Clin Endosc.
2020 May;53(3):255-260. 10.5946/ce.2020.079.
Unilateral Versus Bilateral Biliary Drainage for Post-Transplant Anastomotic Stricture
- Affiliations
-
- 1Department of Internal Medicine and Liver Research Institute, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2502759
- DOI: http://doi.org/10.5946/ce.2020.079
Abstract
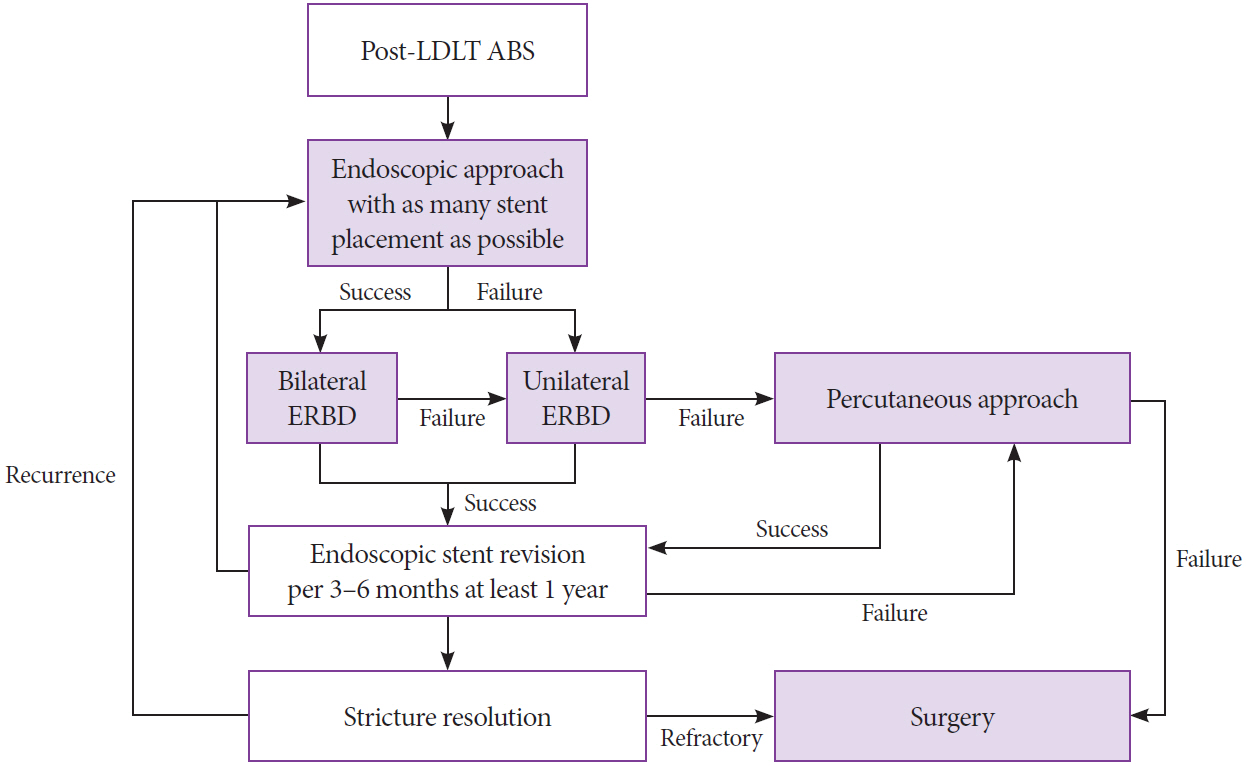
- Living donor liver transplantation is the most common type of liver transplantation in Asia. Post-transplant biliary stricture is frequent in living donor liver transplantation, and endoscopic management is considered to be the treatment of choice. However, endoscopic management is still challenging in patients who undergo right lobe living donor liver transplantation because of the anatomical alteration. In this article, we reviewed the recently updated results for proper endoscopic biliary drainage in post-living donor liver transplantation anatomical biliary stricture and compared unilateral and bilateral drainage.
Keyword
Figure
Reference
-
1. Rela M, Reddy MS. Living donor liver transplant (LDLT) is the way forward in Asia. Hepatol Int. 2017; 11:148–151.
Article2. Ishiko T, Egawa H, Kasahara M, et al. Duct-to-duct biliary reconstruction in living donor liver transplantation utilizing right lobe graft. Ann Surg. 2002; 236:235–240.
Article3. Santosh Kumar KY, Mathew JS, Balakrishnan D, et al. Intraductal transanastomotic stenting in duct-to-duct biliary reconstruction after living-donor liver transplantation: a randomized trial. J Am Coll Surg. 2017; 225:747–754.
Article4. Wan P, Yu X, Xia Q. Operative outcomes of adult living donor liver transplantation and deceased donor liver transplantation: a systematic review and meta-analysis. Liver Transpl. 2014; 20:425–436.
Article5. Akamatsu N, Sugawara Y, Hashimoto D. Biliary reconstruction, its complications and management of biliary complications after adult liver transplantation: a systematic review of the incidence, risk factors and outcome. Transpl Int. 2011; 24:379–392.
Article6. Balderramo D, Navasa M, Cardenas A. Current management of biliary complications after liver transplantation: emphasis on endoscopic therapy. Gastroenterol Hepatol. 2011; 34:107–115.
Article7. Mortele KJ, Ros PR. Anatomic variants of the biliary tree: MR cholangiographic findings and clinical applications. AJR Am J Roentgenol. 2001; 177:389–394.8. Tsujino T, Isayama H, Kogure H, Sato T, Nakai Y, Koike K. Endoscopic management of biliary strictures after living donor liver transplantation. Clin J Gastroenterol. 2017; 10:297–311.
Article9. Noack K, Bronk SF, Kato A, Gores GJ. The greater vulnerability of bile duct cells to reoxygenation injury than to anoxia. Implications for the pathogenesis of biliary strictures after liver transplantation. Transplantation. 1993; 56:495–500.10. Rao HB, Prakash A, Sudhindran S, Venu RP. Biliary strictures complicating living donor liver transplantation: problems, novel insights and solutions. World J Gastroenterol. 2018; 24:2061–2072.
Article11. Bismuth H. Surgical anatomy and anatomical surgery of the liver. World J Surg. 1982; 6:3–9.
Article12. Paik WH, Lee SH, Ryu JK, et al. Long-term clinical outcomes of biliary cast syndrome in liver transplant recipients. Liver Transpl. 2013; 19:275–282.
Article13. Lin TS, Chen CL, Concejero AM, et al. Early and long-term results of routine microsurgical biliary reconstruction in living donor liver transplantation. Liver Transpl. 2013; 19:207–214.
Article14. Seo JK, Ryu JK, Lee SH, et al. Endoscopic treatment for biliary stricture after adult living donor liver transplantation. Liver Transpl. 2009; 15:369–380.
Article15. Chok KS, Chan SC, Cheung TT, et al. Bile duct anastomotic stricture after adult-to-adult right lobe living donor liver transplantation. Liver Transpl. 2011; 17:47–52.
Article16. Na GH, Kim DG, Choi HJ, Han JH, Hong TH, You YK. Interventional treatment of a biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis. HPB (Oxford). 2014; 16:312–319.
Article17. Kyoden Y, Tamura S, Sugawara Y, et al. Incidence and management of biliary complications after adult-to-adult living donor liver transplantation. Clin Transplant. 2010; 24:535–542.
Article18. Zoepf T, Maldonado-Lopez EJ, Hilgard P, et al. Balloon dilatation vs. balloon dilatation plus bile duct endoprostheses for treatment of anastomotic biliary strictures after liver transplantation. Liver Transpl. 2006; 12:88–94.
Article19. You MS, Paik WH, Choi YH, et al. Optimal biliary drainage for patients with biliary anastomotic strictures after right lobe living donor liver transplantation. Liver Transpl. 2019; 25:1209–1219.
Article20. Jang SI, Sung SY, Park H, Lee KH, Joo SM, Lee DK. Salvage therapy using self-expandable metal stents for recalcitrant anastomotic strictures after living-donor liver transplantation. Therap Adv Gastroenterol. 2017; 10:297–309.
Article21. Kurita A, Kodama Y, Minami R, et al. Endoscopic stent placement above the intact sphincter of Oddi for biliary strictures after living donor liver transplantation. J Gastroenterol. 2013; 48:1097–1104.
Article22. Hsieh TH, Mekeel KL, Crowell MD, et al. Endoscopic treatment of anastomotic biliary strictures after living donor liver transplantation: outcomes after maximal stent therapy. Gastrointest Endosc. 2013; 77:47–54.
Article23. Lee YY, Gwak GY, Lee KH, et al. Predictors of the feasibility of primary endoscopic management of biliary strictures after adult living donor liver transplantation. Liver Transpl. 2011; 17:1467–1473.
Article24. Kim TH, Lee SK, Han JH, et al. The role of endoscopic retrograde cholangiography for biliary stricture after adult living donor liver transplantation: technical aspect and outcome. Scand J Gastroenterol. 2011; 46:188–196.
Article25. Chang JH, Lee IS, Choi JY, et al. Biliary stricture after adult right-lobe living-donor liver transplantation with duct-to-duct anastomosis: long-term outcome and its related factors after endoscopic treatment. Gut Liver. 2010; 4:226–233.
Article26. Kim ES, Lee BJ, Won JY, Choi JY, Lee DK. Percutaneous transhepatic biliary drainage may serve as a successful rescue procedure in failed cases of endoscopic therapy for a post-living donor liver transplantation biliary stricture. Gastrointest Endosc. 2009; 69:38–46.
Article27. Kato H, Kawamoto H, Tsutsumi K, et al. Long-term outcomes of endoscopic management for biliary strictures after living donor liver transplantation with duct-to-duct reconstruction. Transpl Int. 2009; 22:914–921.
Article28. Yazumi S, Yoshimoto T, Hisatsune H, et al. Endoscopic treatment of biliary complications after right-lobe living-donor liver transplantation with duct-to-duct biliary anastomosis. J Hepatobiliary Pancreat Surg. 2006; 13:502–510.
Article29. Tsujino T, Isayama H, Sugawara Y, et al. Endoscopic management of biliary complications after adult living donor liver transplantation. Am J Gastroenterol. 2006; 101:2230–2236.
Article30. Hisatsune H, Yazumi S, Egawa H, et al. Endoscopic management of biliary strictures after duct-to-duct biliary reconstruction in right-lobe living-donor liver transplantation. Transplantation. 2003; 76:810–815.
Article31. Parsi MA, Guardino J, Vargo JJ. Peroral cholangioscopy-guided stricture therapy in living donor liver transplantation. Liver Transpl. 2009; 15:263–265.
Article32. Woo YS, Lee JK, Noh DH, Park JK, Lee KH, Lee KT. SpyGlass cholangioscopy-assisted guidewire placement for post-LDLT biliary strictures: a case series. Surg Endosc. 2016; 30:3897–3903.
Article33. De Palma GD, Galloro G, Siciliano S, Iovino P, Catanzano C. Unilateral versus bilateral endoscopic hepatic duct drainage in patients with malignant hilar biliary obstruction: results of a prospective, randomized, and controlled study. Gastrointest Endosc. 2001; 53:547–553.
Article34. Polydorou AA, Chisholm EM, Romanos AA, et al. A comparison of right versus left hepatic duct endoprosthesis insertion in malignant hilar biliary obstruction. Endoscopy. 1989; 21:266–271.
Article35. Dowsett JF, Vaira D, Hatfield AR, et al. Endoscopic biliary therapy using the combined percutaneous and endoscopic technique. Gastroenterology. 1989; 96:1180–1186.
Article36. Lee TH, Kim TH, Moon JH, et al. Bilateral versus unilateral placement of metal stents for inoperable high-grade malignant hilar biliary strictures: a multicenter, prospective, randomized study (with video). Gastrointest Endosc. 2017; 86:817–827.37. Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc. 2010; 72:728–735.
Article38. Kerdsirichairat T, Arain MA, Attam R, et al. Endoscopic drainage of >50% of liver in malignant hilar biliary obstruction using metallic or fenestrated plastic stents. Clin Transl Gastroenterol. 2017; 8:e115.39. Tabibian JH, Asham EH, Han S, et al. Endoscopic treatment of postorthotopic liver transplantation anastomotic biliary strictures with maximal stent therapy (with video). Gastrointest Endosc. 2010; 71:505–512.
Article40. Tarantino I, Mangiavillano B, Di Mitri R, et al. Fully covered self-expandable metallic stents in benign biliary strictures: a multicenter study on efficacy and safety. Endoscopy. 2012; 44:923–927.
Article41. Park DH, Lee SS, Lee TH, et al. Anchoring flap versus flared end, fully covered self-expandable metal stents to prevent migration in patients with benign biliary strictures: a multicenter, prospective, comparative pilot study (with videos). Gastrointest Endosc. 2011; 73:64–70.
Article42. Tal AO, Finkelmeier F, Filmann N, et al. Multiple plastic stents versus covered metal stent for treatment of anastomotic biliary strictures after liver transplantation: a prospective, randomized, multicenter trial. Gastrointest Endosc. 2017; 86:1038–1045.43. Martins FP, De Paulo GA, Contini MLC, Ferrari AP. Metal versus plastic stents for anastomotic biliary strictures after liver transplantation: a randomized controlled trial. Gastrointest Endosc. 2018; 87:131.e1–e131.e13.
Article44. Kaffes A, Griffin S, Vaughan R, et al. A randomized trial of a fully covered self-expandable metallic stent versus plastic stents in anastomotic biliary strictures after liver transplantation. Therap Adv Gastroenterol. 2014; 7:64–71.
Article45. Curcio G, Traina M, Miraglia R, Tarantino I, Barresi L, Granata A. Treatment of a refractory biliary stricture after living donor liver transplantation, with a short fully covered metal stent with a long string. Endoscopy. 2012; 44 Suppl 2 UCTN:E74–E75.
Article46. Moon JH, Choi HJ, Koo HC, et al. Feasibility of placing a modified fully covered self-expandable metal stent above the papilla to minimize stent-induced bile duct injury in patients with refractory benign biliary strictures (with videos). Gastrointest Endosc. 2012; 75:1080–1085.
Article47. Morelli J, Mulcahy HE, Willner IR, Cunningham JT, Draganov P. Longterm outcomes for patients with post-liver transplant anastomotic biliary strictures treated by endoscopic stent placement. Gastrointest Endosc. 2003; 58:374–379.
Article48. Rerknimitr R, Sherman S, Fogel EL, et al. Biliary tract complications after orthotopic liver transplantation with choledochocholedochostomy anastomosis: endoscopic findings and results of therapy. Gastrointest Endosc. 2002; 55:224–231.
Article49. Morelli G, Fazel A, Judah J, Pan JJ, Forsmark C, Draganov P. Rapid-sequence endoscopic management of posttransplant anastomotic biliary strictures. Gastrointest Endosc. 2008; 67:879–885.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case with combined postoperative bile leakage and anastomotic stricture after liver transplantation treated with magnet compression anastomosis
- Endoscopic Stent Placement in the Palliation of Malignant Biliary Obstruction
- Balloon Dilatation and Bougienage of Post-operative Anastomotic Site Stricture of Upper G-I Tract
- Magnetic Compression Anastomosis for the Treatment of Post-Transplant Biliary Stricture
- Efficacy of Nasobiliary Tubes and Biliary Stents in Management of Patients with Bile Leak after Liver Transplantation: A Systematic Review