Korean J Orthod.
2020 Sep;50(5):346-355. 10.4041/kjod.2020.50.5.346.
Maxillary protraction using customized mini-plates for anchorage in an adolescent girl with skeletal Class III malocclusion
- Affiliations
-
- 1Department of Orthodontics, School of Stomatology, Capital Medical University, Beijing, China
- KMID: 2506469
- DOI: http://doi.org/10.4041/kjod.2020.50.5.346
Abstract
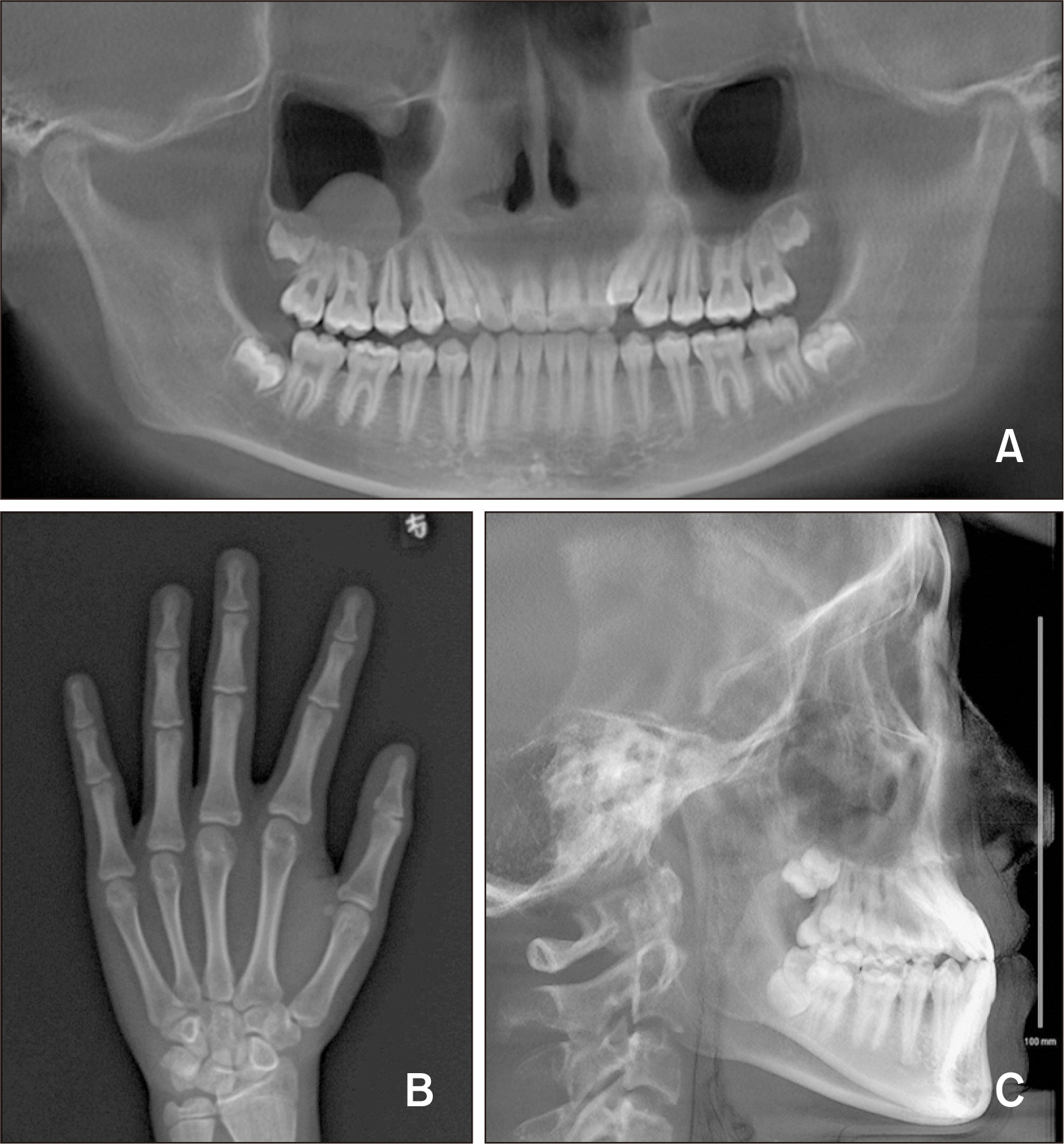
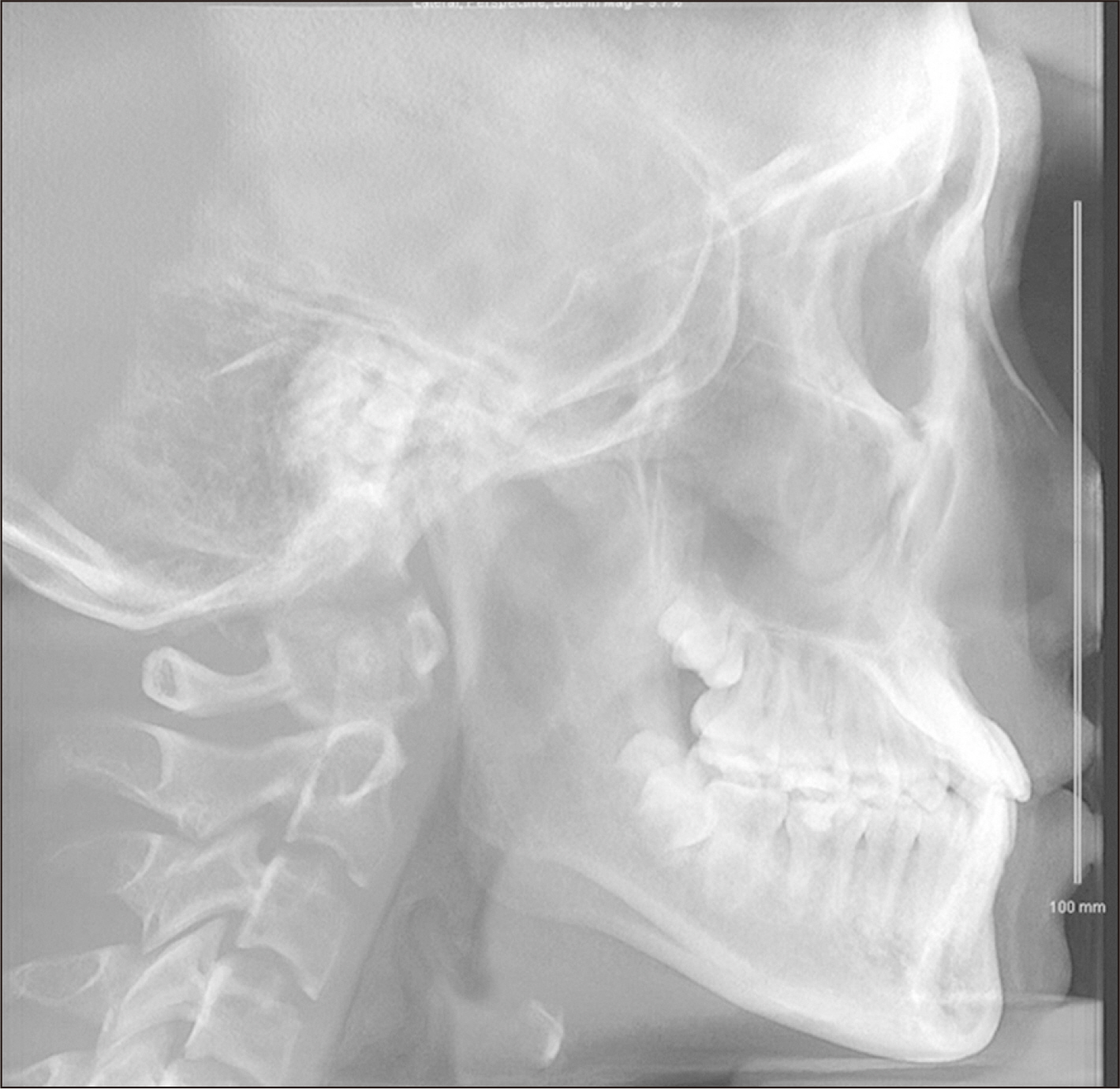
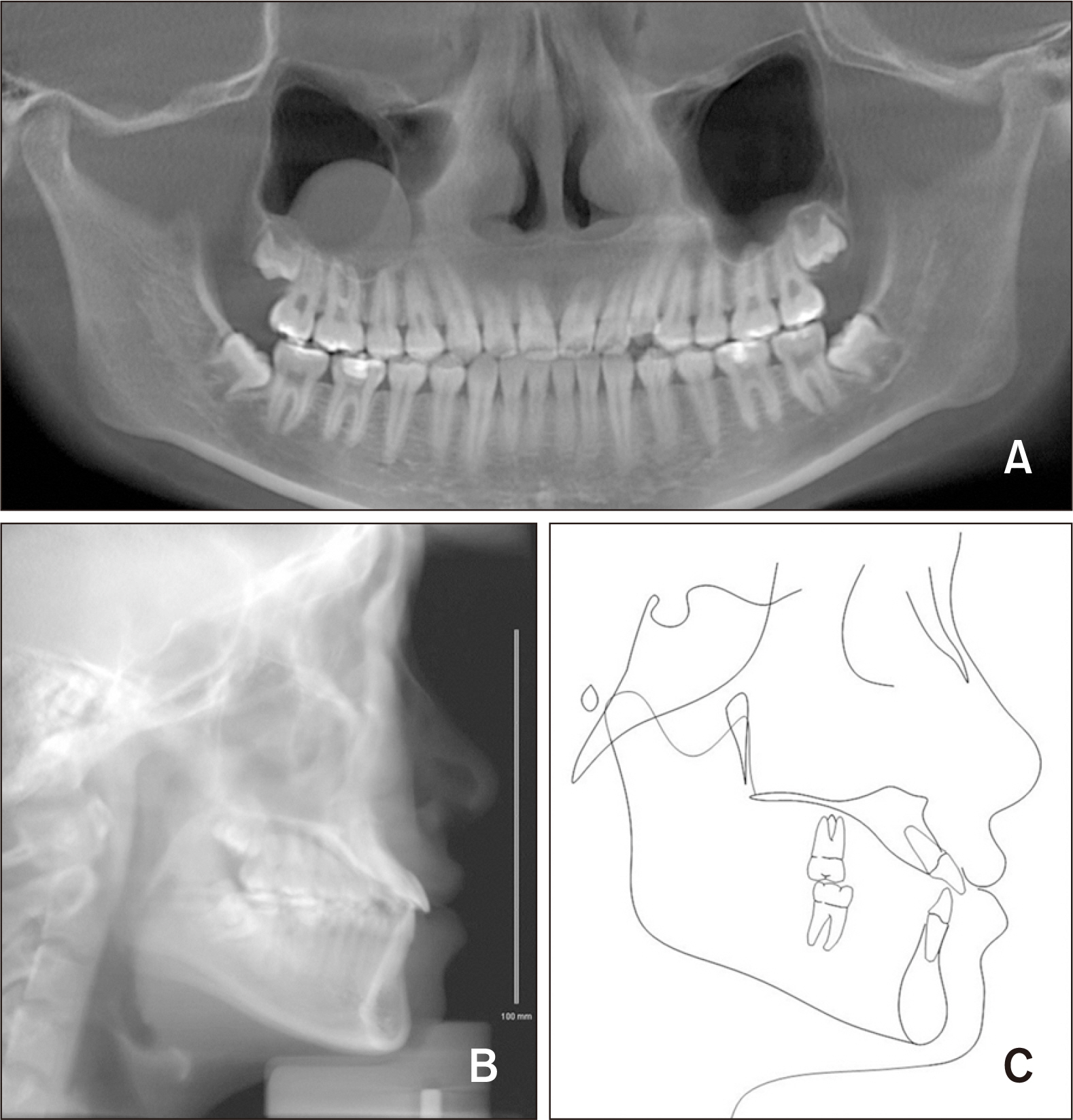
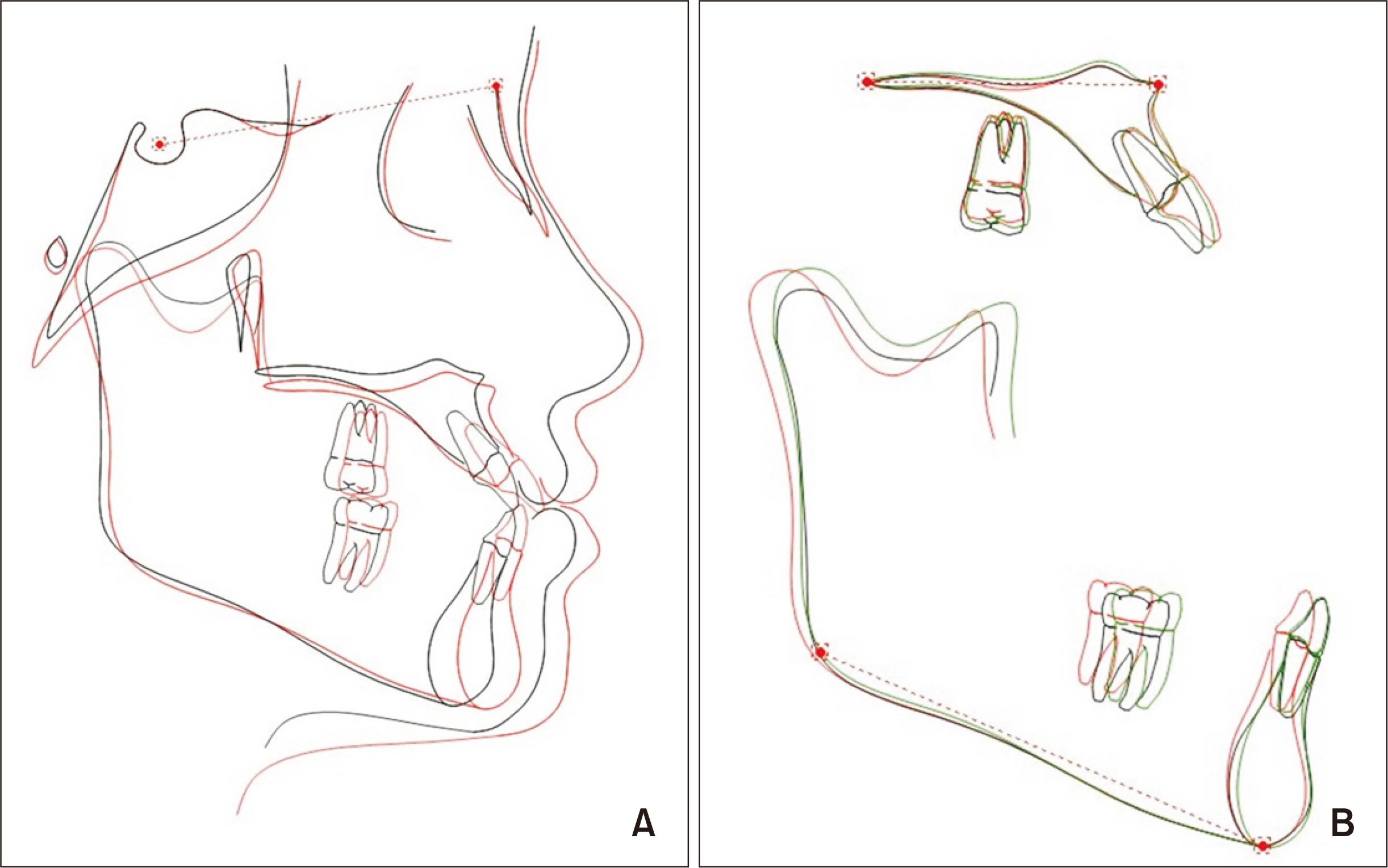
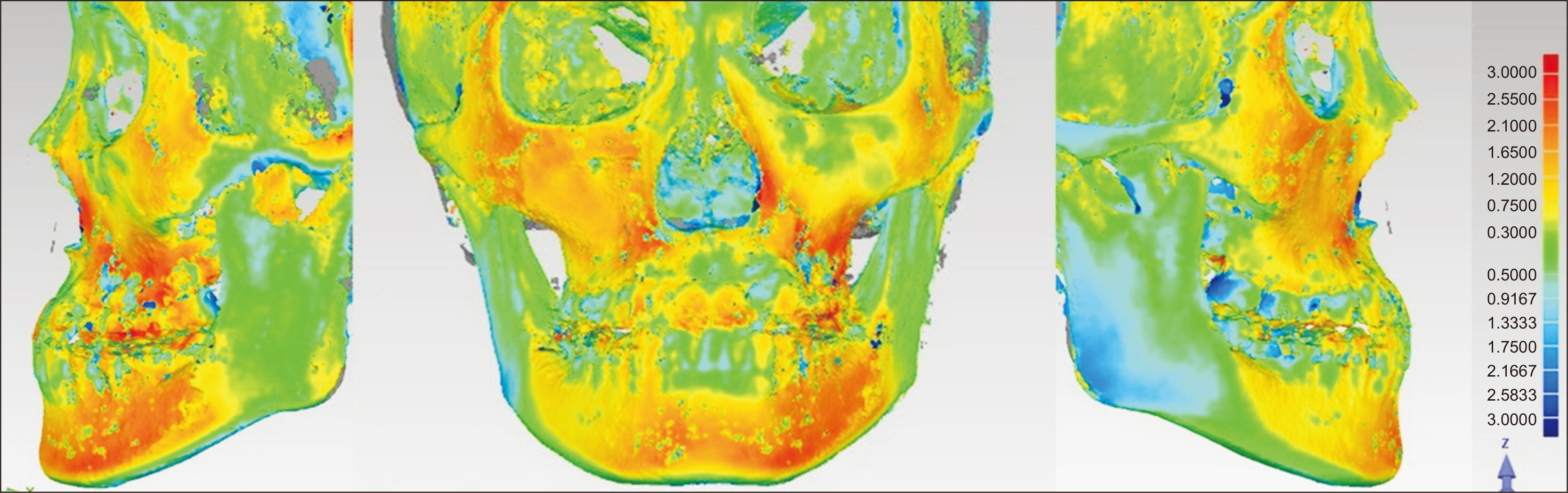
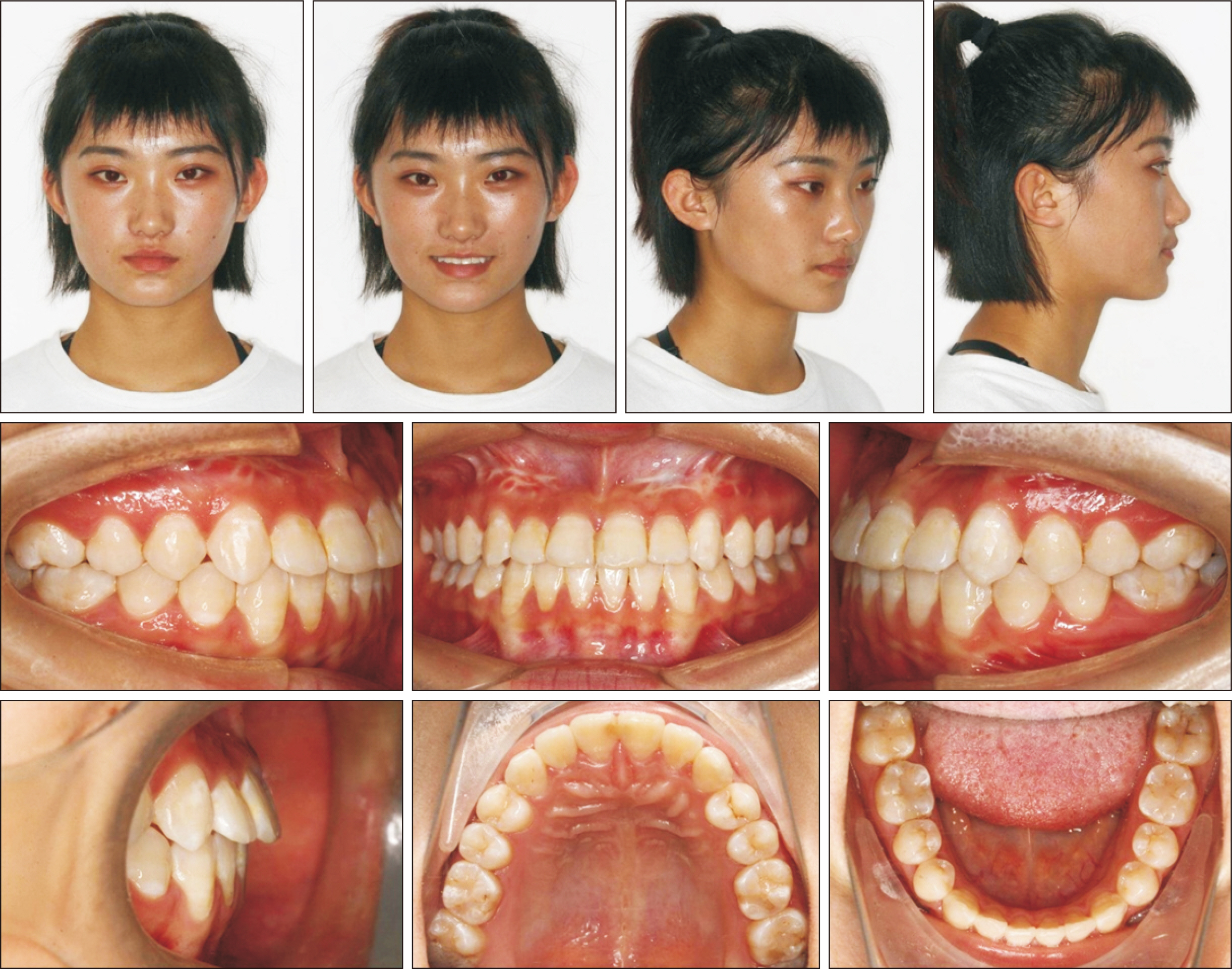
- The treatment of skeletal Class III malocclusion in adolescents is challenging. Maxillary protraction, particularly that using bone anchorage, has been proven to be an effective method for the stimulation of maxillary growth. However, the conventional procedure, which involves the surgical implantation of mini-plates, is traumatic and associated with a high risk. Three-dimensional (3D) digital technology offers the possibility of individualized treatment. Customized miniplates can be designed according to the shape of the maxillary surface and the positions of the roots on cone-beam computed tomography scans; this reduces both the surgical risk and patient trauma. Here we report a case involving a 12-year-old adolescent girl with skeletal Class III malocclusion and midface deficiency that was treated in two phases. In phase 1, rapid maxillary expansion and protraction were performed using 3D-printed mini-plates for anchorage. The mini-plates exhibited better adaptation to the bone contour, and titanium screw implantation was safer because of the customized design. The orthopedic force applied to each mini-plate was approximately 400–500 g, and the plates remained stable during the maxillary protraction process, which exhibited efficacious orthopedic effects and significantly improved the facial profile and esthetics. In phase 2, fixed appliances were used for alignment and leveling of the maxillary and mandibular dentitions. The complete two-phase treatment lasted for 24 months. After 48 months of retention, the treatment outcomes remained stable.
Figure
Cited by 1 articles
-
Three-dimensional finite element analysis on the effects of maxillary protraction with an individual titanium plate at multiple directions and locations
Fan Wang, Qiao Chang, Shuran Liang, Yuxing Bai
Korean J Orthod. 2024;54(2):108-116. doi: 10.4041/kjod23.217.
Reference
-
1. Allwright WC, Bundred WH. 1964; A survey of handicapping dentofacial anomalies among Chinese in Hong Kong. Int Dent J. 14:505–19.2. Guyer EC, Ellis EE 3rd, McNamara JA Jr, Behrents RG. 1986; Components of class III malocclusion in juveniles and adolescents. Angle Orthod. 56:7–30. DOI: 10.1043/0003-3219(1986)056<0007:COCIMI>2.0.CO;2. PMID: 3485393.3. Kim JH, Viana MA, Graber TM, Omerza FF, BeGole EA. 1999; The effectiveness of protraction face mask therapy: a meta-analysis. Am J Orthod Dentofacial Orthop. 115:675–85. DOI: 10.1016/S0889-5406(99)70294-5. PMID: 10358251.
Article4. De Clerck HJ, Cornelis MA, Cevidanes LH, Heymann GC, Tulloch CJ. 2009; Orthopedic traction of the maxilla with miniplates: a new perspective for treatment of midface deficiency. J Oral Maxillofac Surg. 67:2123–9. DOI: 10.1016/j.joms.2009.03.007. PMID: 19761906. PMCID: PMC2910397.
Article5. Kook YA, Bayome M, Park JH, Kim KB, Kim SH, Chung KR. 2015; New approach of maxillary protraction using modified C-palatal plates in Class III patients. Korean J Orthod. 45:209–14. DOI: 10.4041/kjod.2015.45.4.209. PMID: 26258067. PMCID: PMC4524960.
Article6. Cornelis MA, Scheffler NR, Mahy P, Siciliano S, De Clerck HJ, Tulloch JF. 2008; Modified miniplates for temporary skeletal anchorage in orthodontics: placement and removal surgeries. J Oral Maxillofac Surg. 66:1439–45. DOI: 10.1016/j.joms.2008.01.037. PMID: 18571028. PMCID: PMC2705617.
Article7. Sar C, Arman-Özçırpıcı A, Uçkan S, Yazıcı AC. 2011; Comparative evaluation of maxillary protraction with or without skeletal anchorage. Am J Orthod Dentofacial Orthop. 139:636–49. DOI: 10.1016/j.ajodo.2009.06.039. PMID: 21536207.8. Hino CT, Cevidanes LH, Nguyen TT, De Clerck HJ, Franchi L. 2013; Three-dimensional analysis of maxillary changes associated with facemask and rapid maxillary expansion compared with bone anchored maxillary protraction. Am J Orthod Dentofacial Orthop. 144:705–14. DOI: 10.1016/j.ajodo.2013.07.011. PMID: 24182587. PMCID: PMC3972125.
Article9. Suojanen J, Leikola J, Stoor P. 2016; The use of patient-specific implants in orthognathic surgery: a series of 32 maxillary osteotomy patients. J Craniomaxillofac Surg. 44:1913–6. DOI: 10.1016/j.jcms.2016.09.008. PMID: 27769722.
Article10. Brunso J, Franco M, Constantinescu T, Barbier L, Santamaría JA, Alvarez J. 2016; Custom-machined miniplates and bone-supported guides for orthognathic surgery: a new surgical procedure. J Oral Maxillofac Surg. 74:1061.e1–1061.e12. DOI: 10.1016/j.joms.2016.01.016. PMID: 26868183.
Article11. Saadia M, Torres E. 2000; Sagittal changes after maxillary protraction with expansion in class III patients in the primary, mixed, and late mixed dentitions: a longitudinal retrospective study. Am J Orthod Dentofacial Orthop. 117:669–80. DOI: 10.1016/S0889-5406(00)70176-4. PMID: 10842110.
Article12. Cha BK, Ngan PW. 2011; Skeletal anchorage for orthopedic correction of growing class III patients. Semin Orthod. 17:124–37. DOI: 10.1053/j.sodo.2010.12.005.
Article13. Lee NK, Yang IH, Baek SH. 2012; The short-term treatment effects of face mask therapy in Class III patients based on the anchorage device: miniplates vs rapid maxillary expansion. Angle Orthod. 82:846–52. DOI: 10.2319/090811-584.1. PMID: 22264134.14. Ağlarcı C, Esenlik E, Fındık Y. 2016; Comparison of short-term effects between face mask and skeletal anchorage therapy with intermaxillary elastics in patients with maxillary retrognathia. Eur J Orthod. 38:313–23. DOI: 10.1093/ejo/cjv053. PMID: 26219549. PMCID: PMC4914908.
Article15. Esenlik E, Ağlarcı C, Albayrak GE, Fındık Y. 2015; Maxillary protraction using skeletal anchorage and intermaxillary elastics in Skeletal Class III patients. Korean J Orthod. 45:95–101. DOI: 10.4041/kjod.2015.45.2.95. PMID: 25798416. PMCID: PMC4367137.
Article16. Delaire J. 1997; Maxillary development revisited: relevance to the orthopaedic treatment of Class III malocclusions. Eur J Orthod. 19:289–311. DOI: 10.1093/ejo/19.3.289. PMID: 9239959.
Article17. De Clerck H, Cevidanes L, Baccetti T. 2010; Dentofacial effects of bone-anchored maxillary protraction: a controlled study of consecutively treated Class III patients. Am J Orthod Dentofacial Orthop. 138:577–81. DOI: 10.1016/j.ajodo.2009.10.037. PMID: 21055597. PMCID: PMC3033914.
Article18. Kiliç N, Kiki A, Oktay H, Erdem A. 2008; Effects of rapid maxillary expansion on Holdaway soft tissue measurements. Eur J Orthod. 30:239–43. DOI: 10.1093/ejo/cjn004. PMID: 18540012.19. Gautam P, Valiathan A, Adhikari R. 2009; Skeletal response to maxillary protraction with and without maxillary expansion: a finite element study. Am J Orthod Dentofacial Orthop. 135:723–8. DOI: 10.1016/j.ajodo.2007.06.016. PMID: 19524831.
Article20. Bai YX. 2016; [Application of three-dimensional digital technology in the diagnosis and treatment planning in orthodontics]. Zhonghua Kou Qiang Yi Xue Za Zhi. 51:326–30. Chinese. DOI: 10.3760/cma.j.issn.1002-0098.2016.06.002. PMID: 27256524.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Maxillary protraction treatment of skeletal Class III children using miniplate anchorage
- Maxillary protraction using skeletal anchorage and intermaxillary elastics in Skeletal Class III patients
- Does surgically assisted maxillary protraction with skeletal anchorage and Class III elastics affect the pharyngeal airway? A retrospective, long-term study
- Treatment of skeletal Class III malocclustion with maxillary protraction appliance
- Surgical orthodontic treatment of skeletal Class III malocclusion using mini-implant: correction of horizontal and vertical dental compensation