J Korean Fract Soc.
2020 Jan;33(1):22-26. 10.12671/jkfs.2020.33.1.22.
Brachial Plexus Neuropathy after Revision of Clavicular Fracture Nonunion: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, The Catholic University of Korea, Uijeongbu St. Mary's Hospital, Uijeongbu, Korea.
- 2Department of Orthopedic Surgery, Inje University Ilsan Paik Hospital, Goyang, Korea.
- 3Department of Orthopedic Surgery, MS Jaegeon Hospital, Daegu, Korea. bless2d@naver.com
- KMID: 2468670
- DOI: http://doi.org/10.12671/jkfs.2020.33.1.22
Abstract
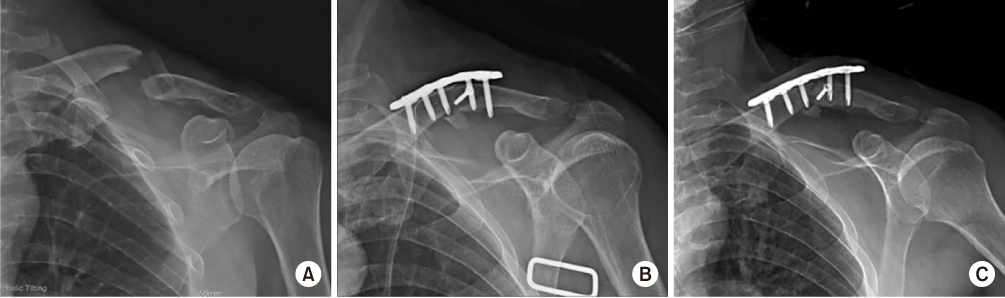
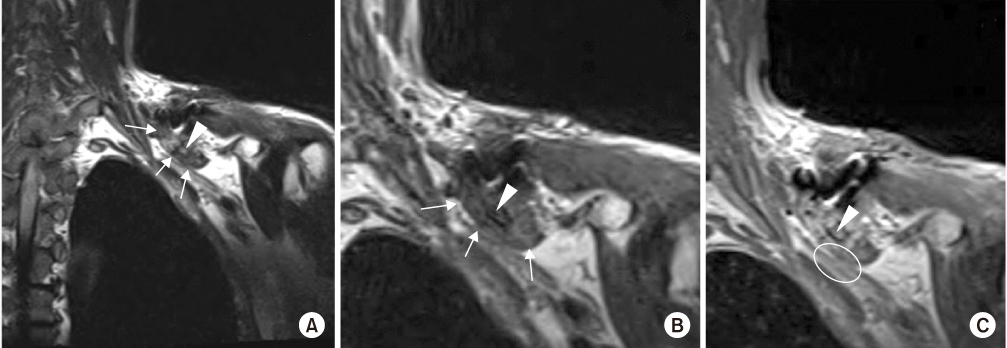
- We performed a revisionary open reduction and internal fixation for treating nonunion of the mid-shaft of the left clavicle with an autogenous cancellous bone graft. On postoperative day 4, the patient presented with neurologic deficits in the left upper extremity. We removed the implant and made a superior angulation to decompress the brachial plexus. At 6 months postoperatively, callus bridging and consolidation were visible and all hand and elbow functions were fully recovered. Our case suggests that brachial plexus neuropathy may be caused by stretching and compression after reduction and straightening of the nonunion site around adhesions or scar tissue. Therefore, care should be taken whether there are the risk factors that can cause brachial plexus neuropathy when revision surgery is performed for treating nonunion of a clavicle shaft fracture.
Keyword
MeSH Terms
Figure
Reference
-
1. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968; 58:29–42.2. Namdari S, Voleti PB, Huffman GR. Compressive brachial plexopathy after fixation of a clavicular fracture nonunion: a case report. JBJS Case Connect. 2012; 2:e26.3. Derham C, Varghese M, Deacon P, Spencer N, Curley P. Brachial plexus palsy secondary to clavicular nonunion. J Trauma. 2007; 63:E105–E107.
Article4. Della Santa D, Narakas A, Bonnard C. Late lesions of the brachial plexus after fracture of the clavicle. Ann Chir Main Memb Super. 1991; 10:531–540.
Article5. Jeyaseelan L, Singh VK, Ghosh S, Sinisi M, Fox M. Iatropathic brachial plexus injury: a complication of delayed fixation of clavicle fractures. Bone Joint J. 2013; 95:106–110.6. Martetschläger F, Gaskill TR, Millett PJ. Management of clavicle nonunion and malunion. J Shoulder Elbow Surg. 2013; 22:862–868.
Article7. Der Tavitian J, Davison JN, Dias JJ. Clavicular fracture non-union surgical outcome and complications. Injury. 2002; 33:135–143.
Article8. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002; 11:452–456.
Article9. Mouzopoulos G, Morakis E, Stamatakos M, Tzurbakis M. Complications associated with clavicular fracture. Orthop Nurs. 2009; 28:217–224. quiz 225-226.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Brachial Plexus Palsy due to Clavicular Fracture: A Case Report
- Brachial Plexus Injury Secondary to Exuberant Callus Formation of Fracture of Clavicle : Two Cases Report
- Progressive Brachial Plexus Palsy after Fixation of Clavicle Shaft Nonunion: A Case Report
- Brachial Plexus Injury of Whole Arm Type Developed after Surgical Treatment of Infectious Mid-Shaft Clavicular Nonunion
- Delayed subclavian - Vein thrombosis Following Nonunion of the Clavicular Fracture: A Case Report