J Korean Med Sci.
2020 Aug;35(31):e268. 10.3346/jkms.2020.35.e268.
Performance of a Community-based Noncommunicable Disease Control Program in Korea: Patients 65 Years of Age or Older
- Affiliations
-
- 1Department of Preventive Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea
- 2Department of Information Statistics, Gyeongsang National University, Jinju, Korea
- 3Department of Preventive Medicine, College of Medicine and Institute of Health Science, Gyeongsang National University, Jinju, Korea
- 4Department of Nursing, Soonchunhyang University College of Medicine, Cheonan, Korea
- KMID: 2505198
- DOI: http://doi.org/10.3346/jkms.2020.35.e268
Abstract
- Background
In Korea, the Korean Community-based Noncommunicable Disease Prevention and Control Program (KCNPC) was implemented in 2012 for the management of patients with chronic diseases. Nineteen primary care clinics, public health centers, and education and consulting centers (ECCs) participated in the implementation of this program. This study assessed the effectiveness of this chronic disease control model by comparing mortality rate and the incidence of complications between patients participating in the KCNPC program and a control group.
Methods
Using data from the National Health Insurance Service and data from hypertension and diabetes patients registered with 19 ECCs between January 1, 2010 and December 31, 2012, hypertension and diabetes patients who had been treated at a clinic were selected. The final analysis included 252,900 patients, with the intervention group and control group having 126,450 patients each. Survival for the two groups was analyzed using the Kaplan-Meier method. Complications were analyzed using the Cox proportional hazards model.
Results
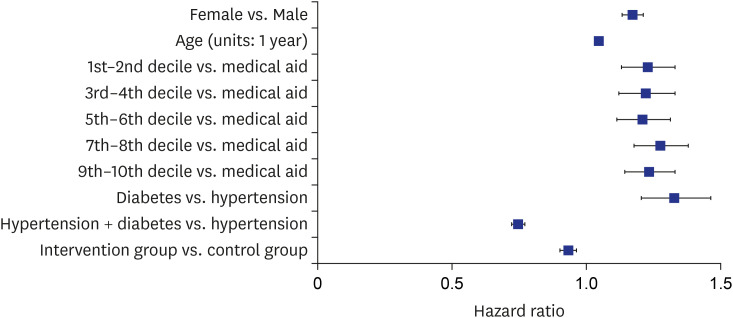
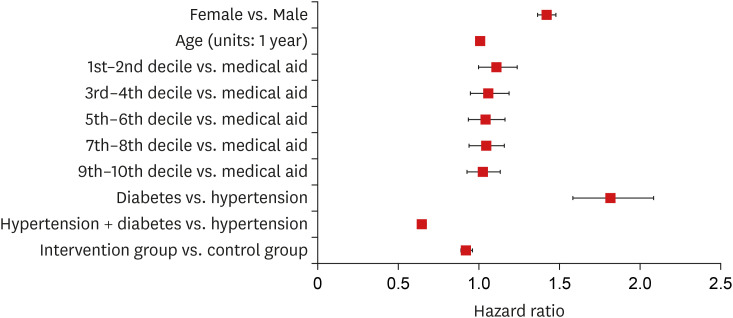
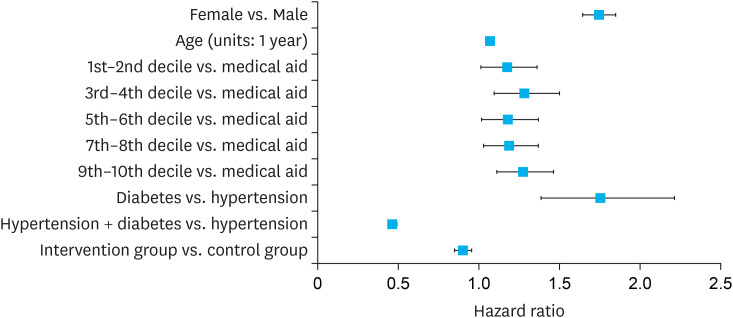
The 5-year survival rate in the intervention group (0.88) was higher than that in the control group (0.86). Cox proportional hazards analysis showed that the intervention group had lower risk for mortality (0.84; 95% confidence interval [CI], 0.82–0.86) compared to the control group. Hospitalization due to complications and the proportional risk of hospitalization were also lower in the intervention group.
Conclusion
The KCNPC model for prevention and control of chronic disease in Korea was found to be effective for hypertension and diabetes patients. Therefore, the KCNPC will be necessary to strengthen the capabilities of local communities, primary medical institutions, and individuals for prevention and control of chronic disease. Expanding the efficient prevention and control policies of the KCNPC to a nationwide scale may be effective as has been demonstrated through limited implementation in some regions.
Figure
Reference
-
1. Acheson D. Independent Inquiry into Inequalities in Health. London, UK: The Stationery Office;1998.2. Breslow L, Enstrom JE. Persistence of health habits and their relationship to mortality. Prev Med. 1980; 9(4):469–483. PMID: 7403016.
Article3. Belloc NB, Breslow L. Relationship of physical health status and health practices. Prev Med. 1972; 1(3):409–421. PMID: 5085007.
Article4. Brownson RC, Remingron PL, Davis JR. Chronic disease epidemiology and control. Washington, D.C.: American Public Health Association;1993.5. World Health Organization. WHO Global NCD Action Plan 2013-2020. Geneva, Switzerland: World Health Organization;2013.6. University of Michigan, Center for Managing Chronic Disease. About chronic disease. Updated 2019. Accessed July 1, 2019. https://cmcd.sph.umich.edu/about/about-chronic-disease/.7. Statistics Korea. Causes of death statistics 2016. Updated 2017. Accessed July 27, 2019. http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=363695.8. Korea Centers for Disease Control & Prevention. Chronic Disease Status and Issue 2018. Cheongju, Korea: Korea Centers for Disease Control & Prevention;2018.9. WHO Global NCD Action Plan. 2013-2020. World Health Organization;2013.10. United States Department of Health & Human Services. Centers for disease control and prevention. Updated 2019. Accessed July 1, 2019. https://www.cdc.gov/chronicdisease/about/index.htm.11. Busse R. Disease management programs in Germany's statutory health insurance system. Health Aff (Millwood). 2004; 23(3):56–67.
Article12. Pekka P, Erkki V, Tiina L, Pekka J, Meri P. The North Karelia Project: from North Karelia to National Action. Helsinki, Finland: National Institute for Health and Welfare (THL);2009.13. Yang HG, Lee DH. Achievements and challenges in a community based registration and management programme for hypertension and diabetes. Public Health Wkly Rep. 2015; 8(35):827–834.14. Yoon SJ. The Development of Model for Efficient Management of Hypertensive Patients and Diabetics. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2013.15. Lee HM, Kim YM, Lee CH, Shin JH, Kim MK, Choi BY. Awareness, treatment and control of hypertension and related factors in the jurisdictional areas of primary health care posts in a rural community of Korea. J Prev Med Public Health. 2011; 44(2):74–83. PMID: 21483226.
Article16. Macías I, del Collado F, Forte G. The effect of a community hypertension control program. Hypertension. 1988; 11(2 Pt 2):I194–7. PMID: 3346057.
Article17. Cho WS. The related of continuity of hospitalization and the medication adherence and health result for new patient with hypertension [master's thesis]. Seoul, Korea: Korea University;2010. p. 45–46.18. Park CM, Jang SM, Jang SH, Lee HJ. Analysis of Medical Costs and Health Outcomes Associated with Continuity of Care. Seoul, Korea: Health Insurance Review & Assessment Service;2010. p. 133–134.19. Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005; 43(6):521–530. PMID: 15908846.
Article20. Lim SM, Park YH, Jhang WG, Kim YT, Ahn EM, Kim GH, et al. Evaluation of community-based hypertension control programme in South Korea. Ann Acad Med Singapore. 2018; 47(4):143–148. PMID: 29777244.21. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002; 346(6):393–403. PMID: 11832527.
Article22. Stock S, Drabik A, Büscher G, Graf C, Ullrich W, Gerber A, et al. German diabetes management programs improve quality of care and curb costs. Health Aff (Millwood). 2010; 29(12):2197–2205. PMID: 21134920.
Article23. Rönnback M, Isomaa B, Fagerudd J, Forsblom C, Groop PH, Tuomi T, et al. Complex relationship between blood pressure and mortality in type 2 diabetic patients: a follow-up of the Botnia Study. Hypertension. 2006; 47(2):168–173. PMID: 16380522.24. Hakala SM, Tilvis RS, Strandberg TE. Blood pressure and mortality in an older population. A 5-year follow-up of the Helsinki Ageing Study. Eur Heart J. 1997; 18(6):1019–1023. PMID: 9183596.
Article25. Guo Z, Viitanen M, Winblad B. Low blood pressure and five-year mortality in a Stockholm cohort of the very old: possible confounding by cognitive impairment and other factors. Am J Public Health. 1997; 87(4):623–628. PMID: 9146442.
Article26. Kim MH, Jeong YW, Lee DH. Cardiovascular diseases prevention and control campaign, 2015. Public Health Wkly Rep. 2015; 8:925–928.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on the Factors in Relation to Job Performance of Community-Based Rehabilitation Program in Health Centers
- Development and Effects of a Community-Based Death Education Program for Older Adults
- The Association of Balance Confidence with Physical Performance and Strength in Community-Dwelling Elderly Persons
- Prevalence of Sarcopenia and its Risk Factors in Community-dwelling Older People during the COVID-19 Pandemic
- Self-Rated Health of the Chronic Disease Patients with Depression in Aged over 65