J Korean Soc Radiol.
2020 Jan;81(1):190-196. 10.3348/jksr.2020.81.1.190.
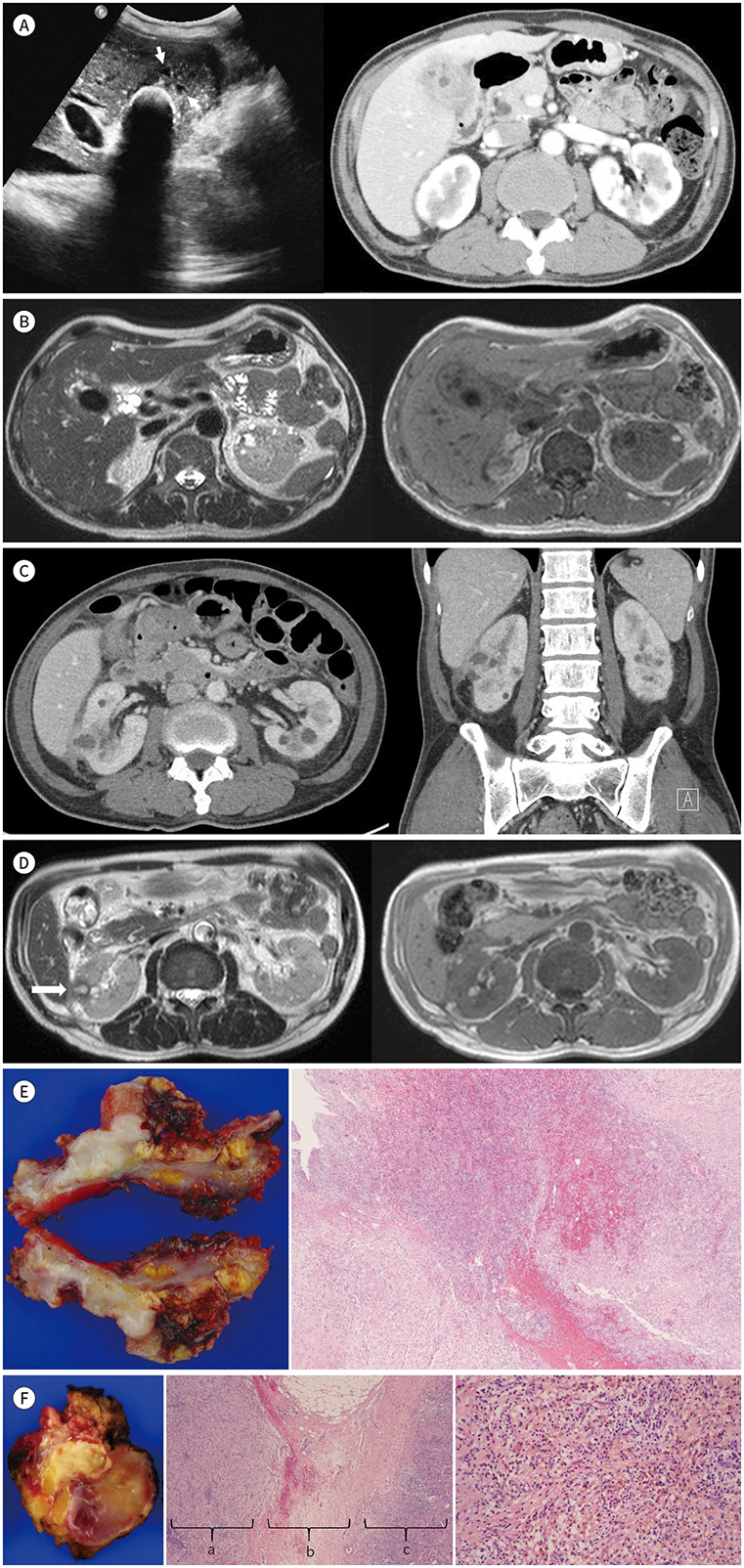
Focal Xanthogranulomatous Pyelonephritis Associated with Xanthogranulomatous Cholecystitis: A Case Report
- Affiliations
-
- 1Department of Radiology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea. kyhkim@hanmail.net
- 2Department of Pathology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- 3Department of General Surgery, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea.
- KMID: 2469192
- DOI: http://doi.org/10.3348/jksr.2020.81.1.190
Abstract
- Xanthogranulomatous inflammation is a rare inflammatory reaction, characterized by lipid-laden macrophages, known as xanthomas, in histopathologic examination. Aggressive xanthogranulomatous inflammation often manifests as local infiltration but does not affect distant organs unless combined with rare systemic diseases. We report a case of focal xanthogranulomatous pyelonephritis (XGP) associated with severe xanthogranulomatous cholecystitis. Focal XGP was suspected in radiologic examination that showed a cystic lesion with an infiltrative margin, which were surgically resected and confirmed in pathologic examination. To our knowledge, this is the first report of focal xanthogranulomatous pyelonephritis associated with xanthogranulomatous cholecystitis. Moreover, we found peripheral hypointensity around the cystic lesion in the T2-weighted image, probably reflecting hemorrhage and fibrosis of the xanthogranulomatous inflammation.
MeSH Terms
Figure
Reference
-
1. Bourm KS, Menias CO, Ali K, Alhalabi K, Elsayes KM. Spectrum of xanthogranulomatous processes in the abdomen and pelvis: a pictorial review of infectious, inflammatory, and proliferative responses. AJR Am J Roentgenol. 2017; 208:475–484.
Article2. Kuo CC, Wu CF, Huang CC, Lee YJ, Lin WC, Tsai CW, et al. Xanthogranulomatous pyelonephritis: critical analysis of 30 patients. Int Urol Nephrol. 2011; 43:15–22.
Article3. Kaushik R, Attri AK. Choleretroperitoneum-an unusual complication of cholelithiasis. Indian J Surg. 2004; 66:358–360.4. Roels K, Bogaert J, Van Hoe L, Vanbeckevoort D, Delvaux S. Xanthogranulomatous cholecystitis associated with a xanthogranulomatous pseudotumour on the left diaphragm. Eur Radiol. 1999; 9:1139–1141.
Article5. Losanoff JE, Reichman TW, Steinberg GD, Millis JM. Duodenal diverticulum causing xanthogranulomatous pyelonephritis with multiorgan involvement: first case report. Digestion. 2006; 74:236–237.
Article6. Verswijvel G, Oyen R, Van Poppel H, Roskams T. Xanthogranulomatous pyelonephritis: MRI findings in the diffuse and the focal type. Eur Radiol. 2000; 10:586–589.
Article7. Song YS, Lee IS, Choi KU, Cho KH, Lee SM, Lee YH, et al. Soft tissue masses showing low signal intensity on T2-weighted images: correlation with pathologic findings. J Korean Soc Magn Reson Med. 2014; 18:279–289.
Article8. Cakmakci H, Tasdelen N, Obuz F, Yilmaz E, Kovanlikaya A. Pediatric focal xanthogranulomatous pyelonephritis: dynamic contrast-enhanced MRI findings. Clin Imaging. 2002; 26:183–186.9. Chang BJ, Kim SH, Park HY, Lim SW, Kim J, Lee KH, et al. Distinguishing xanthogranulomatous cholecystitis from the wall-thickening type of early-stage gallbladder cancer. Gut Liver. 2010; 4:518–523.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Xanthogranulomatous Pyelonephritis
- A case of xanthogranulomatous pyelonephritis
- Two Cases of Xanthogranulomatous Pyelonephritis
- Xanthogranulomatous Pyelonephritis: A Case Report and Review of the Literature
- A Case of Xanthogranulomatous Pyelonephritis which was Confused with Renal Pelvic Tumor