J Korean Ophthalmol Soc.
2020 Jan;61(1):34-40. 10.3341/jkos.2020.61.1.34.
Long-term Outcomes of Vitrectomy Used to Treat Myopic Traction Maculopathy
- Affiliations
-
- 1Department of Ophthalmology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea. sohyun.bae.md@gmail.com
- KMID: 2468474
- DOI: http://doi.org/10.3341/jkos.2020.61.1.34
Abstract
- PURPOSE
We investigated the long-term outcomes of vitrectomy with internal limiting membrane (ILM) peeling as treatment for myopic traction maculopathy (MTM).
METHODS
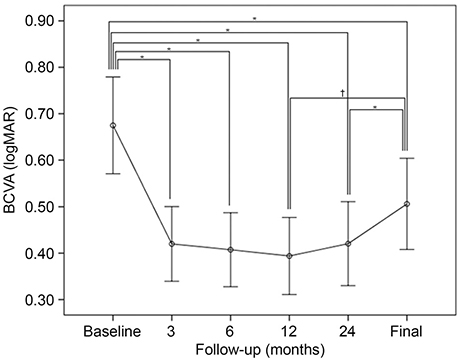
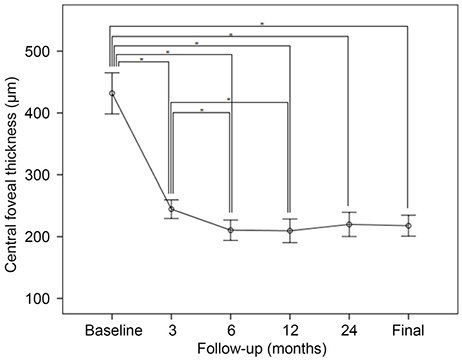
The medical records of patients who underwent vitrectomy to treat MTM were retrospectively evaluated. We excluded patients who exhibited macular holes (MHs) or retinal detachment at the time of primary surgery. The best-corrected visual acuity (BCVA) and central foveal thickness (CFT) were analyzed preoperatively, at 3, 6, 12, and 24 months after surgery, and at the final visit. Complications including retinal detachment or an MH were noted during follow-up.
RESULTS
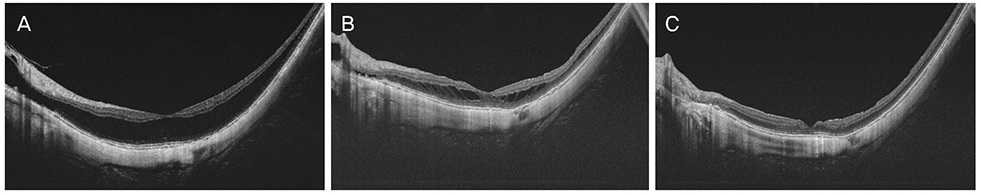
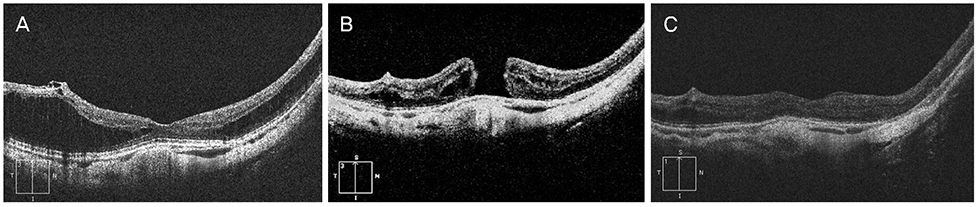
Twenty-three eyes of 22 patients were enrolled. At the time of primary surgery, the mean patient age was 64.4 ± 11.1 years and the baseline mean logMAR BCVA and CFT, 0.67 ± 0.50 and 431.8 ± 159.5 µm, respectively. The mean follow-up period was 53.7 ± 19.3 months. The mean logMAR BCVAs at 3, 6, 12, and 24 months postoperatively and at the final visit were 0.42 ± 0.39 (p = 0.001), 0.41 ± 0.38 (p = 0.001), 0.39 ± 0.40 (p < 0.001), 0.42 ± 0.43 (p < 0.001), and 0.51 ± 0.47 (p = 0.016), respectively, thus significantly better than the baseline value. The mean CFT at 3, 6, 12, and 24 months postoperatively and at the final visit were 244.6 ± 72.3, 210.5 ± 79.1, 209.6 ± 91.6, 219.8 ± 93.9, and 217.7 ± 81.3 µm, respectively, thus significantly less than baseline (all p < 0.001). MTM resolved in 18 eyes (78.3%) after primary surgery, without any complication, and remained stable to the final visit.
CONCLUSIONS
Vitrectomy with ILM peeling afforded favorable long-term efficacy and safety in MTM patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Edwards MH, Lam C. Myopia-historical perspectives and classification. Optician Sutton. 1999; 1:22–26.2. Zejmo M, Formińska-Kapuścik M, Pieczara E, et al. Etiopathogenesis and management of high-degree myopia. Part I. Med Sci Monit. 2009; 15:RA199–RA202.3. Grossniklaus HE, Green WR. Pathologic findings in pathologic myopia. Retina. 1992; 12:127–133.
Article4. Takano M, Kishi S. Foveal retinoschisis and retinal detachment in severely myopic eyes with posterior staphyloma. Am J Ophthalmol. 1999; 128:472–476.
Article5. Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003; 135:338–342.
Article6. Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004; 122:1455–1460.
Article7. Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013; 156:948–957.e1.
Article8. Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007; 143:455–462.
Article9. VanderBeek BL, Johnson MW. The diversity of traction mechanisms in myopic traction maculopathy. Am J Ophthalmol. 2012; 153:93–102.
Article10. Johnson MW. Myopic traction maculopathy: pathogenic mechanisms and surgical treatment. Retina. 2012; 32:Suppl 2. S205–S210.11. Kobayashi H, Kishi S. Vitreous surgery for highly myopic eyes with foveal detachment and retinoschisis. Ophthalmology. 2003; 110:1702–1707.12. Ikuno Y, Sayanagi K, Ohji M, et al. Vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol. 2004; 137:719–724.
Article13. Qi Y, Duan AL, Meng X, Wang N. Vitrectomy without inner limiting membrane peeling for macular retinoschisis in highly myopic eyes. Retina. 2016; 36:953–956.
Article14. Kwok AK, Lai TY, Yip WW. Vitrectomy and gas tamponade without internal limiting membrane peeling for myopic foveoschisis. Br J Ophthalmol. 2005; 89:1180–1183.
Article15. Kumagai K, Furukawa M, Ogino N, Larson E. Factors correlated with postoperative visual acuity after vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Retina. 2010; 30:874–880.
Article16. Taniuchi S, Hirakata A, Itoh Y, et al. Vitrectomy with or without internal limiting membrane peeling for each stage of myopic traction maculopathy. Retina. 2013; 33:2018–2025.
Article17. Shin JY, Yu HG. Visual prognosis and spectral-domain optical coherence tomography findings of myopic foveoschisis surgery using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2012; 32:486–492.
Article18. Gao X, Ikuno Y, Fujimoto S, Nishida K. Risk factors for development of full-thickness macular holes after pars plana vitrectomy for myopic foveoschisis. Am J Ophthalmol. 2013; 155:1021–1027.e1.
Article19. Lehmann M, Devin F, Rothschild PR, et al. Preoperative factors influencing visual recovery after vitrectomy for myopic foveoschisis. Retina. 2019; 39:594–600.
Article20. Rizzo S, Giansanti F, Finocchio L, et al. Vitrectomy with internal limiting membrane peeling and air tamponade for myopic foveoschisis. Retina. 2019; 39:2125–2131.
Article21. Shimada N, Sugamoto Y, Ogawa M, et al. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012; 154:693–701.
Article22. Ho TC, Chen MS, Huang JS, et al. Foveola nonpeeling technique in internal limiting membrane peeling of myopic foveoschisis surgery. Retina. 2012; 32:631–634.
Article23. Figueroa MS, Ruiz-Moreno JM, Gonzalez del, et al. Long-term outcomes of 23-gauge pars plana vitrectomy with internal limiting membrane peeling and gas tamponade for myopic traction maculopathy: a prospective study. Retina. 2015; 35:1836–1843.24. Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007; 125:767–772.
Article25. Ruiz-Medrano J, Montero JA, Flores-Moreno I, et al. Myopic maculopathy: current status and proposal for a new classification and grading system (ATN). Prog Retin Eye Res. 2019; 69:80–115.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Factors Related with Surgical Outcome of Vitrectomy in Myopic Traction Maculopathy
- Acute Stromal Keratitis Following the Vitrectomy for the Treatment of Myopic Tractional Maculopathy in Lupus
- Macular Buckling Surgery Using a Novel L-shaped Buckle for Patients with Myopic Tractional Maculopathy
- A Case of Vitrectomy without Laser for Serous Macular Detachment Associated with Optic Disc Pit
- Clinical Manifestation and Result of Vitrectomy of Vitreomacular Traction Syndrome