Korean J Ophthalmol.
2020 Feb;34(1):67-75. 10.3341/kjo.2019.0115.
Prognostic Factors Related with Surgical Outcome of Vitrectomy in Myopic Traction Maculopathy
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea. jiani4@snu.ac.kr
- KMID: 2469288
- DOI: http://doi.org/10.3341/kjo.2019.0115
Abstract
- PURPOSE
To investigate prognostic factors related to the surgical outcome of vitrectomy in myopic traction maculopathy (MTM).
METHODS
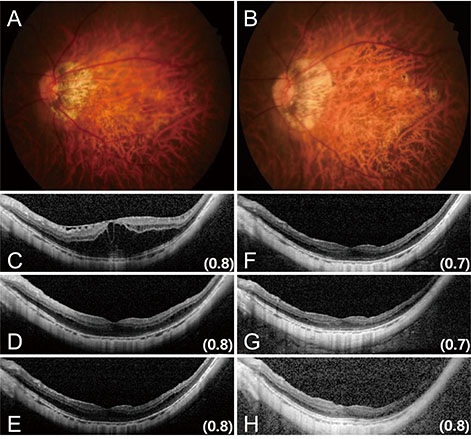
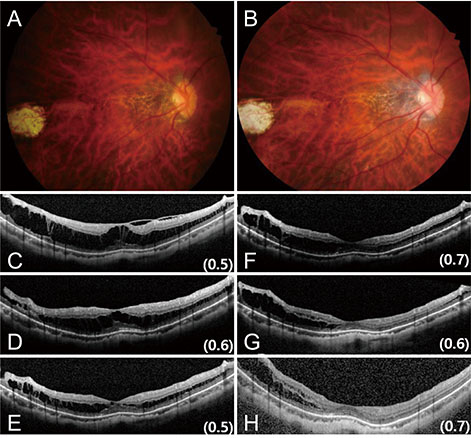
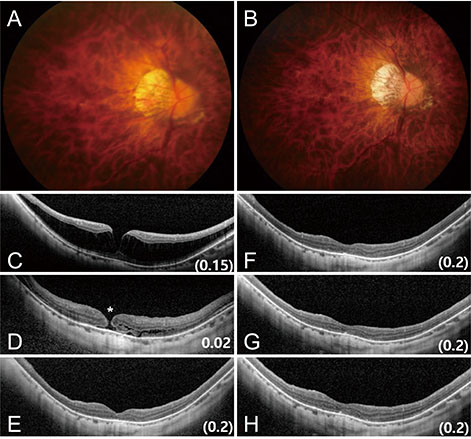
Medical records of patients with MTM who underwent pars plana vitrectomy with internal limiting membrane peeling and follow-up over 12 months were reviewed retrospectively. Best-corrected visual acuity (BCVA), fundoscopic examination and spectral-domain optical coherence tomography findings were evaluated postoperatively. Functional success was defined as visual acuity gain and anatomical success was defined as reduction or resolution of foveoschisis without complications.
RESULTS
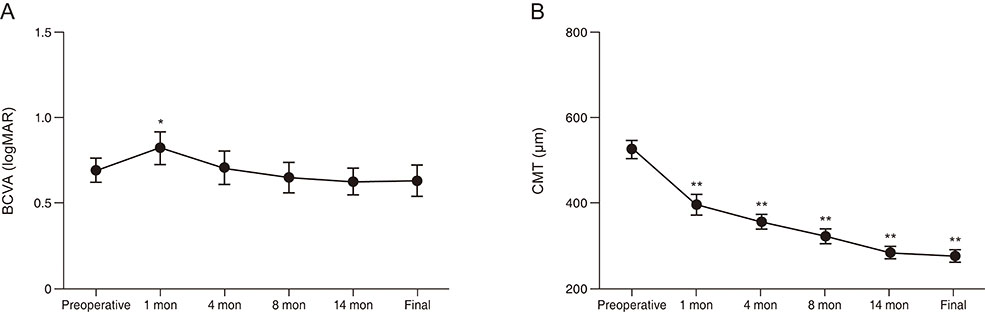
This study included 40 eyes of 36 patients. BCVA improved from 0.70 ± 0.44 to 0.63 ± 0.57 logarithm of minimum angle of resolution and central macular thickness decreased from 526.6 ± 132.1 to 277.8 ± 92.1 µm at final follow-up. Functional success was achieved in 24 (60.0%) eyes, and 33 (82.5%) eyes reached anatomical success. Presence of foveal detachment (FD) and higher category of myopic maculopathy were associated with both functional (p = 0.014, 0.021, respectively) and anatomical (p = 0.011, 0.022, respectively) failure. Longer preoperative axial length showed an association with functional failure but not with anatomical failure (p = 0.041). In multivariate analysis, FD was the only prognostic factor for both functional and anatomical outcome (p = 0.041, 0.043, respectively). Preoperative BCVA (r² = 0.259, p = 0.001), axial length (r² = 0.172, p = 0.008), and myopic maculopathy category (r² = 0.336, p < 0.001) showed significant correlation with final BCVA.
CONCLUSIONS
More severe myopic maculopathy and the presence of FD are associated with poorer functional and anatomical outcomes of pars plana vitrectomy in MTM. Better preoperative BCVA, shorter axial length, and less severe myopic maculopathy are correlated with better final BCVA.
MeSH Terms
Figure
Reference
-
1. Verkicharla PK, Ohno-Matsui K, Saw SM. Current and predicted demographics of high myopia and an update of its associated pathological changes. Ophthalmic Physiol Opt. 2015; 35:465–475.
Article2. Panozzo G, Mercanti A. Optical coherence tomography findings in myopic traction maculopathy. Arch Ophthalmol. 2004; 122:1455–1460.
Article3. Baba T, Ohno-Matsui K, Futagami S, et al. Prevalence and characteristics of foveal retinal detachment without macular hole in high myopia. Am J Ophthalmol. 2003; 135:338–342.
Article4. Johnson MW. Myopic traction maculopathy: pathogenic mechanisms and surgical treatment. Retina. 2012; 32:S205–S210.5. VanderBeek BL, Johnson MW. The diversity of traction mechanisms in myopic traction maculopathy. Am J Ophthalmol. 2012; 153:93–102.
Article6. Ikuno Y, Gomi F, Tano Y. Potent retinal arteriolar traction as a possible cause of myopic foveoschisis. Am J Ophthalmol. 2005; 139:462–467.
Article7. Panozzo G, Mercanti A. Vitrectomy for myopic traction maculopathy. Arch Ophthalmol. 2007; 125:767–772.
Article8. Shimada N, Tanaka Y, Tokoro T, Ohno-Matsui K. Natural course of myopic traction maculopathy and factors associated with progression or resolution. Am J Ophthalmol. 2013; 156:948–957.
Article9. Kobayashi H, Kishi S. Vitreous surgery for highly myopic eyes with foveal detachment and retinoschisis. Ophthalmology. 2003; 110:1702–1707.10. Futagami S, Inoue M, Hirakata A. Removal of internal limiting membrane for recurrent myopic traction maculopathy. Clin Exp Ophthalmol. 2008; 36:782–785.
Article11. Kanda S, Uemura A, Sakamoto Y, Kita H. Vitrectomy with internal limiting membrane peeling for macular retinoschisis and retinal detachment without macular hole in highly myopic eyes. Am J Ophthalmol. 2003; 136:177–180.
Article12. Gaucher D, Haouchine B, Tadayoni R, et al. Long-term follow-up of high myopic foveoschisis: natural course and surgical outcome. Am J Ophthalmol. 2007; 143:455–462.
Article13. Gao X, Ikuno Y, Fujimoto S, Nishida K. Risk factors for development of full-thickness macular holes after pars plana vitrectomy for myopic foveoschisis. Am J Ophthalmol. 2013; 155:1021–1027.
Article14. Kumagai K, Furukawa M, Ogino N, Larson E. Factors correlated with postoperative visual acuity after vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Retina. 2010; 30:874–880.
Article15. Hwang JU, Joe SG, Lee JY, et al. Microincision vitrectomy surgery for myopic foveoschisis. Br J Ophthalmol. 2013; 97:879–884.
Article16. Figueroa MS, Ruiz-Moreno JM, Gonzalez del, et al. Long-term outcomes of 23-gauge pars plana vitrectomy with internal limiting membrane peeling and gas tamponade for myopic traction maculopathy: A Prospective Study. Retina. 2015; 35:1836–1843.17. Shin JY, Yu HG. Visual prognosis and spectral-domain optical coherence tomography findings of myopic foveoschisis surgery using 25-gauge transconjunctival sutureless vitrectomy. Retina. 2012; 32:486–492.
Article18. Sayanagi K, Ikuno Y, Soga K, Tano Y. Photoreceptor inner and outer segment defects in myopic foveoschisis. Am J Ophthalmol. 2008; 145:902–908.
Article19. Hattori K, Kataoka K, Takeuchi J, et al. Predictive factors of surgical outcomes in vitrectomy for myopic traction maculopathy. Retina. 2018; 38:S23–S30.
Article20. Ohno-Matsui K, Kawasaki R, Jonas JB, et al. International photographic classification and grading system for myopic maculopathy. Am J Ophthalmol. 2015; 159:877–883.
Article21. Taniuchi S, Hirakata A, Itoh Y, et al. Vitrectomy with or without internal limiting membrane peeling for each stage of myopic traction maculopathy. Retina. 2013; 33:2018–2025.
Article22. Ikuno Y, Sayanagi K, Ohji M, et al. Vitrectomy and internal limiting membrane peeling for myopic foveoschisis. Am J Ophthalmol. 2004; 137:719–724.
Article23. Shimada N, Sugamoto Y, Ogawa M, et al. Fovea-sparing internal limiting membrane peeling for myopic traction maculopathy. Am J Ophthalmol. 2012; 154:693–701.
Article24. Ho TC, Yang CM, Huang JS, et al. Long-term outcome of foveolar internal limiting membrane nonpeeling for myopic traction maculopathy. Retina. 2014; 34:1833–1840.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of Vitrectomy for Complication of Proliferative Diabetic Retinopathy
- Acute Stromal Keratitis Following the Vitrectomy for the Treatment of Myopic Tractional Maculopathy in Lupus
- Macular Buckling Surgery Using a Novel L-shaped Buckle for Patients with Myopic Tractional Maculopathy
- Causes of Decreased Visual Acuity after Diabetic Vitrectomy
- Clinical Manifestation and Result of Vitrectomy of Vitreomacular Traction Syndrome