, Korea
- 4Department of Thoracic and Cardiovascular Surgery, Hanyang University Guri Hospital, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2507619
- DOI: http://doi.org/10.3346/jkms.2020.35.e360
Abstract
- Background
Aortic dissection (AD) is one of the most catastrophic diseases and is associated with high morbidity and mortality. The aim of this study is to investigate the hospital incidence and mortality rates of thoracic AD in Korea using a nationwide database.
Methods
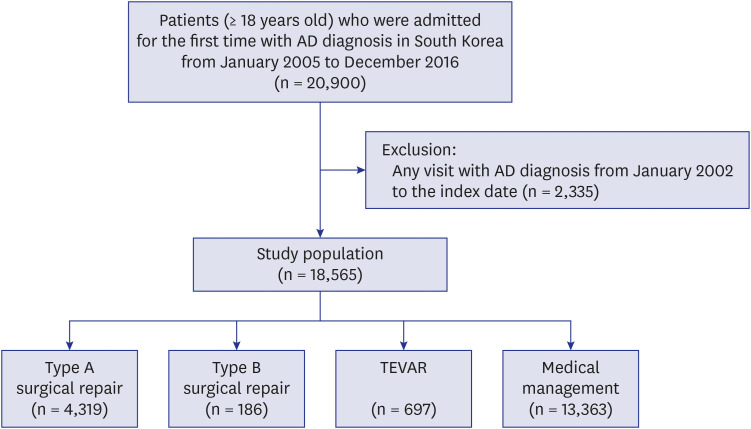
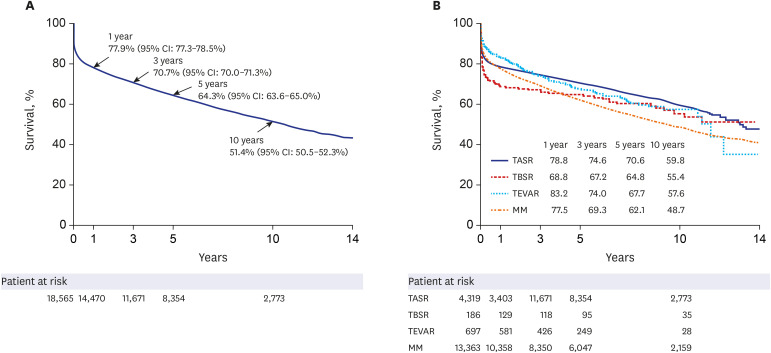
We conducted a nationwide population-based study using the health claims data of the National Health Insurance Service in Korea. From 2005 to 2016, adult patients newly diagnosed with AD were included. All patients were divided into the following four subgroups by treatment: type A surgical repair (TASR), type B surgical repair (TBSR), thoracic endovascular aortic repair (TEVAR), and medical management (MM). The incidence rate, mortality rate, and risk factors of in-hospital mortality were evaluated.
Results
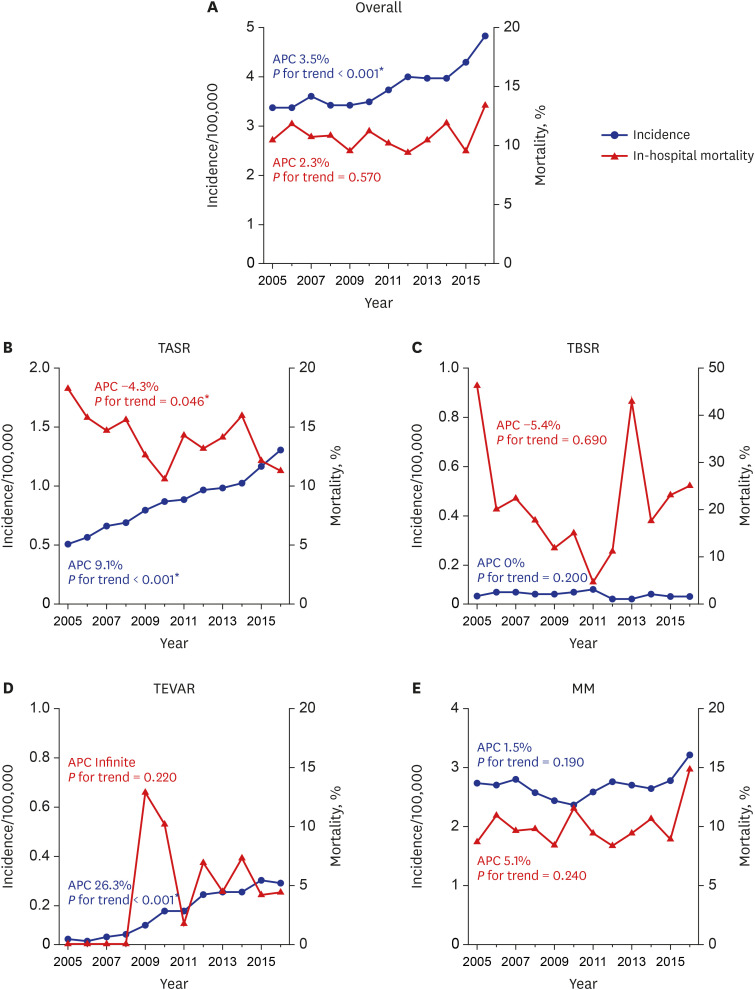
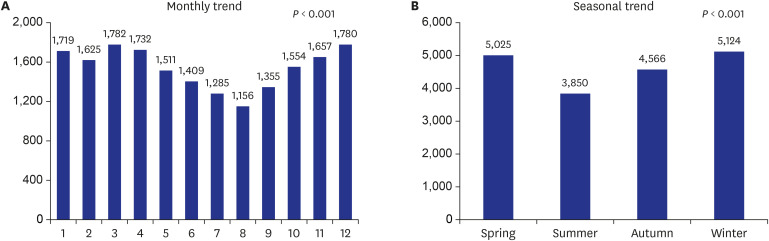
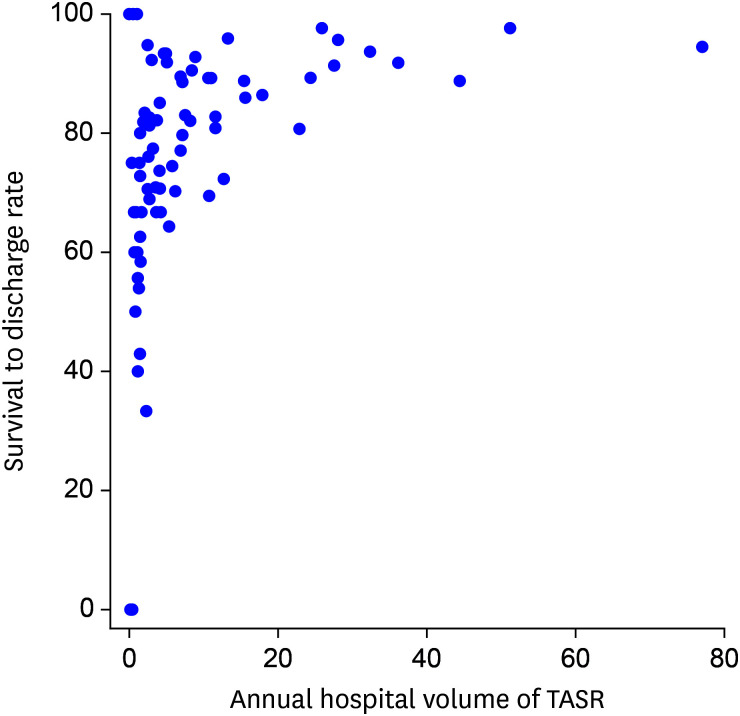
In total, 18,565 patients were newly diagnosed with AD (TASR, n = 4,319 [23.3%]; TBSR, n = 186 [1.0%]; TEVAR, n = 697 [3.8%]; MM, n = 13,363 [72.0%]). The overall AD incidence rate was 3.76 per 100,000 person-years and exhibited a gradual increase during the study period (3.29 to 4.82, P < 0.001). The overall in-hospital mortality rate was 10.84% and remained consistent (P = 0.57). However, the in-hospital mortality rate decreased in the TASR subgroup (18.23 to 11.27%, P = 0.046). An older age, the female sex, hypertension, and chronic kidney disease were independent risk factors for in-hospital mortality.
Conclusion
The incidence of thoracic AD has gradually increased in Korea. The in-hospital mortality in the TASR subgroup decreased over the decade, although the overall mortality of AD patients did not change.
Figure
Reference
-
1. McClure RS, Brogly SB, Lajkosz K, Payne D, Hall SF, Johnson AP. Epidemiology and management of thoracic aortic dissections and thoracic aortic aneurysms in Ontario, Canada: a population-based study. J Thorac Cardiovasc Surg. 2018; 155(6):2254–2264.e4. PMID: 29499864.
Article2. Zimmerman KP, Oderich G, Pochettino A, Hanson KT, Habermann EB, Bower TC, et al. Improving mortality trends for hospitalization of aortic dissection in the National Inpatient Sample. J Vasc Surg. 2016; 64(3):606–615.e1. PMID: 27183856.
Article3. Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, et al. The International Registry of Acute Aortic Dissection (IRAD): new insights into an old disease. JAMA. 2000; 283(7):897–903. PMID: 10685714.4. Melvinsdottir IH, Lund SH, Agnarsson BA, Sigvaldason K, Gudbjartsson T, Geirsson A. The incidence and mortality of acute thoracic aortic dissection: results from a whole nation study. Eur J Cardiothorac Surg. 2016; 50(6):1111–1117. PMID: 27334108.
Article5. Howard DP, Banerjee A, Fairhead JF, Perkins J, Silver LE, Rothwell PM, et al. Population-based study of incidence and outcome of acute aortic dissection and premorbid risk factor control: 10-year results from the Oxford Vascular Study. Circulation. 2013; 127(20):2031–2037. PMID: 23599348.
Article6. Mészáros I, Mórocz J, Szlávi J, Schmidt J, Tornóci L, Nagy L, et al. Epidemiology and clinicopathology of aortic dissection. Chest. 2000; 117(5):1271–1278. PMID: 10807810.
Article7. Mody PS, Wang Y, Geirsson A, Kim N, Desai MM, Gupta A, et al. Trends in aortic dissection hospitalizations, interventions, and outcomes among medicare beneficiaries in the United States, 2000–2011. Circ Cardiovasc Qual Outcomes. 2014; 7(6):920–928. PMID: 25336626.
Article8. Evangelista A, Isselbacher EM, Bossone E, Gleason TG, Eusanio MD, Sechtem U, et al. Insights from the international registry of acute aortic dissection: a 20-year experience of collaborative clinical research. Circulation. 2018; 137(17):1846–1860. PMID: 29685932.9. Pape LA, Awais M, Woznicki EM, Suzuki T, Trimarchi S, Evangelista A, et al. Presentation, diagnosis, and outcomes of acute aortic dissection. J Am Coll Cardiol. 2015; 66(4):350–358. PMID: 26205591.10. Tsai TT, Trimarchi S, Nienaber CA. Acute aortic dissection: perspectives from the International Registry of Acute Aortic Dissection (IRAD). Eur J Vasc Endovasc Surg. 2009; 37(2):149–159. PMID: 19097813.
Article11. Rampoldi V, Trimarchi S, Eagle KA, Nienaber CA, Oh JK, Bossone E, et al. Simple risk models to predict surgical mortality in acute type A aortic dissection: the International Registry of Acute Aortic Dissection score. Ann Thorac Surg. 2007; 83(1):55–61. PMID: 17184630.
Article12. Yeh TY, Chen CY, Huang JW, Chiu CC, Lai WT, Huang YB. Epidemiology and medication utilization pattern of aortic dissection in Taiwan: a population-based study. Medicine (Baltimore). 2015; 94(36):e1522. PMID: 26356726.13. Olsson C, Thelin S, Ståhle E, Ekbom A, Granath F. Thoracic aortic aneurysm and dissection: increasing prevalence and improved outcomes reported in a nationwide population-based study of more than 14,000 cases from 1987 to 2002. Circulation. 2006; 114(24):2611–2618. PMID: 17145990.
Article14. Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox regression. Am J Epidemiol. 2007; 165(6):710–718. PMID: 17182981.
Article15. Wundram M, Falk V, Eulert-Grehn JJ, Herbst H, Thurau J, Leidel BA, et al. Incidence of acute type A aortic dissection in emergency departments. Sci Rep. 2020; 10(1):7434. PMID: 32366917.
Article16. Abe T, Yamamoto H, Miyata H, Motomura N, Tokuda Y, Tanemoto K, et al. Patient trends and outcomes of surgery for type A acute aortic dissection in Japan: an analysis of more than 10 000 patients from the Japan Cardiovascular Surgery Database. Eur J Cardiothorac Surg. 2020; 57(4):660–667. PMID: 31793995.
Article17. Manzur M, Han SM, Dunn J, Elsayed RS, Fleischman F, Casagrande Y, et al. Management of patients with acute aortic syndrome through a regional rapid transport system. J Vasc Surg. 2017; 65(1):21–29. PMID: 27707620.
Article18. Lou X, Chen EP, Duwayri YM, Veeraswamy RK, Jordan WD Jr, Zehner CA, et al. The impact of thoracic endovascular aortic repair on long-term survival in type B aortic dissection. Ann Thorac Surg. 2018; 105(1):31–38. PMID: 28811003.19. Grigorian A, Spencer D, Donayre C, Nahmias J, Schubl S, Gabriel V, et al. National trends of thoracic endovascular aortic repair versus open repair in blunt thoracic aortic injury. Ann Vasc Surg. 2018; 52:72–78. PMID: 29886219.
Article20. Cho JR, Shin S, Kim JS, Ko YG, Hong MK, Jang Y, et al. Clinical characteristics of acute aortic syndrome in korean patients: from the korean multi-center registry of acute aortic syndrome. Korean Circ J. 2012; 42(8):528–537. PMID: 22977448.
Article21. Kim JB, Choo SJ, Kim WK, Kim HJ, Jung SH, Chung CH, et al. Outcomes of acute retrograde type A aortic dissection with an entry tear in descending aorta. Circulation. 2014; 130(11):Suppl 1. S39–44. PMID: 25200054.
Article22. Nienaber CA, Clough RE. Management of acute aortic dissection. Lancet. 2015; 385(9970):800–811. PMID: 25662791.
Article23. Yamaguchi T, Nakai M, Sumita Y, Miyamoto Y, Matsuda H, Inoue Y, et al. Current status of the management and outcomes of acute aortic dissection in Japan: Analyses of nationwide Japanese Registry of All Cardiac and Vascular Diseases-Diagnostic Procedure Combination data. Eur Heart J Acute Cardiovasc Care. Forthcoming 2019. DOI: 10.1177/2048872619872847.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sensitivity of Medical Insurance Claims Data Using Population-based Cancer Registry Data
- Fracture of the Bare Spring of a Thoracic Endograft for Type A Aortic Dissection: A Case Report
- Retrograde Aortic Dissection after Thoracic Endovascular Aortic Repair for Descending Aorta: 2 case reports
- A Case of Total Aortic Arch Replacement with Root Plasty with Right Coronary Artery Bypass and Distal Open Stent-graft Insertion in Acute Type I Aortic Dissection
- Incidence and Clinical Outcomes of Febrile Neutropenia in Adult Cancer Patients with Chemotherapy Using Korean Nationwide Health Insurance Database