Ann Hepatobiliary Pancreat Surg.
2020 May;24(2):209-215. 10.14701/ahbps.2020.24.2.209.
Living donor liver transplantation for diffuse biliary papillomatosis with malignant change: A case report with 10-year follow-up
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2500808
- DOI: http://doi.org/10.14701/ahbps.2020.24.2.209
Abstract
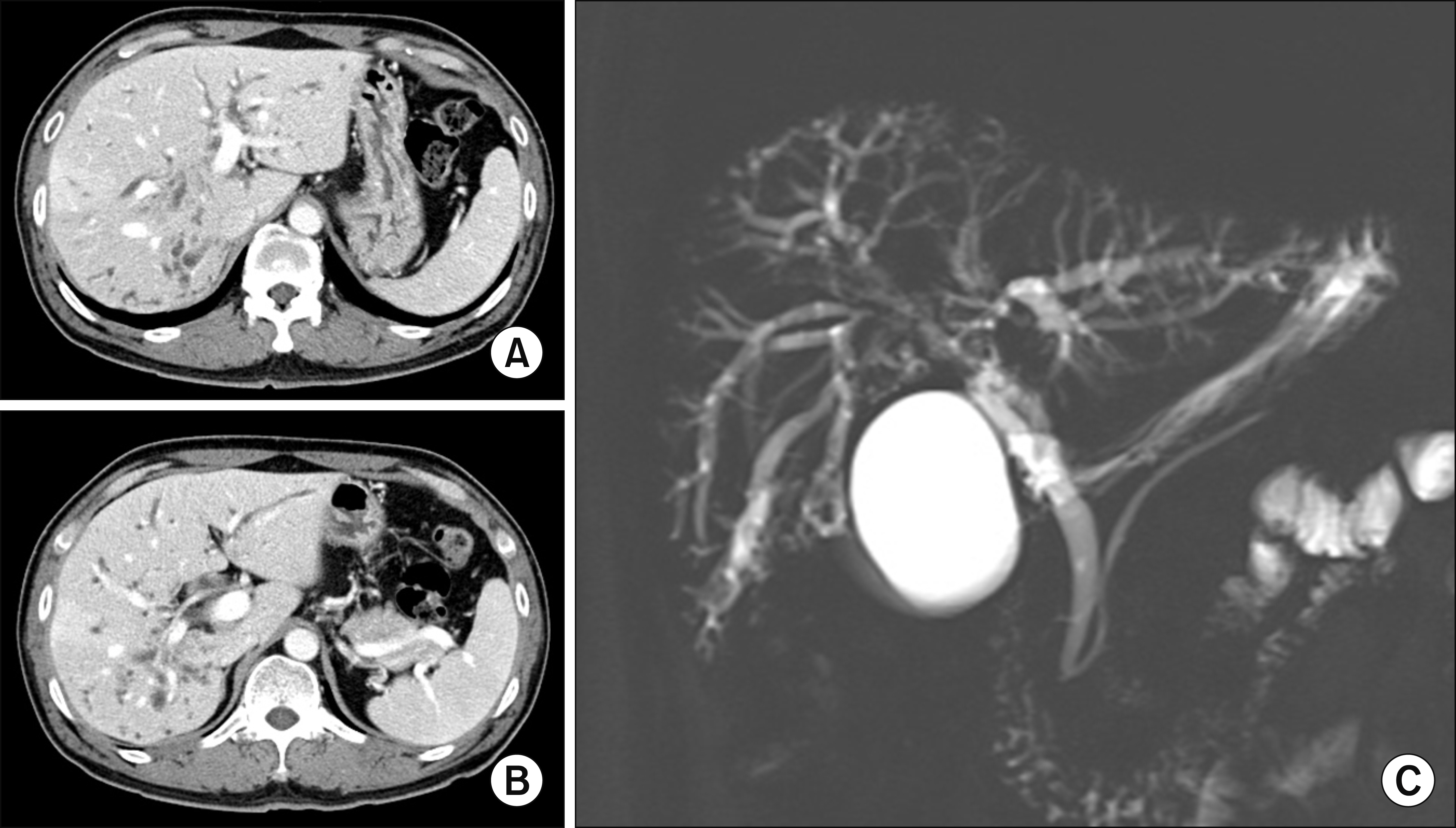
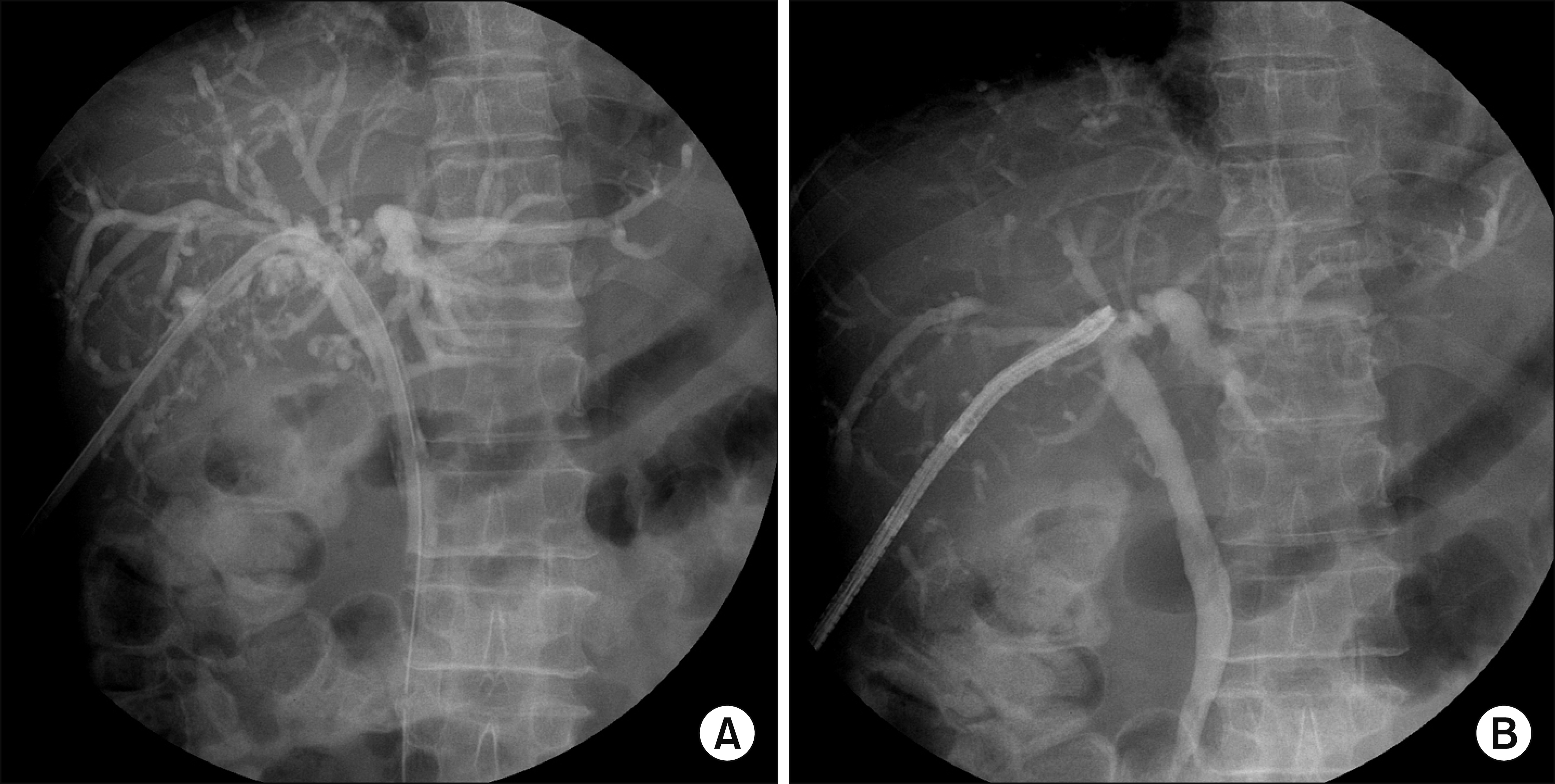
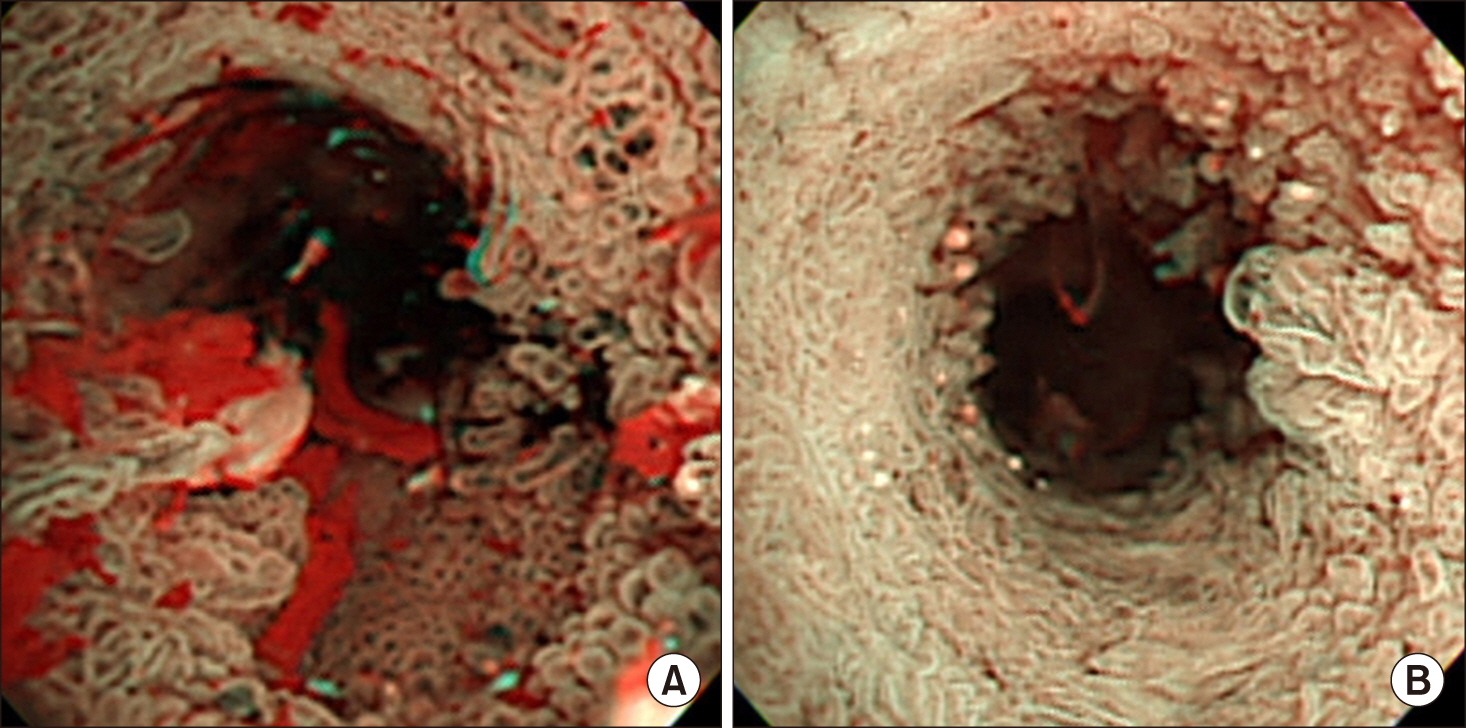
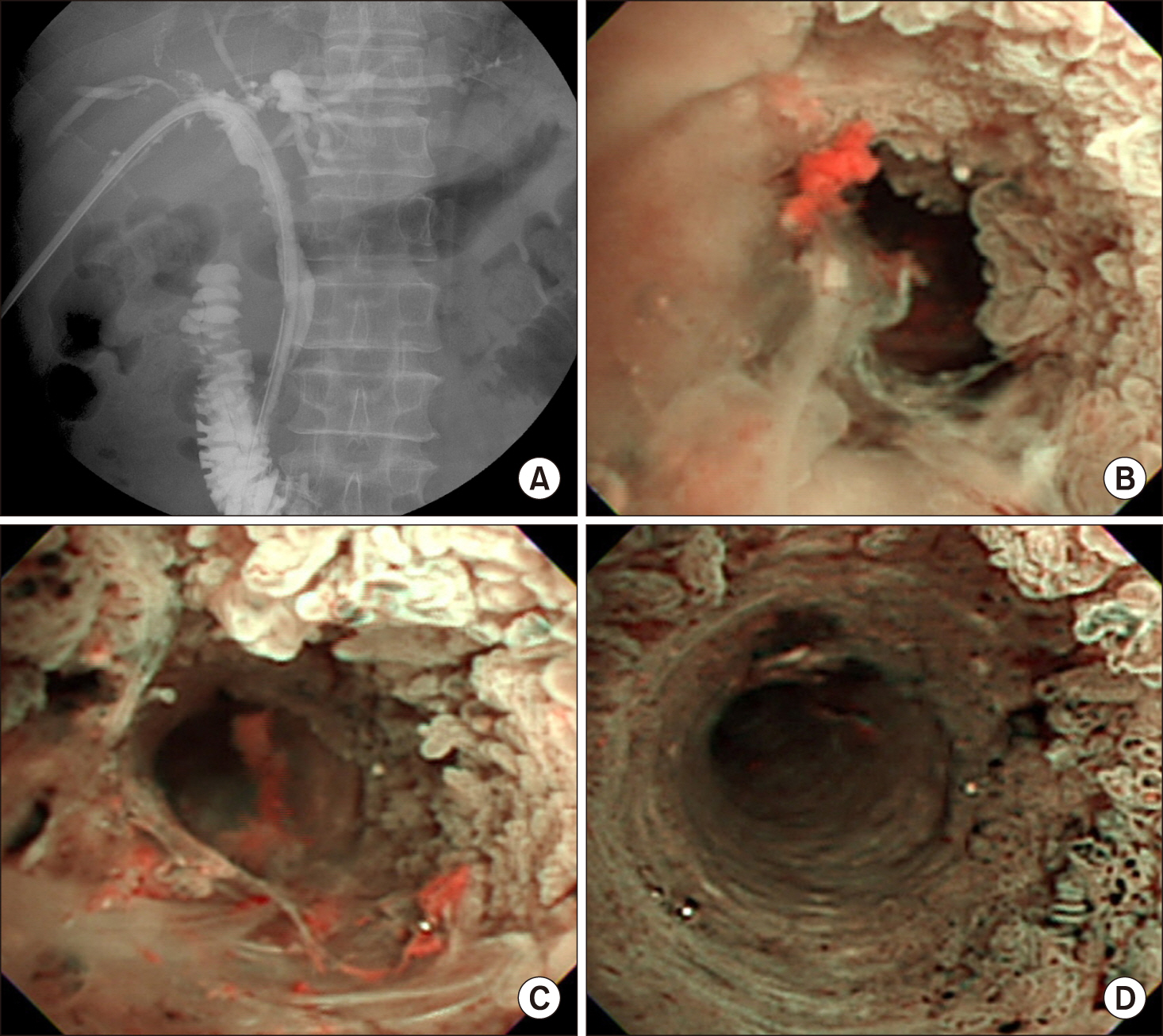
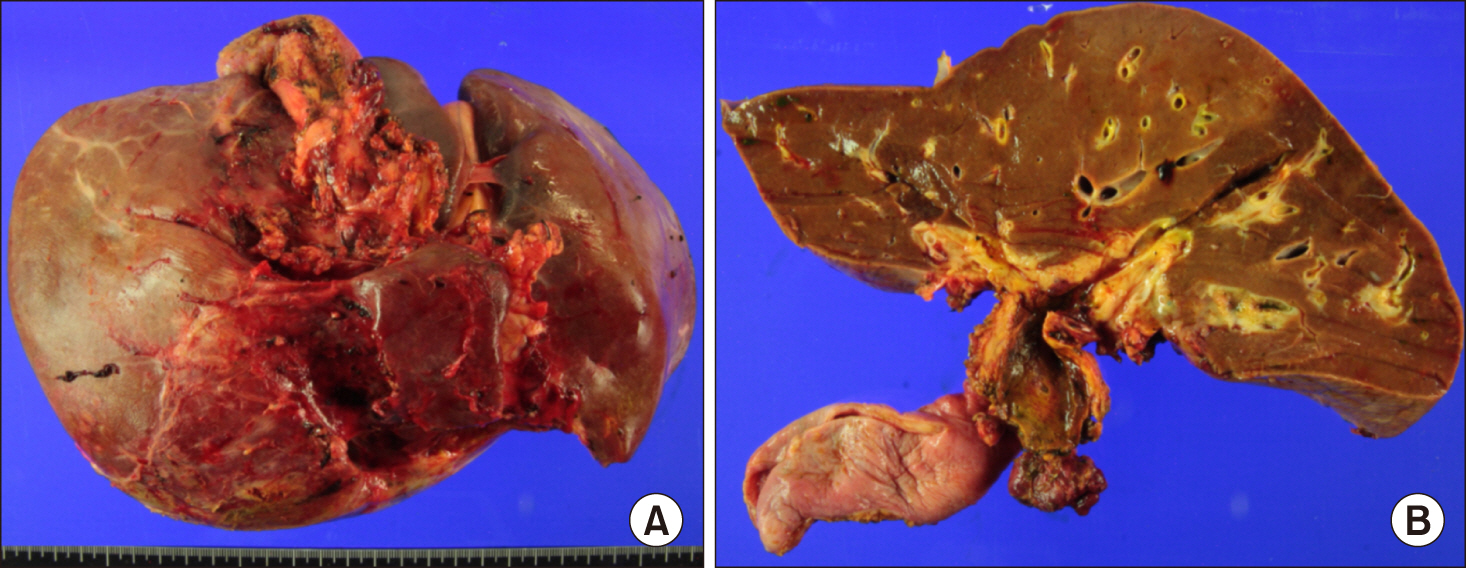
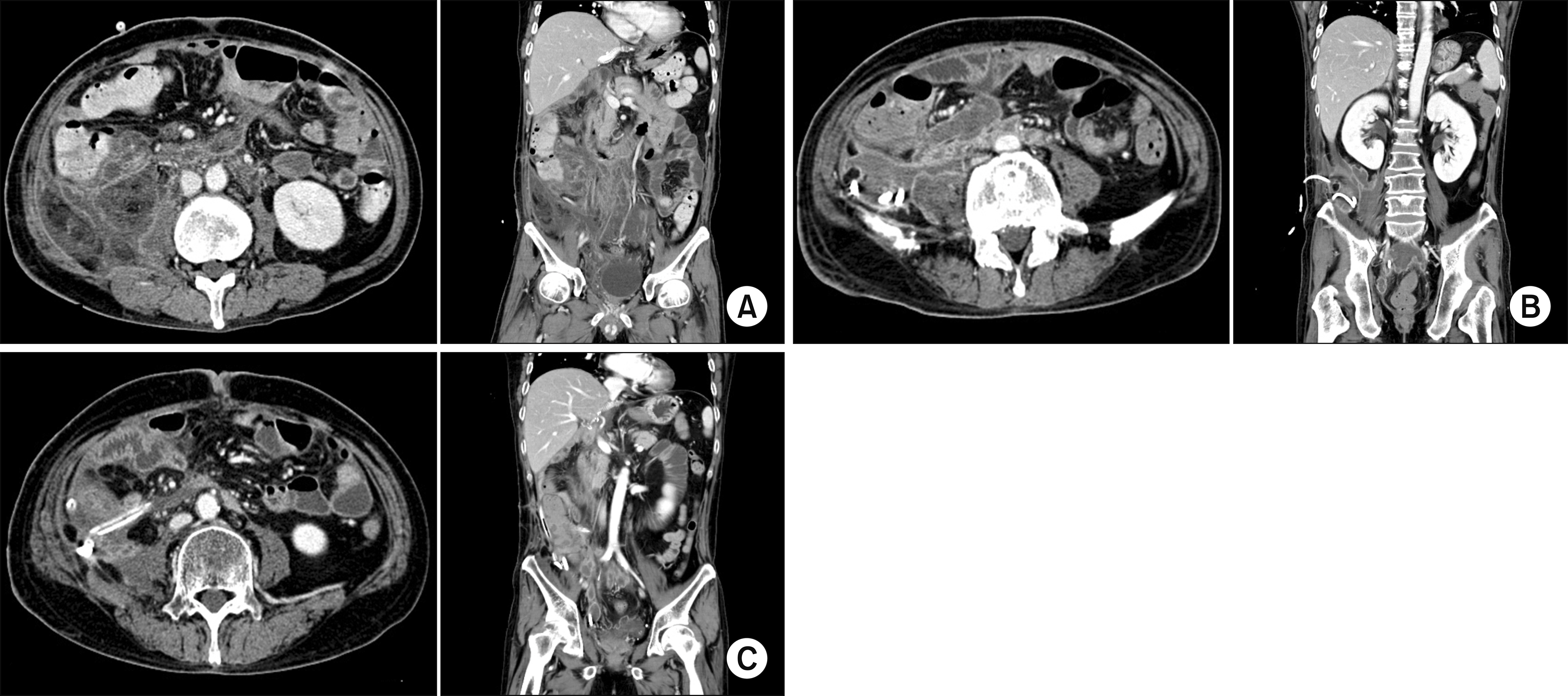
- Biliary papillomatosis is a rare disease of the biliary tract. In this study, we present a case of a male patient with biliary papillomatosis with malignant change who underwent living donor liver transplantation (LDLT). The 49-year-old man was admitted due to intrahepatic ductal mass, which was finally diagnosed as biliary papillomatosis. It was initially treated by photodynamic therapy, but LDLT was planned due to low efficacy of photodynamic therapy. LDLT was performed with a right liver graft from his son. The pathology report revealed intraductal papillary neoplasm with associated invasive carcinoma. He recovered uneventfully. Although the distal bile duct resection margin was free of tumor, the risk of tumor recurrence at the remnant intrahepatic bile duct still remained. Therefore, staged pylorus-preserving pancreatoduodenectomy was planned. However, after 3 months, he was readmitted due to retropancreatic abscess. It took 6 months to control the intractable retropancreatic abscess. Due to late development of retropancreatic abscess and its slow recovery, staged pancreatoduodenectomy was no longer considered. The patient recovered complete at 1 year posttransplant without any evidence of disease recurrence. After 5 years posttransplant, lung metastasis developed and pulmonary metastasectomy was performed three times. No further recurrence developed during the last 3 years to date, and the patient currently is alive, 10 years after the LDLT. Experience on our case and literature review suggest that patients with biliary papillomatosis with or without malignant transformation are selectively indicated for liver transplantation.
Keyword
Figure
Reference
-
1. Chappet V. 1894; Cancer epithelial primitif du canal cholédoque. Lyon Med. 76:145–157.2. Gu C, Lin YE, Jin H, Jian Z. 2015; Biliary papillomatosis with malignant transformation: a case report and review of the literature. Oncol Lett. 10:3315–3317. DOI: 10.3892/ol.2015.3682. PMID: 26722332. PMCID: PMC4665382.
Article3. Imvrios G, Papanikolaou V, Lalountas M, Patsiaoura K, Giakoustidis D, Fouzas I, et al. 2007; Papillomatosis of intra- and extrahepatic biliary tree: successful treatment with liver transplantation. Liver Transpl. 13:1045–1048. DOI: 10.1002/lt.21207. PMID: 17600352.
Article4. White AD, Young AL, Verbeke C, Brannan R, Smith A, Prasad KR. 2012; Biliary papillomatosis in three Caucasian patients in a Western centre. Eur J Surg Oncol. 38:181–184. DOI: 10.1016/j.ejso.2011.11.007. PMID: 22154963.
Article5. Vassiliou I, Kairi-Vassilatou E, Marinis A, Theodosopoulos T, Arkadopoulos N, Smyrniotis V. 2006; Malignant potential of intrahepatic biliary papillomatosis: a case report and review of the literature. World J Surg Oncol. 4:71. DOI: 10.1186/1477-7819-4-71. PMID: 17026772. PMCID: PMC1618388.
Article6. Li Z, Gao C, Zhang X, He Z, Abm K, Biswas S, et al. 2015; Intrahepatic biliary papillomatosis associated with malignant transformation: report of two cases and review of the literature. Int J Clin Exp Med. 8:21802–21806. PMID: 26885145. PMCID: PMC4723990.7. Cheng MS, AhChong AK, Mak KL, Yip AW. 1999; Case report: two cases of biliary papillomatosis with unusual associations. J Gastroenterol Hepatol. 14:464–467. DOI: 10.1046/j.1440-1746.1999.01895.x. PMID: 10355511.
Article8. Yeung YP, AhChong K, Chung CK, Chun AY. 2003; Biliary papillomatosis: report of seven cases and review of English literature. J Hepatobiliary Pancreat Surg. 10:390–395. DOI: 10.1007/s00534-002-0837-0. PMID: 14598142.
Article9. Bedossa P, Paradis V. Jarnagin WR, Belghiti J, Büchler MW, Chapman WC, D'Angelica MI, DeMatteo RP, editors. 2012. Tumors of the liver: pathologic aspects. Blumgart’s surgery of the liver, biliary tract, and pancreas. 5th ed. Elsevier Saunders;Philadelphia: p. 1223–1249.10. Lee SS, Kim MH, Lee SK, Jang SJ, Song MH, Kim KP, et al. 2004; Clinicopathologic review of 58 patients with biliary papillomatosis. Cancer. 100:783–793. DOI: 10.1002/cncr.20031. PMID: 14770435.
Article11. Ferraro D, Levi Sandri GB, Vennarecci G, Santoro R, Colasanti M, Meniconi RL, et al. 2019; Successful orthotopic liver transplant for diffuse biliary papillomatosis with malignant transformation: a case report with long-term follow-up. Exp Clin Transplant. 17:835–837. DOI: 10.6002/ect.2017.0134. PMID: 29534660.
Article12. Caso Maestro Ó, Justo Alonso I, Rodríguez Gil Y, Marcacuzco Quinto A, Calvo Pulido J, Jiménez Romero C. 2018; Tumor recurrence after liver transplantation for diffuse biliary papillomatosis in the absence of invasive carcinoma. Rev Esp Enferm Dig. 110:526–528. DOI: 10.17235/reed.2018.5557/2018. PMID: 29938516.13. Vibert E, Dokmak S, Belghiti J. 2010; Surgical strategy of biliary papillomatosis in Western countries. J Hepatobiliary Pancreat Sci. 17:241–245. DOI: 10.1007/s00534-009-0151-1. PMID: 19649560.
Article14. Bechmann LP, Hilgard P, Frilling A, Schumacher B, Baba HA, Gerken G, et al. 2008; Successful photodynamic therapy for biliary papillomatosis: a case report. World J Gastroenterol. 14:4234–4237. DOI: 10.3748/wjg.14.4234. PMID: 18636672. PMCID: PMC2725388.
Article15. Cheong CO, Lim JH, Park JS, Park SW, Kim HK, Kim KS. 2015; Volume-reserving surgery after photodynamic therapy for biliary papillomatosis: a case report. Korean J Gastroenterol. 66:55–58. DOI: 10.4166/kjg.2015.66.1.55. PMID: 26194131.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Anatomical limits in living donor liver transplantation
- Kaposi sarcoma of a liver graft in living donor liver transplantation: a rare case report
- Liver retransplantation for adult recipients