Blood Res.
2020 Mar;55(1):10-16. 10.5045/br.2020.55.1.10.
A general view of CD33⺠leukemic stem cells and CAR-T cells as interesting targets in acute myeloblatsic leukemia therapy
- Affiliations
-
- 1Department of Clinical Sciences, Faculty of Veterinary Medicine, University of Tabriz, Tabriz, Iran.
- 2Hematology and Oncology Research Center, Tabriz University of Medical Sciences, Tabriz, Iran. farahzadir@tbzmed.ac.ir
- 3Cellular and Molecular Research Center, Zahedan University of Medical Sciences, Zahedan, Iran.
- 4Division of Cell Biology, Biocenter, Medical University Innsbruck, Innsbruck, Austria.
- KMID: 2472003
- DOI: http://doi.org/10.5045/br.2020.55.1.10
Abstract
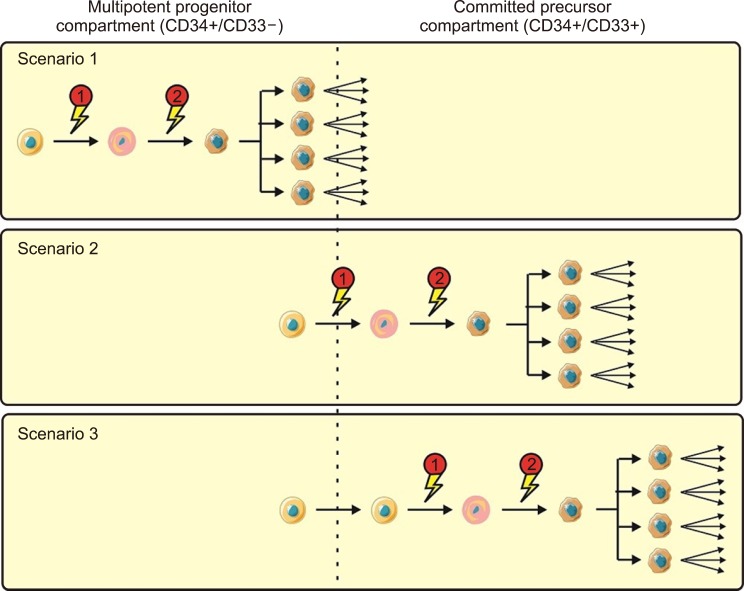
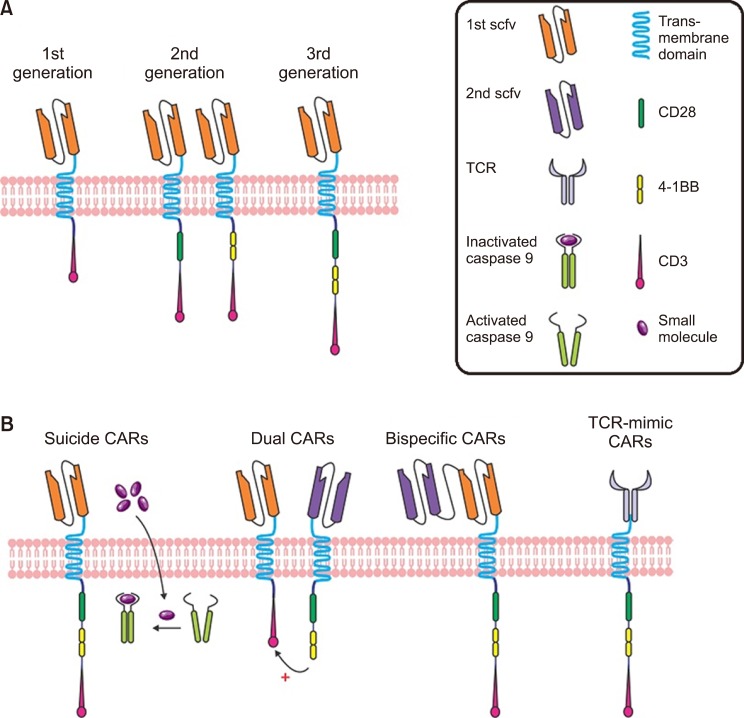
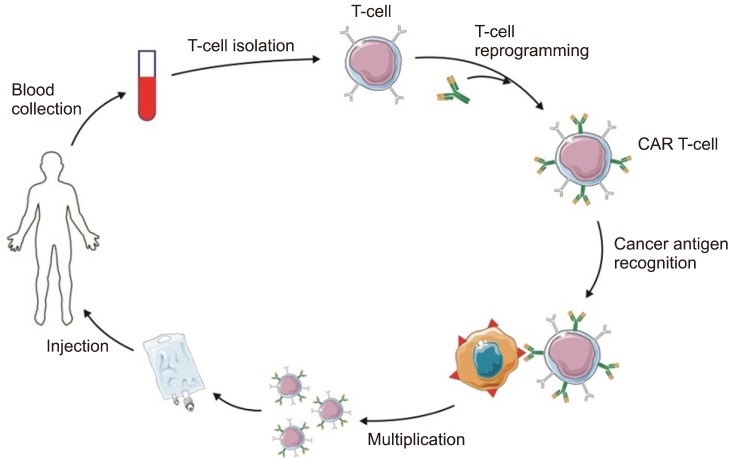
- Acute myeloblastic leukemia (AML) is the most frequent acute leukemia in adulthood with very poor overall survival rates. In the past few decades, significant progresses had led to the findings of new therapeutic approaches and the better understanding of the molecular complexity of this hematologic malignancy. Leukemic stem cells (LSCs) play a key role in the initiation, progression, regression, and drug resistance of different types of leukemia. The cellular and molecular characteristics of LSCs and their mechanism in the development of leukemia had not yet been specified. Therefore, determining their cellular and molecular characteristics and creating new approaches for targeted therapy of LSCs is crucial for the future of leukemia research. For this reason, the recognition of surface maker targets on the cell surface of LSCs has attracted much attention. CD33 has been detected on blasts in most AML patients, making them an interesting target for AML therapy. Genetic engineering of T cells with chimeric antigen receptor (CAR-T cell therapy) is a novel therapeutic strategy. It extends the range of antigens available for use in adoptive T-cell immunotherapy. This review will focus on CAR-T cell approaches as well as monoclonal antibody (mAB)-based therapy, the two antibody-based therapies utilized in AML treatment.
Keyword
MeSH Terms
Figure
Reference
-
1. Ehninger A, Kramer M, Röllig C, et al. Distribution and levels of cell surface expression of CD33 and CD123 in acute myeloid leukemia. Blood Cancer J. 2014; 4:e218. PMID: 24927407.
Article2. Walter RB, Appelbaum FR, Estey EH, Bernstein ID. Acute myeloid leukemia stem cells and CD33-targeted immunotherapy. Blood. 2012; 119:6198–6208. PMID: 22286199.
Article3. Röllig C, Bornhäuser M, Thiede C, et al. Long-term prognosis of acute myeloid leukemia according to the new genetic risk classification of the European LeukemiaNet recommendations: evaluation of the proposed reporting system. J Clin Oncol. 2011; 29:2758–2765. PMID: 21632498.
Article4. Reya T, Morrison SJ, Clarke MF, Weissman IL. Stem cells, cancer, and cancer stem cells. Nature. 2001; 414:105–111. PMID: 11689955.
Article5. Hofmann S, Schubert ML, Wang L, et al. Chimeric antigen receptor (CAR) T cell therapy in acute myeloid leukemia (AML). J Clin Med. 2019; 8:E200. PMID: 30736352.
Article6. ten Cate B, de Bruyn M, Wei Y, Bremer E, Helfrich W. Targeted elimination of leukemia stem cells; a new therapeutic approach in hemato-oncology. Curr Drug Targets. 2010; 11:95–110. PMID: 20017722.7. Gorczyca W, Sun ZY, Cronin W, Li X, Mau S, Tugulea S. Immunophenotypic pattern of myeloid populations by flow cytometry analysis. Methods Cell Biol. 2011; 103:221–266. PMID: 21722806.
Article8. Schwonzen M, Diehl V, Dellanna M, Staib P. Immunophenotyping of surface antigens in acute myeloid leukemia by flow cytometry after red blood cell lysis. Leuk Res. 2007; 31:113–116. PMID: 16730795.
Article9. Hoyer JD, Grogg KL, Hanson CA, Gamez JD, Dogan A. CD33 detection by immunohistochemistry in paraffin-embedded tissues: a new antibody shows excellent specificity and sensitivity for cells of myelomonocytic lineage. Am J Clin Pathol. 2008; 129:316–323. PMID: 18208813.10. Hauswirth AW, Florian S, Printz D, et al. Expression of the target receptor CD33 in CD34+/CD38−/CD123+ AML stem cells. Eur J Clin Invest. 2007; 37:73–82. PMID: 17181570.11. Arndt C, von Bonin M, Cartellieri M, et al. Redirection of T cells with a first fully humanized bispecific CD33-CD3 antibody efficiently eliminates AML blasts without harming hematopoietic stem cells. Leukemia. 2013; 27:964–967. PMID: 23325142.
Article12. Carnero A, Garcia-Mayea Y, Mir C, Lorente J, Rubio IT, LLeonart ME. The cancer stem-cell signaling network and resistance to therapy. Cancer Treat Rev. 2016; 49:25–36. PMID: 27434881.
Article13. Rosen JM, Jordan CT. The increasing complexity of the cancer stem cell paradigm. Science. 2009; 324:1670–1673. PMID: 19556499.
Article14. Lapidot T, Sirard C, Vormoor J, et al. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature. 1994; 367:645–648. PMID: 7509044.
Article15. Al-Hajj M, Wicha MS, Benito-Hernandez A, Morrison SJ, Clarke MF. Prospective identification of tumorigenic breast cancer cells. Proc Natl Acad Sci U S A. 2003; 100:3983–3988. PMID: 12629218.
Article16. Singh SK, Clarke ID, Terasaki M, et al. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003; 63:5821–5828. PMID: 14522905.17. Yu Z, Baserga R, Chen L, Wang C, Lisanti MP, Pestell RG. microRNA, cell cycle, and human breast cancer. Am J Pathol. 2010; 176:1058–1064. PMID: 20075198.
Article18. Yu Z, Pestell TG, Lisanti MP, Pestell RG. Cancer stem cells. Int J Biochem Cell Biol. 2012; 44:2144–2151. PMID: 22981632.
Article19. Wang X, Huang S, Chen JL. Understanding of leukemic stem cells and their clinical implications. Mol Cancer. 2017; 16:2. PMID: 28137304.
Article20. Yang X, Xu X, Liu Y, et al. Advances in acute myeloid leukemia stem cells. In : Hamid GA, editor. Advances in hematologic malignancies. London, UK: IntechOpen;2019.21. Dick JE. Stem cell concepts renew cancer research. Blood. 2008; 112:4793–4807. PMID: 19064739.
Article22. Colmone A, Amorim M, Pontier AL, Wang S, Jablonski E, Sipkins DA. Leukemic cells create bone marrow niches that disrupt the behavior of normal hematopoietic progenitor cells. Science. 2008; 322:1861–1865. PMID: 19095944.
Article23. Bonnet D, Dick JE. Human acute myeloid leukemia is organized as a hierarchy that originates from a primitive hematopoietic cell. Nat Med. 1997; 3:730–737. PMID: 9212098.
Article24. Fialkow PJ, Singer JW, Adamson JW, et al. Acute nonlymphocytic leukemia: heterogeneity of stem cell origin. Blood. 1981; 57:1068–1073. PMID: 6939452.
Article25. Bernstein ID, Singer JW, Smith FO, et al. Differences in the frequency of normal and clonal precursors of colony-forming cells in chronic myelogenous leukemia and acute myelogenous leukemia. Blood. 1992; 79:1811–1816. PMID: 1373089.26. Chao MP, Seita J, Weissman IL. Establishment of a normal hematopoietic and leukemia stem cell hierarchy. Cold Spring Harb Symp Quant Biol. 2008; 73:439–449. PMID: 19022770.
Article27. Goardon N, Marchi E, Atzberger A, et al. Coexistence of LMPP-like and GMP-like leukemia stem cells in acute myeloid leukemia. Cancer Cell. 2011; 19:138–152. PMID: 21251617.
Article28. Taussig DC, Pearce DJ, Simpson C, et al. Hematopoietic stem cells express multiple myeloid markers: implications for the origin and targeted therapy of acute myeloid leukemia. Blood. 2005; 106:4086–4092. PMID: 16131573.
Article29. Jordan CT, Guzman ML. Mechanisms controlling pathogenesis and survival of leukemic stem cells. Oncogene. 2004; 23:7178–7187. PMID: 15378078.
Article30. Fialkow PJ, Singer JW, Raskind WH, et al. Clonal development, stem-cell differentiation, and clinical remissions in acute nonlymphocytic leukemia. N Engl J Med. 1987; 317:468–473. PMID: 3614291.
Article31. Grimwade D, Enver T. Acute promyelocytic leukemia: where does it stem from? Leukemia. 2004; 18:375–384. PMID: 14737069.
Article32. Garfin PM, Feldman EJ. Antibody-based treatment of acute myeloid leukemia. Curr Hematol Malig Rep. 2016; 11:545–552. PMID: 27734262.
Article33. Bernstein ID. CD33 as a target for selective ablation of acute myeloid leukemia. Clin Lymphoma. 2002; 2 Suppl 1:S9–S11. PMID: 11970770.
Article34. van der Velden VH, Boeckx N, Jedema I, et al. High CD33-antigen loads in peripheral blood limit the efficacy of gemtuzumab ozogamicin (Mylotarg) treatment in acute myeloid leukemia patients. Leukemia. 2004; 18:983–988. PMID: 15029214.
Article35. Laszlo GS, Estey EH, Walter RB. The past and future of CD33 as therapeutic target in acute myeloid leukemia. Blood Rev. 2014; 28:143–153. PMID: 24809231.
Article36. Abdool A, Yeh CH, Kantarjian H, et al. Circulating CD33 and its clinical value in acute leukemia. Exp Hematol. 2010; 38:462–471. PMID: 20362641.
Article37. Raghavan PR. Metadichol and CD33 expression in umbilical cord cells. J Stem Cell Res Ther. 2019; 9:1000443.
Article38. Jurcic JG. What happened to anti-CD33 therapy for acute myeloid leukemia? Curr Hematol Malig Rep. 2012; 7:65–73. PMID: 22109628.
Article39. Chari RV, Miller ML, Widdison WC. Antibody-drug conjugates: an emerging concept in cancer therapy. Angew Chem Int Ed Engl. 2014; 53:3796–3827. PMID: 24677743.
Article40. Caron PC, Dumont L, Scheinberg DA. Supersaturating infusional humanized anti-CD33 monoclonal antibody HuM195 in myelogenous leukemia. Clin Cancer Res. 1998; 4:1421–1428. PMID: 9626458.41. Borot F, Wang H, Ma Y, et al. Gene-edited stem cells enable CD33-directed immune therapy for myeloid malignancies. Proc Natl Acad Sci U S A. 2019; 116:11978–11987. PMID: 31138698.
Article42. Kolb HJ, Schmid C, Barrett AJ, Schendel DJ. Graft-versus-leukemia reactions in allogeneic chimeras. Blood. 2004; 103:767–776. PMID: 12958064.
Article43. Jensen MC, Popplewell L, Cooper LJ, et al. Antitransgene rejection responses contribute to attenuated persistence of adoptively transferred CD20/CD19-specific chimeric antigen receptor redirected T cells in humans. Biol Blood Marrow Transplant. 2010; 16:1245–1256. PMID: 20304086.
Article44. Wang E, Wang LC, Tsai CY, et al. Generation of potent T-cell immunotherapy for cancer using DAP12-based, multichain, chimeric immunoreceptors. Cancer Immunol Res. 2015; 3:815–826. PMID: 25941351.
Article45. Guedan S, Chen X, Madar A, et al. ICOS-based chimeric antigen receptors program bipolar TH17/TH1 cells. Blood. 2014; 124:1070–1080. PMID: 24986688.
Article46. Ruella M, Barrett DM, Kenderian SS, et al. Dual CD19 and CD123 targeting prevents antigen-loss relapses after CD19-directed immunotherapies. J Clin Invest. 2016; 126:3814–3826. PMID: 27571406.
Article47. Wilkie S, van Schalkwyk MC, Hobbs S, et al. Dual targeting of ErbB2 and MUC1 in breast cancer using chimeric antigen receptors engineered to provide complementary signaling. J Clin Immunol. 2012; 32:1059–1070. PMID: 22526592.
Article48. Zah E, Lin MY, Silva-Benedict A, Jensen MC, Chen YY. T cells expressing CD19/CD20 bispecific chimeric antigen receptors prevent antigen escape by malignant B cells. Cancer Immunol Res. 2016; 4:498–508. PMID: 27059623.
Article49. Alcantara M, Tesio M, June CH, Houot R. CAR T-cells for T-cell malignancies: challenges in distinguishing between therapeutic, normal, and neoplastic T-cells. Leukemia. 2018; 32:2307–2315. PMID: 30315238.
Article50. Lamers CH, Sleijfer S, van Steenbergen S, et al. Treatment of metastatic renal cell carcinoma with CAIX CAR-engineered T cells: clinical evaluation and management of on-target toxicity. Mol Ther. 2013; 21:904–912. PMID: 23423337.
Article51. Sauer T, Rooney CM. Current challenges for CAR T-cell therapy of acute myeloid leukemia. Transfusion. 2019; 59:1171–1173. PMID: 30762880.
Article52. Hills RK, Castaigne S, Appelbaum FR, et al. Addition of gemtuzumab ozogamicin to induction chemotherapy in adult patients with acute myeloid leukaemia: a meta-analysis of individual patient data from randomised controlled trials. Lancet Oncol. 2014; 15:986–996. PMID: 25008258.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Human acute myeloid leukemia stem cells: evolution of concept
- Relapse of Biphenotypic Acute Leukemia as a Breast Mass
- Inactivation of the NHEJ Activity of DNA-PKcs Prevents Fanconi Anemia Pre-Leukemic HSC Expansion
- Immunotherapy using Dendritic Cells against Acute Myelogenous Leukemia
- Generation of Leukemic Dendritic Cells from Patients with Acute Myelogenous Leukemia