HDL Subclass Analysis in Predicting Metabolic Syndrome in Koreans With High HDL Cholesterol Levels
- Affiliations
-
- 1Department of Cardiovascular Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 2Department of Laboratory Medicine, Konkuk University School of Medicine, Seoul, Korea. dearmina@hanmail.net
- 3Department of Respiratory Medicine, Konkuk University School of Medicine, Seoul, Korea.
- 4Research Coordinating Center, Konkuk University Medical Center, Seoul, Korea.
- 5Department of Medical-Surgery Sciences and Translational Medicine, University La Sapienza Rome, Sant'Andrea Hospital, Rome, Italy.
- KMID: 2470325
- DOI: http://doi.org/10.3343/alm.2020.40.4.297
Abstract
- BACKGROUND
High-density lipoprotein cholesterol (HDL-C) is a complex mixture of subclasses with heterogeneous atheroprotective activities. We analyzed HDL-C subclass in relation to cardiovascular risk and metabolic syndrome (MetS) in a population with high HDL-C levels.
METHODS
A total of 300 Korean individuals with high HDL-C levels (≥2.331 mmol/L) were enrolled following a comprehensive general medical examination including body composition analysis. HDL3-C levels were measured using the HDL3-EX SEIKEN kit (Randox Ltd., Crumlin, UK) and non-HDL3-C levels were calculated by subtracting HDL3-C levels from total HDL-C levels.
RESULTS
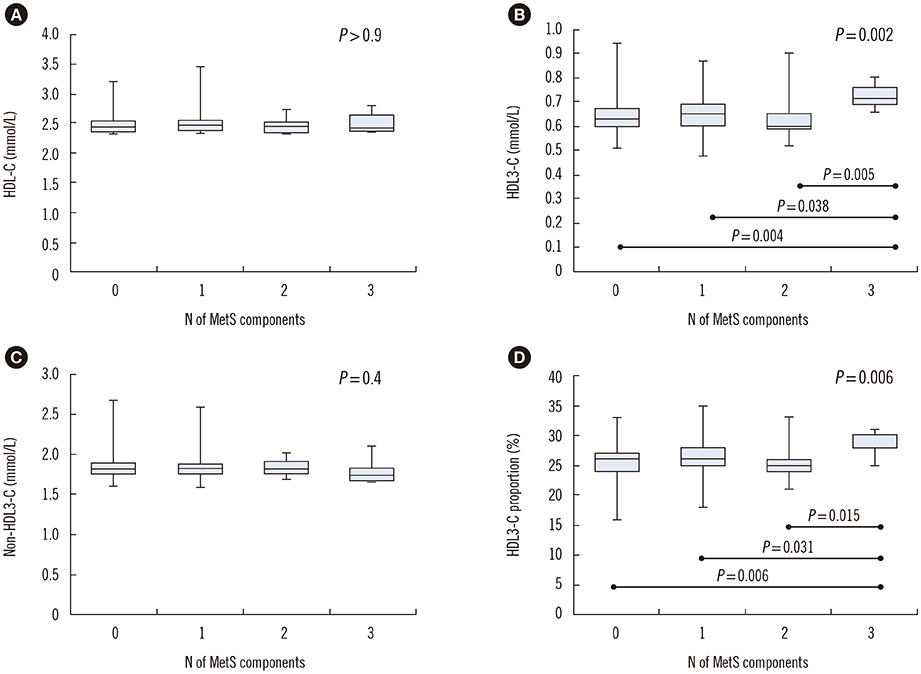
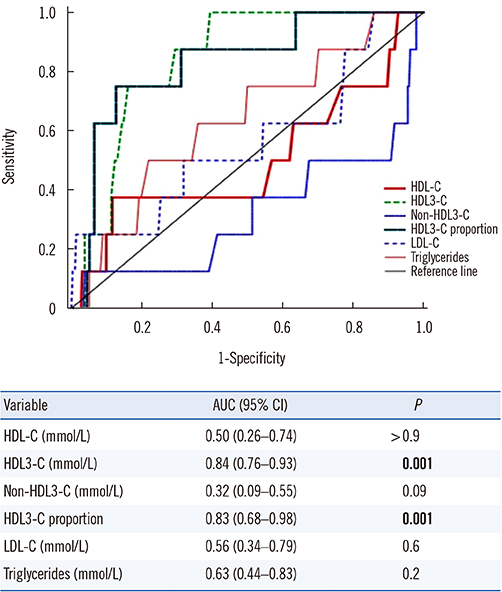
HDL3-C levels and HDL3-C proportion had a weak positive correlation with low-density lipoprotein cholesterol (LDL-C) and triglycerides (r=0.21, r=0.25; r=0.26, r=0.34, respectively, all P<0.001); in contrast, non-HDL3-C levels had a weak negative correlation with these parameters (r=−0.17 and r=−0.25, respectively, both P<0.005). HDL3-C levels and HDL3-C proportion were significantly higher in the MetS group (N=8) than in the non-MetS group (0.71 vs 0.63 mmol/L, P=0.001; 29.7 vs 25.8%, P=0.001, respectively); these were the only predictors of MetS among the lipid variables (areas under the curves [AUC]=0.84 and 0.83, respectively, both P=0.001).
CONCLUSIONS
In populations with high HDL-C levels, HDL-C subclass may provide a greater amount of information on cardiovascular risk and MetS than HDL-C levels alone.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Sex-Specific U-Shaped Relationships Between High-Density Lipoprotein Cholesterol Levels and 10-year Major Adverse Cardiovascular Events: A Nationwide Cohort Study of 5.7 Million South Koreans
Hyun Suk Yang, Ho Jin Jeong, Hyeongsu Kim, Hweung Kon Hwang, Mina Hur, Seungho Lee
Ann Lab Med. 2022;42(4):415-427. doi: 10.3343/alm.2022.42.4.415.Intuitive Modification of the Friedewald Formula for Calculation of LDL-Cholesterol
Jinyoung Hong, Hyunjung Gu, Juhee Lee, Woochang Lee, Sail Chun, Ki Hoon Han, Won-Ki Min
Ann Lab Med. 2023;43(1):29-37. doi: 10.3343/alm.2023.43.1.29.Apolipoprotein B, Non-HDL Cholesterol, and LDL Cholesterol as Markers for Atherosclerotic Cardiovascular Disease Risk Assessment
Yeo-Min Yun
Ann Lab Med. 2023;43(3):221-222. doi: 10.3343/alm.2023.43.3.221.
Reference
-
1. Wilson PW, Abbott RD, Castelli WP. High density lipoprotein cholesterol and mortality. The Framingham Heart Study. Arteriosclerosis. 1988; 8:737–741.
Article2. Gordon DJ, Rifkind BM. High-density lipoprotein–the clinical implications of recent studies. N Engl J Med. 1989; 321:1311–1316.3. Voight BF, Peloso GM, Orho-Melander M, Frikke-Schmidt R, Barbalic M, Jensen MK, et al. Plasma HDL cholesterol and risk of myocardial infarction: a Mendelian randomisation study. Lancet. 2012; 380:572–580.4. AIM-HIGH Investigators. Boden WE, Probstfield JL, Anderson T, Chaitman BR, Desvignes-Nickens P, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011; 365:2255–2267.
Article5. Madsen CM, Varbo A, Nordestgaard BG. Extreme high-density lipoprotein cholesterol is paradoxically associated with high mortality in men and women: two prospective cohort studies. Eur Heart J. 2017; 38:2478–2486.6. Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016; 37:2999–3058.
Article7. Mortensen MB, Afzal S, Nordestgaard BG, Falk E. The high-density lipoprotein-adjusted SCORE model worsens SCORE-based risk classification in a contemporary population of 30,824 Europeans: the Copenhagen General Population Study. Eur Heart J. 2015; 36:2446–2453.8. Vallejo-Vaz AJ, Ray KK. Cholesterol efflux capacity as a novel biomarker for incident cardiovascular events: has high-density lipoprotein been resuscitated? Circ Res. 2015; 116:1646–1648.9. Wallentin L, Fåhraeus L. HDL3 and HDL2 determination by a combined ultracentrifugation and precipitation procedure. Clin Chim Acta. 1981; 116:199–208.
Article10. Mueller O, Chang E, Deng D, Franz T, Jing D, Kincaid R, et al. PROCAM Study: risk prediction for myocardial infarction using microfluidic high-density lipoprotein (HDL) subfractionation is independent of HDL cholesterol. Clin Chem Lab Med. 2008; 46:490–498.
Article11. Ashmaig ME, Gupta S, McConnell JP, Warnick GR. Validation of a novel homogeneous assay for of HDL3-C measurement. Clin Chim Acta. 2013; 425:37–41.
Article12. Gómez F, Camps J, Simó JM, Ferré N, Joven J. Agreement study of methods based on the elimination principle for the measurement of LDL- and HDL-cholesterol compared with ultracentrifugation in patients with liver cirrhosis. Clin Chem. 2000; 46:1188–1191.13. Rosenson RS, Brewer HB Jr, Chapman MJ, Fazio S, Hussain MM, Kontush A, et al. HDL measures, particle heterogeneity, proposed nomenclature, and relation to atherosclerotic cardiovascular events. Clin Chem. 2011; 57:392–410.
Article14. Camont L, Chapman MJ, Kontush A. Biological activities of HDL subpopulations and their relevance to cardiovascular disease. Trends Mol Med. 2011; 17:594–603.
Article15. Joshi PH, Toth PP, Lirette ST, Griswold ME, Massaro JM, Martin SS, et al. Association of high-density lipoprotein subclasses and incident coronary heart disease: The Jackson Heart and Framingham Offspring Cohort Studies. Eur J Prev Cardiol. 2016; 23:41–49.
Article16. Yu S, Yarnell JW, Sweetnam P, Bolton CH. High density lipoprotein subfractions and the risk of coronary heart disease: 9-years follow-up in the Caerphilly Study. Atherosclerosis. 2003; 166:331–338.
Article17. Albers JJ, Slee A, Fleg JL, O'Brien KD, Marcovina SM. Relationship of baseline HDL subclasses, small dense LDL and LDL triglyceride to cardiovascular events in the AIM-HIGH clinical trial. Atherosclerosis. 2016; 251:454–459.
Article18. Martin SS, Khokhar AA, May HT, Kulkarni KR, Blaha MJ, Joshi PH, et al. HDL cholesterol subclasses, myocardial infarction, and mortality in secondary prevention: the Lipoprotein Investigators Collaborative. Eur Heart J. 2015; 36:22–30.
Article19. Williams PT, Feldman DE. Prospective study of coronary heart disease vs. HDL2, HDL3, and other lipoproteins in Gofman's Livermore Cohort. Atherosclerosis. 2011; 214:196–202.
Article20. Lamarche B, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Després JP. Associations of HDL2 and HDL3 subfractions with ischemic heart disease in men. Prospective results from the Quebec Cardiovascular Study. Arterioscler Thromb Vasc Biol. 1997; 17:1098–1105.21. Salonen JT, Salonen R, Seppänen K, Rauramaa R, Tuomilehto J. HDL, HDL2, and HDL3 subfractions, and the risk of acute myocardial infarction. A prospective population study in eastern Finnish men. Circulation. 1991; 84:129–139.
Article22. Superko HR, Pendyala L, Williams PT, Momary KM, King SB 3rd, Garrett BC. High-density lipoprotein subclasses and their relationship to cardiovascular disease. J Clin Lipidol. 2012; 6:496–523.
Article23. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA. 2001; 285:2486–2497.24. Tan CE, Ma S, Wai D, Chew SK, Tai ES. Can we apply the National Cholesterol Education Program Adult Treatment Panel definition of the metabolic syndrome to Asians? Diabetes Care. 2004; 27:1182–1186.
Article25. Lee M, Jang Y, Kim K, Cho H, Jee SH, Park Y, et al. Relationship between HDL3 subclasses and waist circumferences on the prevalence of metabolic syndrome: KMSRI-Seoul Study. Atherosclerosis. 2010; 213:288–293.
Article26. Moriyama K, Negami M, Takahashi E. HDL2-cholesterol/HDL3-cholesterol ratio was associated with insulin resistance, high-molecular-weight adiponectin, and components for metabolic syndrome in Japanese. Diabetes Res Clin Pract. 2014; 106:360–365.
Article27. Tabara Y, Arai H, Hirao Y, Takahashi Y, Setoh K, Kawaguchi T, et al. Different inverse association of large high-density lipoprotein subclasses with exacerbation of insulin resistance and incidence of type 2 diabetes: The Nagahama study. Diabetes Res Clin Pract. 2017; 127:123–131.
Article28. Generoso G, Bensenor IM, Santos RD, Santos IS, Goulart AC, Jones SR, et al. Association between high-density lipoprotein subfractions and low-grade inflammation, insulin resistance, and metabolic syndrome components: The ELSA-Brasil study. J Clin Lipidol. 2018; 12:1290–1297.e1.
Article29. McLester CN, Nickerson BS, Kliszczewicz BM, McLester JR. Reliability and agreement of various InBody body composition analyzers as compared to dual-energy X-ray absorptiometry in healthy men and women. J Clin Densitom. 2018; 11. 03. DOI: 10.1016/j.jocd.2018.10.008. [Epub ahead of print].
Article30. Schober P, Boer C, Schwarte LA. Correlation coefficients: appropriate use and interpretation. Anesth Analg. 2018; 126:1763–1768.31. Patrick ME. High-intensity drinking. Alcohol Res. 2018; 39:49–55.32. Anagnostis P, Stevenson JC, Crook D, Johnston DG, Godsland IF. Effects of menopause, gender and age on lipids and high-density lipoprotein cholesterol subfractions. Maturitas. 2015; 81:62–68.
Article33. Tian L, Li C, Liu Y, Chen Y, Fu M. The value and distribution of high-density lipoprotein subclass in patients with acute coronary syndrome. PLoS One. 2014; 9:e85114.
Article34. Yang D, Cai Q, Qi X, Zhou Y. Postprandial lipid concentrations and daytime biological variation of lipids in a healthy Chinese population. Ann Lab Med. 2018; 38:431–439.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Relationship between Metabolic Syndrome and Triglyceride/High-density Lipoprotein Cholesterol Ratio
- Association between High-Density Lipoprotein Cholesterol and Vitamin D Levels in Adult Men in the Fifth Korea National Health and Nutrition Examination Survey
- Obesity and High-density lipoprotein Cholesterol (HDL-C) : The Recent Related Research Trend Including New Generation Drugs for HDL-C
- A Study on Changes of Serum HDL-Cholesterol Level in Some Diseases
- Lipid Profiles in Hypertension and Cerebrovascular Diseases