Ann Surg Treat Res.
2020 Sep;99(3):153-160. 10.4174/astr.2020.99.3.153.
Clinical impact of sarcopenia in patients with colon cancer undergoing laparoscopic surgery
- Affiliations
-
- 1Department of Surgery, Chungnam National University College of Medicine, Daejeon, Korea
- 2Department of Radiology, Chungnam National University College of Medicine, Daejeon, Korea
- KMID: 2505487
- DOI: http://doi.org/10.4174/astr.2020.99.3.153
Abstract
- Purpose
Previous studies have reported that progressive muscle loss, known as sarcopenia, has a negative impact on colon cancer treatment. However, the majority of studies have analyzed on patients undergoing open resection, and the association of sarcopenia with clinical outcomes is not clear for patients with colon cancer undergoing laparoscopic surgery. Thus, the aim of this study was to evaluate the impact of sarcopenia on clinical outcomes after laparoscopic surgery for colon cancer.
Methods
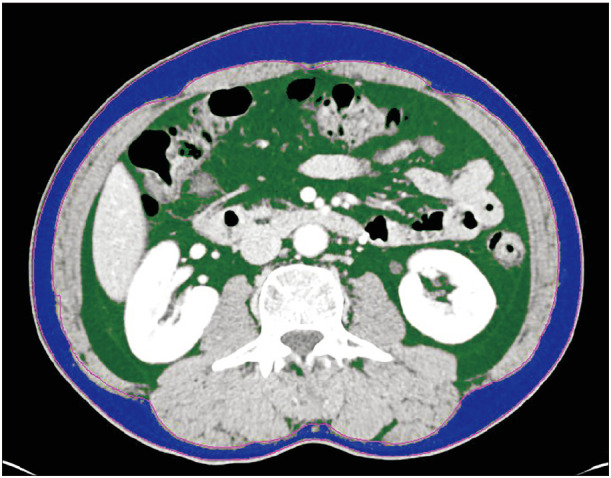
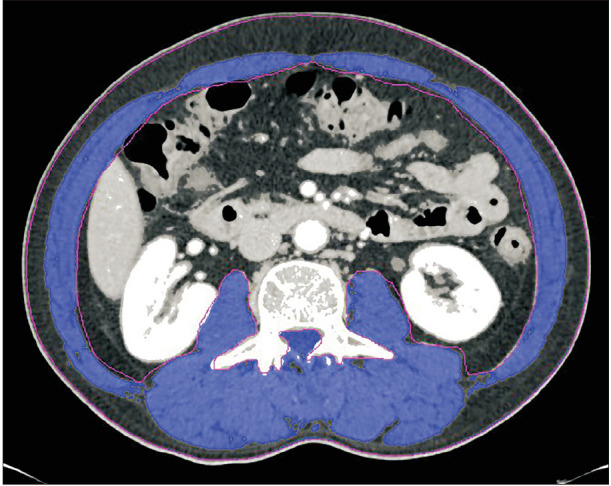
A total of 423 patients who underwent laparoscopic surgery for colon cancer between November 2010 and October 2014 were included. Body composition was assessed by measuring muscle and fat areas at the third lumbar vertebra (L3) on preoperative computed tomography. The L3 skeletal muscle area was used to calculate the skeletal muscle index and to assess for sarcopenia.
Results
Sarcopenia was identified in 54 patients (12.8%). The median time to first flatus (3 days), median time to tolerable soft diet (4 days), and median length of hospital stay (7 days) were not significantly different between patients with and without sarcopenia. However, sarcopenia was an independent risk factor for postoperative complications in the logistic regression multivariate analysis (p = 0.015). Sarcopenia was not associated with overall or disease-free survival.
Conclusion
Sarcopenia was not negatively associated with functional recovery, hospital stay, and oncologic outcomes in patients with colon cancer who underwent laparoscopic surgery. However, sarcopenia was associated with postoperative complications after laparoscopic surgery for colon cancer.
Keyword
Figure
Cited by 1 articles
-
Upper thigh skeletal muscle index predicts outcomes in liver transplant recipients
Manuel Lim, Jong Man Kim, Jaehun Yang, Jieun Kwon, Kyeong Deok Kim, Eun Sung Jeong, Jinsoo Rhu, Gyu-Seong Choi, Jae-Won Joh, Suk-Koo Lee
Ann Surg Treat Res. 2023;105(4):219-227. doi: 10.4174/astr.2023.105.4.219.
Reference
-
1. Milte R, Crotty M. Musculoskeletal health, frailty and functional decline. Best Pract Res Clin Rheumatol. 2014; 28:395–410. PMID: 25481423.2. Cooper C, Dere W, Evans W, Kanis JA, Rizzoli R, Sayer AA, et al. Frailty and sarcopenia: definitions and outcome parameters. Osteoporos Int. 2012; 23:1839–1848. PMID: 22290243.3. Prado CM, Lieffers JR, McCargar LJ, Reiman T, Sawyer MB, Martin L, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol. 2008; 9:629–635. PMID: 18539529.4. Levolger S, van Vugt JL, de Bruin RW, IJzermans JN. Systematic review of sarcopenia in patients operated on for gastrointestinal and hepatopancreatobiliary malignancies. Br J Surg. 2015; 102:1448–1458. PMID: 26375617.5. Lieffers JR, Bathe OF, Fassbender K, Winget M, Baracos VE. Sarcopenia is associated with postoperative infection and delayed recovery from colorectal cancer resection surgery. Br J Cancer. 2012; 107:931–936. PMID: 22871883.6. Huang DD, Wang SL, Zhuang CL, Zheng BS, Lu JX, Chen FF, et al. Sarcopenia, as defined by low muscle mass, strength and physical performance, predicts complications after surgery for colorectal cancer. Colorectal Dis. 2015; 17:O256–O264. PMID: 26194849.7. Jones KI, Doleman B, Scott S, Lund JN, Williams JP. Simple psoas cross-sectional area measurement is a quick and easy method to assess sarcopenia and predicts major surgical complications. Colorectal Dis. 2015; 17:O20–O26. PMID: 25328119.8. Malietzis G, Aziz O, Bagnall NM, Johns N, Fearon KC, Jenkins JT. The role of body composition evaluation by computerized tomography in determining colorectal cancer treatment outcomes: a systematic review. Eur J Surg Oncol. 2015; 41:186–196. PMID: 25468746.9. Peng PD, van Vledder MG, Tsai S, de Jong MC, Makary M, Ng J, et al. Sarcopenia negatively impacts short-term outcomes in patients undergoing hepatic resection for colorectal liver metastasis. . HPB (Oxford). 2011; 13:439–446. PMID: 21689226.10. Jayne DG, Guillou PJ, Thorpe H, Quirke P, Copeland J, Smith AM, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007; 25:3061–3068. PMID: 17634484.11. Colon Cancer Laparoscopic or Open Resection Study Group. Buunen M, Veldkamp R, Hop WC, Kuhry E, Jeekel J, et al. Survival after laparoscopic surgery versus open surgery for colon cancer: long-term outcome of a randomised clinical trial. Lancet Oncol. 2009; 10:44–52. PMID: 19071061.12. Clinical Outcomes of Surgical Therapy Study Group. Nelson H, Sargent DJ, Wieand HS, Fleshman J, Anvari M, et al. A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004; 350:2050–2059. PMID: 15141043.13. Pedziwiatr M, Pisarska M, Major P, Grochowska A, Matłok M, Przeczek K, et al. Laparoscopic colorectal cancer surgery combined with enhanced recovery after surgery protocol (ERAS) reduces the negative impact of sarcopenia on shortterm outcomes. Eur J Surg Oncol. 2016; 42:779–787. PMID: 27156809.14. Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R. Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol (1985). 1998; 85:115–122. PMID: 9655763.15. Martin L, Birdsell L, Macdonald N, Reiman T, Clandinin MT, McCargar LJ, et al. Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol. 2013; 31:1539–1547. PMID: 23530101.16. Jung HW, Kim JW, Kim JY, Kim SW, Yang HK, Lee JW, et al. Effect of muscle mass on toxicity and survival in patients with colon cancer undergoing adjuvant chemotherapy. Support Care Cancer. 2015; 23:687–694. PMID: 25163434.17. Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005; 6:477–484. PMID: 15992696.18. Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, et al. Laparoscopy-assisted colectomy versus open colectomy for treatment of nonmetastatic colon cancer: a randomised trial. Lancet. 2002; 359:2224–2229. PMID: 12103285.19. Janssen I, Heymsfield SB, Ross R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc. 2002; 50:889–896. PMID: 12028177.20. Evans WJ. Skeletal muscle loss: cachexia, sarcopenia, and inactivity. Am J Clin Nutr. 2010; 91:1123S–1127S. PMID: 20164314.21. Van Vledder MG, Levolger S, Ayez N, Verhoef C, Tran TC, Ijzermans JN. Body composition and outcome in patients undergoing resection of colorectal liver metastases. Br J Surg. 2012; 99:550–557. PMID: 22246799.22. Dodson S, Baracos VE, Jatoi A, Evans WJ, Cella D, Dalton JT, et al. Muscle wasting in cancer cachexia: clinical implications, diagnosis, and emerging treatment strategies. Annu Rev Med. 2011; 62:265–279. PMID: 20731602.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of single-port laparoscopic approach on scar assessment by patients and observers: a multicenter retrospective study
- Laparoscopic transverse colectomy using a new articulating instrument
- Is the oncological impact of vascular invasion more important in right colon cancer?
- Comparing the initiation of adjuvant chemotherapy after robotic and laparoscopic colon cancer surgeries: A case-controlled study with propensity score matching
- Laparoscopic Surgery for Colorectal Cancer