Korean J Ophthalmol.
2020 Feb;34(1):35-45. 10.3341/kjo.2019.0086.
Effect of Donor Age on Graft Survival in Primary Penetrating Keratoplasty with Imported Donor Corneas
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. jeonhs@snu.ac.kr
- 2Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 2469285
- DOI: http://doi.org/10.3341/kjo.2019.0086
Abstract
- PURPOSE
To investigate the influence of donor age on corneal graft survival following primary penetrating keratoplasty (PK) with imported donor corneas.
METHODS
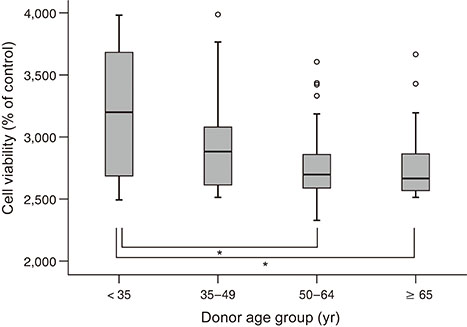
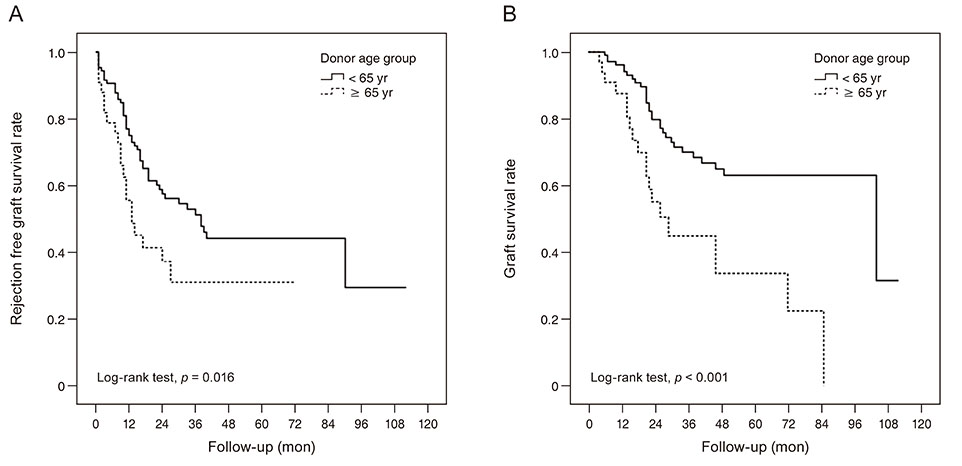
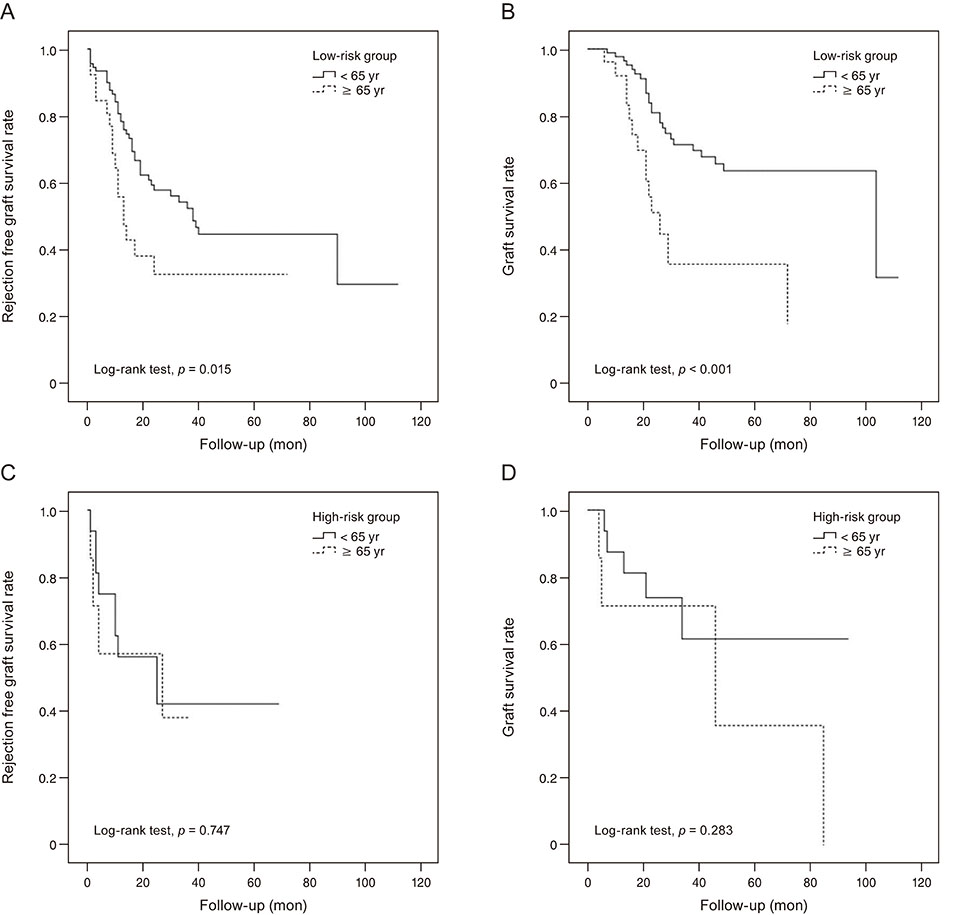
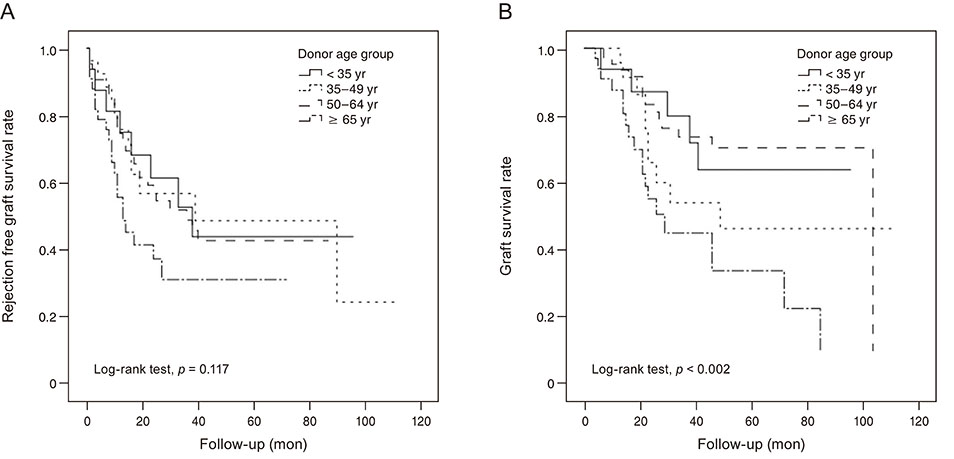
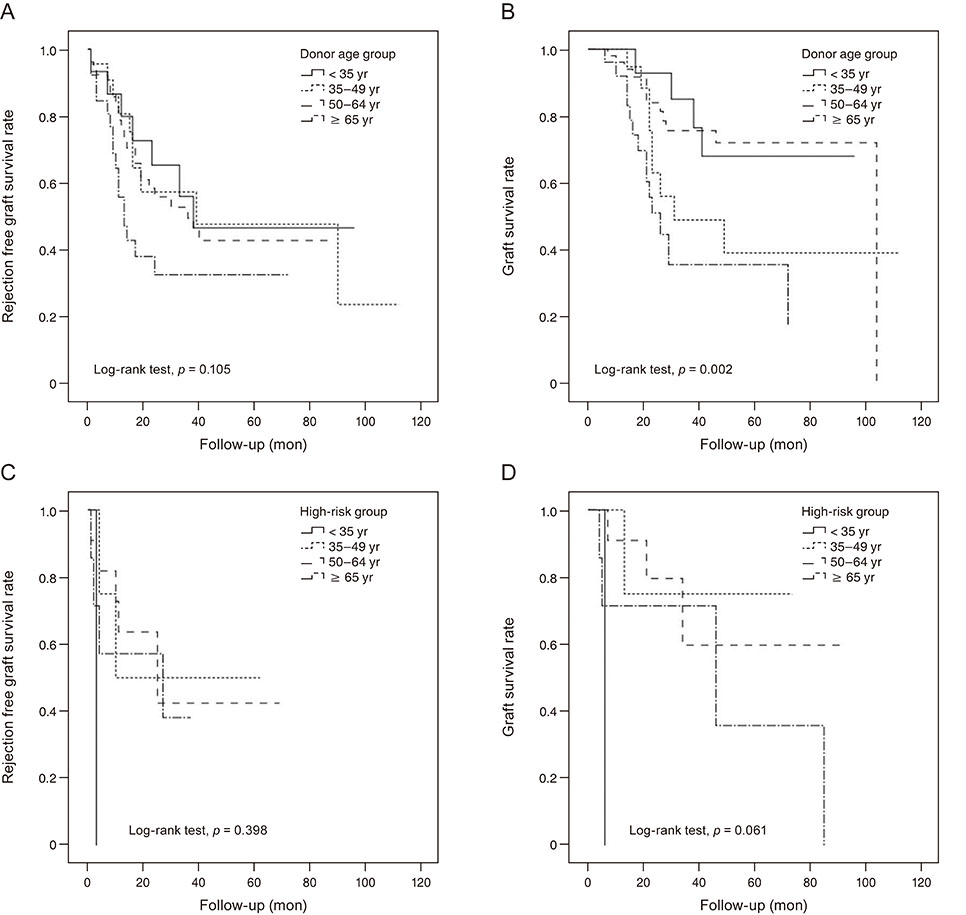
The eyes of patients who underwent primary PK with imported donor corneas were classified retrospectively into two groups according to a donor-age cutoff of 65 years. Primary outcome measures were rejection-free graft survival and graft survival. Cox proportional hazard regression analysis was used to assess the factors affecting graft survival. Survival analysis was performed using the Kaplan-Meier method, while differences between groups were examined using a log-rank test. A subgroup analysis of low- and high-risk eyes according to preoperative diagnosis was also performed.
RESULTS
A total of 140 eyes from 138 patients (age, 58 ± 18 years) were enrolled. Cox regression analysis revealed that the donor age of 65 years or older group presented an increased risk of both graft rejection and failure. Survival analysis revealed that rejection-free graft survival and graft survival rates were higher in eyes in the donor age of less than 65 years group. Finally, in the subgroup analysis, both rejection-free graft survival and graft survival rates were significantly higher in the donor age of less than 65 years group than in the donor age of 65 years or older group, but only in the low-risk subgroup.
CONCLUSIONS
Donor age may correlate with graft survival in primary PK performed with imported donor corneas. Donor age could be a considerable factor in primary PK with imported donor corneas, especially in preoperatively low-risk patients.
MeSH Terms
Figure
Reference
-
1. Williams KA, Roder D, Esterman A, et al. Factors predictive of corneal graft survival. Report from the Australian Corneal Graft Registry. Ophthalmology. 1992; 99:403–414.2. Kim MK, Lee JH. Long-term outcome of graft rejection after penetrating keratoplasty. J Korean Ophthalmol Soc. 1997; 38:1553–1560.3. Krohn J, Hovding G. The influence of donor age and cause of death on corneal endothelial cell density. Acta Ophthalmol Scand. 2005; 83:746–750.
Article4. Kwon JW, Cho KJ, Kim HK, et al. Analyses of factors affecting endothelial cell density in an eye bank corneal donor database. Cornea. 2016; 35:1206–1210.
Article5. Wagoner MD, Gonnah el-S, Al-Towerki AE. King Khaled Eye Specialist Hospital Cornea Transplant Study Group. Outcome of primary adult optical penetrating keratoplasty with imported donor corneas. Int Ophthalmol. 2010; 30:127–136.
Article6. Armitage WJ, Jones MN, Zambrano I, et al. The suitability of corneas stored by organ culture for penetrating keratoplasty and influence of donor and recipient factors on 5-year graft survival. Invest Ophthalmol Vis Sci. 2014; 55:784–791.
Article7. Sugar A, Gal RL, Beck W, et al. Baseline donor characteristics in the Cornea Donor Study. Cornea. 2005; 24:389–396.8. Beck RW, Gal RL, Mannis MJ, et al. Is donor age an important determinant of graft survival? Cornea. 1999; 18:503–510.
Article9. Cornea Donor Study Investigator Group. Gal RL, Dontchev M, et al. The effect of donor age on corneal transplantation outcome results of the cornea donor study. Ophthalmology. 2008; 115:620–626.10. Cornea Donor Study Investigator Group. Lass JH, Gal RL, et al. Donor age and corneal endothelial cell loss 5 years after successful corneal transplantation. Specular microscopy ancillary study results. Ophthalmology. 2008; 115:627–632.11. Writing Committee for the Cornea Donor Study Research Group. Mannis MJ, Holland EJ, et al. The effect of donor age on penetrating keratoplasty for endothelial disease: graft survival after 10 years in the Cornea Donor Study. Ophthalmology. 2013; 120:2419–2427.12. Writing Committee for the Cornea Donor Study Research Group. Lass JH, Benetz BA, et al. Donor age and factors related to endothelial cell loss 10 years after penetrating keratoplasty: Specular Microscopy Ancillary Study. Ophthalmology. 2013; 120:2428–2435.13. Park SH, Kim JH, Joo CK. The clinical evaluations of the penetrating keratoplasty with imported donor corneas. J Korean Ophthalmol Soc. 2005; 46:28–34.14. Kong SJ, Cho K, Kim MS. Analysis of factors affecting the decrease of endothelial cell density in imported donor corneas. J Korean Ophthalmol Soc. 2012; 53:20–26.
Article15. Kim DH, Lee JY, Oh JY, et al. Comparative analysis of clinical outcome in penetrating keratoplasty using domestic or imported cornea. J Korean Ophthalmol Soc. 2015; 56:672–679.
Article16. Kim MJ, Kim JH, Jeon HS, et al. Effect of histocompatibility Y antigen matching on graft survival in primary penetrating keratoplasty. Cornea. 2018; 37:33–38.
Article17. Shimazaki J, Iseda A, Satake Y, Shimazaki-Den S. Efficacy and safety of long-term corticosteroid eye drops after penetrating keratoplasty: a prospective, randomized, clinical trial. Ophthalmology. 2012; 119:668–673.18. Bohringer D, Reinhard T, Spelsberg H, Sundmacher R. Influencing factors on chronic endothelial cell loss characterised in a homogeneous group of patients. Br J Ophthalmol. 2002; 86:35–38.
Article19. Palay DA, Kangas TA, Stulting RD, et al. The effects of donor age on the outcome of penetrating keratoplasty in adults. Ophthalmology. 1997; 104:1576–1579.
Article20. Shimazaki J, Shinozaki N, Shimmura S, et al. Efficacy and safety of international donor sharing: a single-center, case-controlled study on corneal transplantation. Transplantation. 2004; 78:216–220.
Article21. Cho EY, Kim MS. Penetrating keratoplasty before and after establishment of Korean Network for Organ Sharing. J Korean Ophthalmol Soc. 2006; 47:525–530.22. Lee JS, Park YG, Yoon KC. Long-term results of Descemet’s stripping automated endothelial keratoplasty in Korea. J Korean Ophthalmol Soc. 2010; 51:1431–1437.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Clinical Evaluations of the Penetrating Keratoplasty with Imported Donor Corneas
- Influence of Endothelial Cell Loss During Preservation on Graft Survival in Imported Donor Cornea
- Penetrating Keratoplasty before and after Establishment of Korean Network for Organ Sharing
- Analysis of Factors Affecting the Decrease of Endothelial Cell Density in Imported Donor Corneas
- Comparative Analysis of Clinical Outcome in Penetrating Keratoplasty Using Domestic or Imported Cornea