Endocrinol Metab.
2020 Mar;35(1):149-156. 10.3803/EnM.2020.35.1.149.
Modification of the Tumor-Node-Metastasis Staging System for Differentiated Thyroid Carcinoma by Considering Extra-Thyroidal Extension and Lateral Cervical Lymph Node Metastasis
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. tykim@amc.seoul.kr
- 3Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea. drkang@chonnam.ac.kr
- 4Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea.
- 5Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 2471731
- DOI: http://doi.org/10.3803/EnM.2020.35.1.149
Abstract
- BACKGROUND
Concerns have arisen about the classification of extra-thyroidal extension (ETE) and lateral cervical lymph node metastasis (N1b) in the 8th edition of the tumor-node-metastasis staging system (TNM-8). This study evaluated the prognostic validity of a modified-TNM staging system, focusing on ETE and N1b, in differentiated thyroid carcinoma (DTC) patients.
METHODS
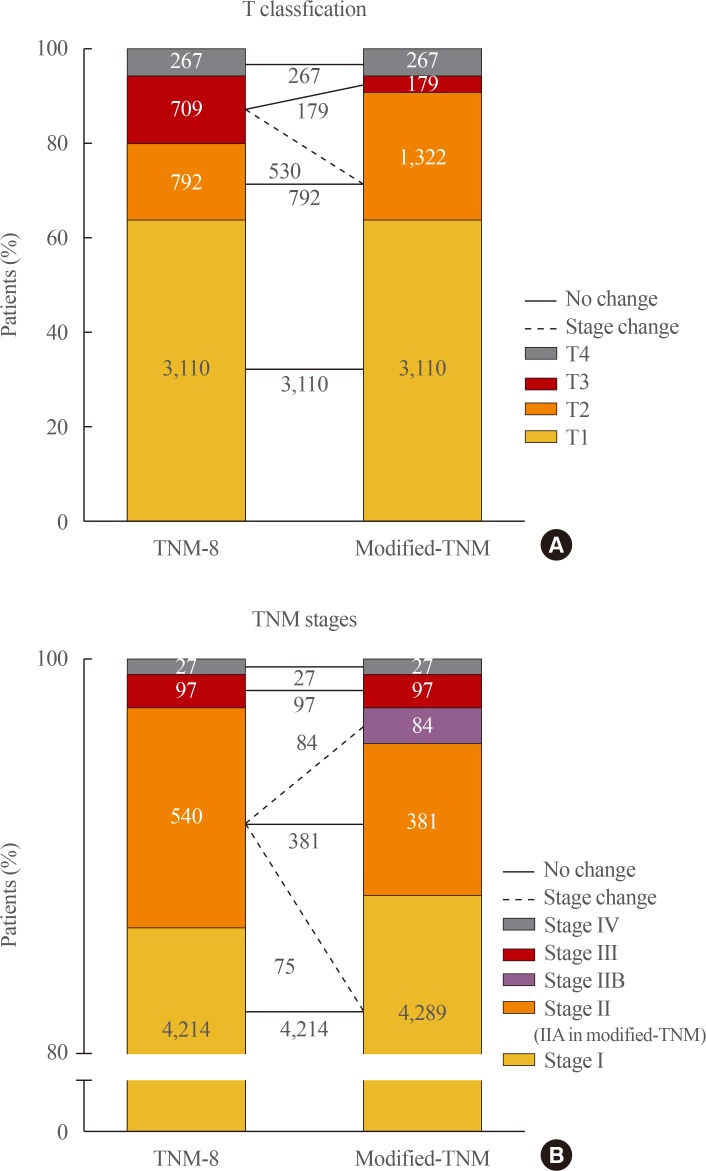
This multicenter retrospective cohort study included 4,878 DTC patients from five tertiary hospitals. In the modified-TNM, T3b in TNM-8 was down-staged to T2, and stage II was subdivided into stages IIA and IIB. Older patients with N1b were reclassified as stage IIB.
RESULTS
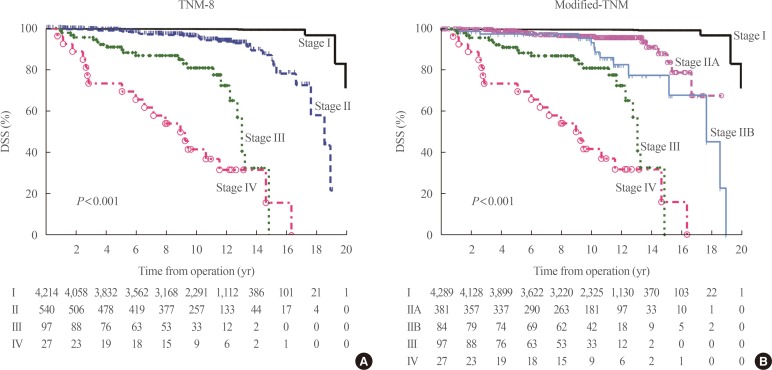
The modified-TNM resulted in staging migration in 540 patients (11%) classified as stage II according to the TNM-8, with 75 (14%), 381 (71%), and 84 patients (16%) classified as stages I, IIA, and IIB, respectively. The 10-year disease-specific survival (DSS) rates in patients classified as stages I, II, III, and IV by TNM-8 were 99.8%, 95.9%, 81.0%, and 41.6%, respectively. The DSS rates of patients classified as stages I, IIA, IIB, III, and IV according to the modified-TNM were 99.8%, 96.4%, 93.3%, 81.0%, and 41.6%, respectively. DSS curves between stages on TNM-8 (P<0.001) and modified-TNM (P<0.001) differed significantly, but the modified-TNM discriminated better than TNM-8. The proportions of variation explained values of TNM-8 and modified-TNM were 6.3% and 6.5%, respectively.
CONCLUSION
Modification of the TNM staging system focusing on ETE and N1b could improve the prediction of DSS in patients with DTC. Further researches are needed to validate the prognostic accuracy of this modified-TNM staging system.
Keyword
MeSH Terms
Figure
Reference
-
1. Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE, et al. 2015 American Thyroid Association Management Guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association Guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid. 2016; 26:1–133. PMID: 26462967.
Article2. Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010; 17:1471–1474. PMID: 20180029.
Article3. Edge SB. American Joint Committee on Cancer. AJCC cancer staging manual. 8th ed. New York: Springer International Publishing;2017.4. Tuttle RM, Haugen B, Perrier ND. Updated American Joint Committee on cancer/tumor-node-metastasis staging system for differentiated and anaplastic thyroid cancer (Eighth edition): what changed and why? Thyroid. 2017; 27:751–756. PMID: 28463585.
Article5. Kim M, Kim WG, Oh HS, Park S, Kwon H, Song DE, et al. Comparison of the seventh and eighth editions of the American Joint Committee on cancer/union for international cancer control tumor-node-metastasis staging system for differentiated thyroid cancer. Thyroid. 2017; 27:1149–1155. PMID: 28635571.
Article6. Kim TH, Kim YN, Kim HI, Park SY, Choe JH, Kim JH, et al. Prognostic value of the eighth edition AJCC TNM classification for differentiated thyroid carcinoma. Oral Oncol. 2017; 71:81–86. PMID: 28688696.
Article7. Song E, Lee YM, Oh HS, Jeon MJ, Song DE, Kim TY, et al. A relook at the T stage of differentiated thyroid carcinoma with a focus on gross extrathyroidal extension. Thyroid. 2019; 29:202–208. PMID: 30358515.
Article8. Park SY, Kim HI, Kim JH, Kim JS, Oh YL, Kim SW, et al. Prognostic significance of gross extrathyroidal extension invading only strap muscles in differentiated thyroid carcinoma. Br J Surg. 2018; 105:1155–1162. PMID: 29663333.
Article9. Kim M, Jeon MJ, Oh HS, Park S, Song DE, Sung TY, et al. Prognostic implication of N1b classification in the eighth edition of the tumor-node-metastasis staging system of differentiated thyroid cancer. Thyroid. 2018; 28:496–503. PMID: 29620964.
Article10. Kim M, Kim HK, Kim HI, Kim EH, Jeon MJ, Yi HS, et al. Modification of the eight-edition tumor-node-metastasis staging system with N1b for papillary thyroid carcinoma: a multi-institutional cohort study. Oral Oncol. 2018; 86:48–52. PMID: 30409319.
Article11. Schemper M, Stare J. Explained variation in survival analysis. Stat Med. 1996; 15:1999–2012. PMID: 8896135.
Article12. Amit M, Boonsripitayanon M, Goepfert RP, Tam S, Busaidy NL, Cabanillas ME, et al. Extrathyroidal extension: does strap muscle invasion alone influence recurrence and survival in patients with differentiated thyroid cancer? Ann Surg Oncol. 2018; 25:3380–3388. PMID: 30022274.
Article13. Ortiz S, Rodriguez JM, Soria T, Perez-Flores D, Pinero A, Moreno J, et al. Extrathyroid spread in papillary carcinoma of the thyroid: clinicopathological and prognostic study. Otolaryngol Head Neck Surg. 2001; 124:261–265. PMID: 11240987.
Article14. Andersen PE, Kinsella J, Loree TR, Shaha AR, Shah JP. Differentiated carcinoma of the thyroid with extrathyroidal extension. Am J Surg. 1995; 170:467–470. PMID: 7485734.
Article15. Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K, et al. Prognostic significance of extrathyroid extension of papillary thyroid carcinoma: massive but not minimal extension affects the relapse-free survival. World J Surg. 2006; 30:780–786. PMID: 16411013.
Article16. Woo CG, Sung CO, Choi YM, Kim WG, Kim TY, Shong YK, et al. Clinicopathological significance of minimal extrathyroid extension in solitary papillary thyroid carcinomas. Ann Surg Oncol. 2015; 22 Suppl 3:S728–S733. PMID: 26077913.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Significance of a Minimal Extra-thyroidal Extension of Papillary Thyroid Cancer for the Recurrence of Regional Cervical Lymph Nodes
- Lateral Neck Node Dissection in Differentiated Thyroid Carcinoma
- The Pattern of Cervical Lymph Node Metastases in Papillary Thyroid Cancer
- Pattern of Cervical Neck Lymph Node Metastasis in Papillary Thyroid Carcinoma according to Tumor Size
- Retropharyngeal Lymph Node Metastasis of Thyroid Papillary Carcinoma