Chest Radiographic and CT Findings of the 2019 Novel Coronavirus Disease (COVID-19): Analysis of Nine Patients Treated in Korea
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine, Seoul National University Hospital, Seoul, Korea. yshoka@gmail.com
- 2Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 3Department of Internal Medicine, Incheon Medical Center, Incheon, Korea.
- 4Department of Radiology, Seoul Medical Center, Seoul, Korea.
- 5Department of Radiology, National Medical Center, Seoul, Korea.
- 6Department of Radiology, Myongji Hospital, Goyang, Korea.
- 7Department of Radiology, Chonnam National University Hospital, Gwangju, Korea.
- KMID: 2471815
- DOI: http://doi.org/10.3348/kjr.2020.0132
Abstract
OBJECTIVE
This study presents a preliminary report on the chest radiographic and computed tomography (CT) findings of the 2019 novel coronavirus disease (COVID-19) pneumonia in Korea.
MATERIALS AND METHODS
As part of a multi-institutional collaboration coordinated by the Korean Society of Thoracic Radiology, we collected nine patients with COVID-19 infections who had undergone chest radiography and CT scans. We analyzed the radiographic and CT findings of COVID-19 pneumonia at baseline. Fisher's exact test was used to compare CT findings depending on the shape of pulmonary lesions.
RESULTS
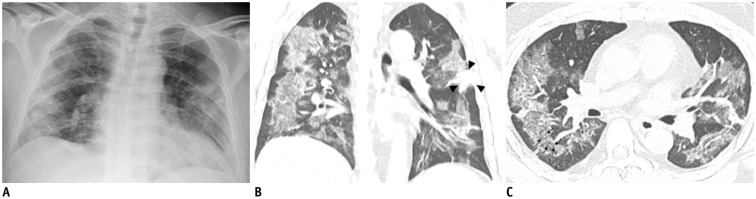
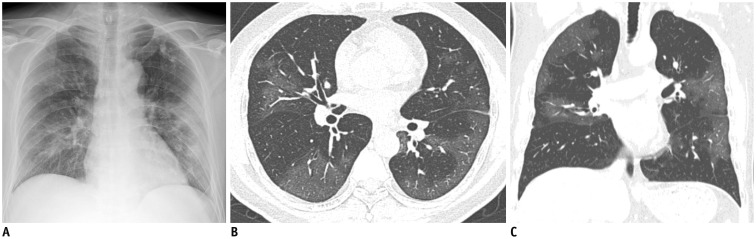
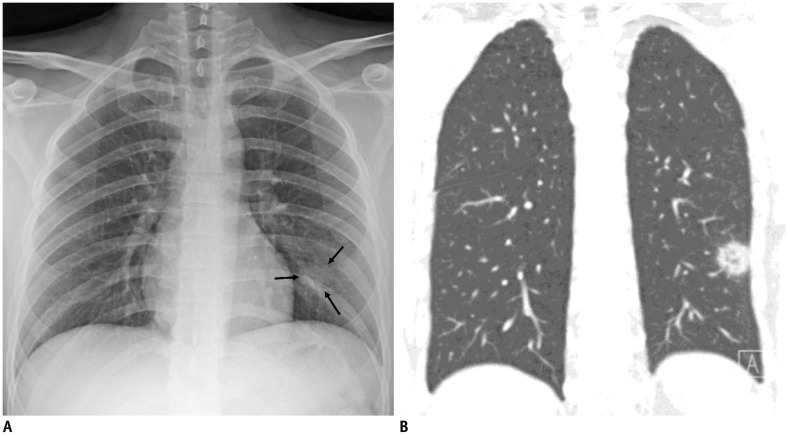
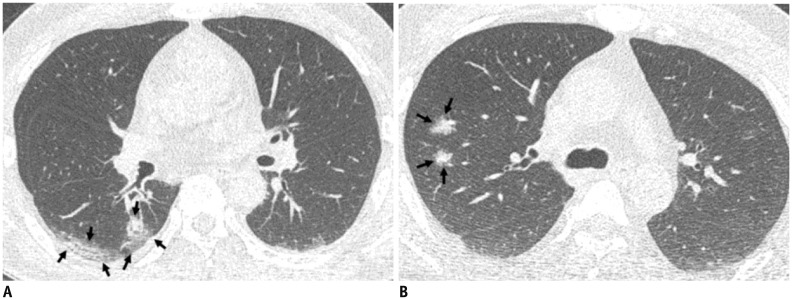
Three of the nine patients (33.3%) had parenchymal abnormalities detected by chest radiography, and most of the abnormalities were peripheral consolidations. Chest CT images showed bilateral involvement in eight of the nine patients, and a unilobar reversed halo sign in the other patient. In total, 77 pulmonary lesions were found, including patchy lesions (39%), large confluent lesions (13%), and small nodular lesions (48%). The peripheral and posterior lung fields were involved in 78% and 67% of the lesions, respectively. The lesions were typically ill-defined and were composed of mixed ground-glass opacities and consolidation or pure ground-glass opacities. Patchy to confluent lesions were primarily distributed in the lower lobes (p = 0.040) and along the pleura (p < 0.001), whereas nodular lesions were primarily distributed along the bronchovascular bundles (p = 0.006).
CONCLUSION
COVID-19 pneumonia in Korea primarily manifested as pure to mixed ground-glass opacities with a patchy to confluent or nodular shape in the bilateral peripheral posterior lungs. A considerable proportion of patients with COVID-19 pneumonia had normal chest radiographs.
Keyword
MeSH Terms
Figure
Cited by 5 articles
-
Revised Triage and Surveillance Protocols for Temporary Emergency Department Closures in Tertiary Hospitals as a Response to COVID-19 Crisis in Daegu Metropolitan City
Han Sol Chung, Dong Eun Lee, Jong Kun Kim, In Hwan Yeo, Changho Kim, Jungbae Park, Kang Suk Seo, Sin-Yul Park, Jung Ho Kim, Gyunmoo Kim, Suk Hee Lee, Jeon Jae Cheon, Yang Hun Kim
J Korean Med Sci. 2020;35(19):e189. doi: 10.3346/jkms.2020.35.e189.Adverse Initial CT Findings Associated with Poor Prognosis of Coronavirus Disease
YoungJun Chon, Jin Young Kim, Young Joo Suh, Ji Yeon Lee, Jae Seok Park, Sung Min Moon, Mu Sook Lee, Jaehyuck Yi
J Korean Med Sci. 2020;35(34):e316. doi: 10.3346/jkms.2020.35.e316.Establishment of a Nationwide Korean Imaging Cohort of Coronavirus Disease 2019
Soon Ho Yoon, Soo-Youn Ham, Bo Da Nam, Kum Ju Chae, Dabee Lee, Jin Young Yoo, So Hyeon Bak, Jin Young Kim, Jin Hwan Kim, Ki Beom Kim, Jung Im Jung, Jae-Kwang Lim, Jong Eun Lee, Myung Jin Chung, Young Kyung Lee, Young Seon Kim, Ji Eun Jo, Sang Min Lee, Woocheol Kwon, Chang Min Park, Yun-Hyeon Kim, Yeon Joo Jeong
J Korean Med Sci. 2020;35(46):e413. doi: 10.3346/jkms.2020.35.e413.Prognostic Implications of CT Feature Analysis in Patients with COVID-19: a Nationwide Cohort Study
Yeon Joo Jeong, Bo Da Nam, Jin Young Yoo, Kun-Il Kim, Hee Kang, Jung Hwa Hwang, Yun-Hyeon Kim, Kyung Soo Lee
J Korean Med Sci. 2021;36(8):e51. doi: 10.3346/jkms.2021.36.e51.The Clinical Manifestations and Chest Computed Tomography Findings of Coronavirus Disease 2019 (COVID-19) Patients in China: A Proportion Meta-Analysis
Joo-Hyun Park, Wook Jang, Sang-Woo Kim, Jeongjun Lee, Yun-Sung Lim, Chang-Gun Cho, Seok-Won Park, Bo Hae Kim
Clin Exp Otorhinolaryngol. 2020;13(2):95-105. doi: 10.21053/ceo.2020.00570.
Reference
-
1. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. China Novel Coronavirus Investigating and Research Team. A novel Coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020; 382:727–773. PMID: 31978945.
Article2. Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel Coronavirus-infected pneumonia. N Engl J Med. 2020; 1. 29. DOI: 10.1056/NEJMoa2001316. [Epub].
Article3. Coronavirus disease 2019 (COVID-19) situation report-27. World Health Organization Web site;2020. 2. 17. Accessed February 17, 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200216-sitrep-27-covid-19.pdf?sfvrsn=78c0eb78_2.4. Chung M, Bernheim A, Mei X, Zhang N, Huang M, Zeng X, et al. CT imaging features of 2019 novel Coronavirus (2019-nCoV). Radiology. 2020; 2. 04. DOI: 10.1148/radiol.2020200230. [Epub].5. Song F, Shi N, Shan F, Zhang Z, Shen J, Lu H, et al. Emerging coronavirus 2019-nCoV pneumonia. Radiology. 2020; 2. 06. DOI: 10.1148/radiol.2020200274. [Epub].6. Pan F, Ye T, Sun P, Gui S, Liang B, Li L, et al. Time course of lung changes on chest CT during recovery from 2019 novel Coronavirus (COVID-19) pneumonia. Radiology. 2020; 2. 13. DOI: 10.1148/radiol.2020200370. [Epub].7. Kim JY, Choe PG, Oh Y, Oh KJ, Kim J, Park SJ, et al. The first case of 2019 novel Coronavirus pneumonia imported into Korea from Wuhan, China: implication for infection prevention and control measures. J Korean Med Sci. 2020; 35:e61. PMID: 32030925.
Article8. Taylor E, Haven K, Reed P, Bissielo A, Harvey D, McArthur C, et al. SHIVERS Investigation Team. A chest radiograph scoring system in patients with severe acute respiratory infection: a validation study. BMC Med Imaging. 2015; 15:61. PMID: 26714630.
Article9. Hansell DM, Bankier AA, MacMahon H, McLoud TC, Müller NL, Remy J. Fleischner Society: glossary of terms for thoracic imaging. Radiology. 2008; 246:697–722. PMID: 18195376.
Article10. Ajlan AM, Ahyad RA, Jamjoom LG, Alharthy A, Madani TA. Middle East respiratory syndrome Coronavirus (MERS-CoV) infection: chest CT findings. AJR Am J Roentgenol. 2014; 203:782–787. PMID: 24918624.
Article11. Das KM, Lee EY, Enani MA, AlJawder SE, Singh R, Bashir S, et al. CT correlation with outcomes in 15 patients with acute Middle East respiratory syndrome coronavirus. AJR Am J Roentgenol. 2015; 204:736–742. PMID: 25615627.
Article12. Wong KT, Antonio GE, Hui DS, Lee N, Yuen EH, Wu A, et al. Thin-section CT of severe acute respiratory syndrome: evaluation of 73 patients exposed to or with the disease. Radiology. 2003; 228:395–400. PMID: 12738877.
Article13. Choi WJ, Lee KN, Kang EJ, Lee H. Middle East respiratory syndrome-Coronavirus infection: a case report of serial computed tomographic findings in a young male patient. Korean J Radiol. 2016; 17:166–170. PMID: 26798230.
Article14. Wan YL, Tsay PK, Cheung YC, Chiang PC, Wang CH, Tsai YH, et al. A correlation between the severity of lung lesions on radiographs and clinical findings in patients with severe acute respiratory syndrome. Korean J Radiol. 2007; 8:466–474. PMID: 18071276.
Article15. Antonio GE, Ooi CG, Wong KT, Tsui EL, Wong JS, Sy AN, et al. Radiographic-clinical correlation in severe acute respiratory syndrome: study of 1373 patients in Hong Kong. Radiology. 2005; 237:1081–1090. PMID: 16304120.
Article16. Wong KT, Antonio GE, Hui DS, Lee N, Yuen EH, Wu A, et al. Severe acute respiratory syndrome: radiographic appearances and pattern of progression in 138 patients. Radiology. 2003; 228:401–406. PMID: 12759474.
Article17. Das KM, Lee EY, Al Jawder SE, Enani MA, Singh R, Skakni L, et al. Acute Middle East respiratory syndrome Coronavirus: temporal lung changes observed on the chest radiographs of 55 patients. AJR Am J Roentgenol. 2015; 205:W267–W274. PMID: 26102309.
Article18. Lin X, Gong Z, Xiao Z, Xiong J, Fan B, Liu J. Novel Coronavirus pneumonia outbreak in 2019: computed tomographic findings in two cases. Korean J Radiol. 2020; 2. 11. DOI: 10.3348/kjr.2020.0078. [Epub].
Article19. Ng MY, Lee EYP, Yang J, Yang F, Li X, Wang H, et al. Imaging profile of the COVID-19 infection: radiologic findings and literature review. Radiol Cardiothorac Imaging. 2020; 2:e20003.
Article20. Fang Y, Zhang H, Xu Y, Xie J, Pang P, Ji W. CT manifestations of two cases of 2019 novel Coronavirus (2019-nCoV) pneumonia. Radiology. 2020; 2. 07. DOI: 10.1148/radiol.2020200280. [Epub].21. Kong W, Agarwal PP. Chest imaging appearance of COVID-19 infection. Radiol Cardiothorac Imaging. 2020; 2:e20002.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Radiologic Findings of COVID-19 Pneumonia: South Korean Experience from Three Cases
- Pulmonary Contusion Similar to COVID-19 Pneumonia
- 2019 Novel Coronavirus (COVID-19) Pneumonia: Serial Computed Tomography Findings
- Role of Chest Radiographs and CT Scans and the Application of Artificial Intelligence in Coronavirus Disease 2019
- Halo, Reversed Halo, or Both? Atypical Computed Tomography Manifestations of Coronavirus Disease (COVID-19) Pneumonia: The “Double Halo Sign”