J Korean Med Sci.
2016 Oct;31(10):1617-1623. 10.3346/jkms.2016.31.10.1617.
Age, Predisposing Diseases, and Ultrasonographic Findings in Determining Clinical Outcome of Acute Acalculous Inflammatory Gallbladder Diseases in Children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea. hrlamb@hanmail.net
- 2Department of Pediatrics, Chung-Ang University Hospital, Seoul, Korea.
- 3Department of Radiology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 4Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2468253
- DOI: http://doi.org/10.3346/jkms.2016.31.10.1617
Abstract
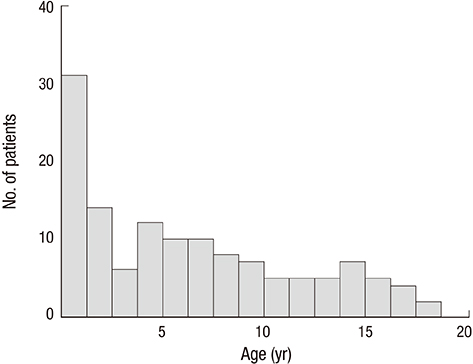
- We evaluated clinical factors such as age, gender, predisposing diseases and ultrasonographic findings that determine clinical outcome of acute acalculous inflammatory gallbladder diseases in children. The patients were divided into the four age groups. From March 2004 through February 2014, clinical data from 131 children diagnosed as acute acalculous inflammatory gallbladder disease by ultrasonography were retrospectively reviewed. Systemic infectious diseases were the most common etiology of acute inflammatory gallbladder disease in children and were identified in 50 patients (38.2%). Kawasaki disease was the most common predisposing disease (28 patients, 21.4%). The incidence was highest in infancy and lowest in adolescence. The age groups were associated with different predisposing diseases; noninfectious systemic disease was the most common etiology in infancy and early childhood, whereas systemic infectious disease was the most common in middle childhood and adolescence (P = 0.001). Gallbladder wall thickening was more commonly found in malignancy (100%) and systemic infection (94.0%) (P = 0.002), whereas gallbladder distension was more frequent in noninfectious systemic diseases (60%) (P = 0.000). Ascites seen on ultrasonography was associated with a worse clinical course compared with no ascites (77.9% vs. 37.7%, P = 0.030), and the duration of hospitalization was longer in patients with ascites (11.6 ± 10.7 vs. 8.0 ± 6.6 days, P = 0.020). In conclusion, consideration of age and predisposing disease in addition to ultrasonographic gallbladder findings in children suspected of acute acalculous inflammatory gallbladder disease might result in better outcomes.
MeSH Terms
-
Abdomen/*diagnostic imaging
Acute Disease
Adolescent
Age Factors
Ascites/etiology
Child
Child, Preschool
Female
Gallbladder/*physiopathology
Gallbladder Diseases/*diagnosis/epidemiology
Hospitalization
Humans
Incidence
Length of Stay
Male
Mucocutaneous Lymph Node Syndrome/diagnosis/pathology
Retrospective Studies
Sex Factors
Ultrasonography
Figure
Cited by 1 articles
-
Prolonged Gallbladder Hydrops in a Kawasaki Disease Patient
Kyung Lim Yoon, Do Hee Kim, Mi Young Han, Sung Ho Cha, Hyun Cheol Kim
Adv Pediatr Surg. 2018;24(2):107-112. doi: 10.13029/aps.2018.24.2.107.
Reference
-
1. Huang SC, Yang YJ. Septic shock and hypofibrinogenemia predict a fatal outcome in childhood acute acalculous cholecystitis. J Pediatr Gastroenterol Nutr. 2011; 53:548–552.2. Kalliafas S, Ziegler DW, Flancbaum L, Choban PS. Acute acalculous cholecystitis: incidence, risk factors, diagnosis, and outcome. Am Surg. 1998; 64:471–475.3. Barie PS, Eachempati SR. Acute acalculous cholecystitis. Gastroenterol Clin North Am. 2010; 39:343–357.4. Sievert W, Vakil NB. Emergencies of the biliary tract. Gastroenterol Clin North Am. 1988; 17:245–264.5. Tsakayannis DE, Kozakewich HP, Lillehei CW. Acalculous cholecystitis in children. J Pediatr Surg. 1996; 31:127–130.6. Flancbaum L, Choban PS. Use of morphine cholescintigraphy in the diagnosis of acute cholecystitis in critically ill patients. Intensive Care Med. 1995; 21:120–124.7. Huffman JL, Schenker S. Acute acalculous cholecystitis: a review. Clin Gastroenterol Hepatol. 2010; 8:15–22.8. Imamoğlu M, Sarihan H, Sari A, Ahmetoğlu A. Acute acalculous cholecystitis in children: diagnosis and treatment. J Pediatr Surg. 2002; 37:36–39.9. Yasuda H, Takada T, Kawarada Y, Nimura Y, Hirata K, Kimura Y, Wada K, Miura F, Hirota M, Mayumi T, et al. Unusual cases of acute cholecystitis and cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007; 14:98–113.10. Wang AJ, Wang TE, Lin CC, Lin SC, Shih SC. Clinical predictors of severe gallbladder complications in acute acalculous cholecystitis. World J Gastroenterol. 2003; 9:2821–2823.11. Higuchi R, Takada T, Strasberg SM, Pitt HA, Gouma DJ, Garden OJ, Büchler MW, Windsor JA, Mayumi T, Yoshida M, et al. TG13 miscellaneous etiology of cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci. 2013; 20:97–105.12. Yi DY, Kim JY, Choi EY, Choi JY, Yang HR. Hepatobiliary risk factors for clinical outcome of Kawasaki disease in children. BMC Pediatr. 2014; 14:51.13. Gora-Gebka M, Liberek A, Bako W, Szarszewski A, Kamińska B, Korzon M. Acute acalculous cholecystitis of viral etiology--a rare condition in children? J Pediatr Surg. 2008; 43:e25–7.14. Arya SO, Saini A, El-Baba M, Salimnia H, Abdel-Haq N. Epstein Barr virus-associated acute acalculous cholecystitis: a rare occurrence but favorable outcome. Clin Pediatr (Phila). 2010; 49:799–804.15. Kim A, Yang HR, Moon JS, Chang JY, Ko JS. Epstein-barr virus infection with acute acalculous cholecystitis. Pediatr Gastroenterol Hepatol Nutr. 2014; 17:57–60.16. Shin YH, Shin JI, Park JM, Kim JH, Lee JS, Kim MJ. A five-year-old boy with nephrotic syndrome complicated with acute acalculous cholecystitis. Pediatr Int. 2007; 49:674–676.17. Williams K, Thomson D, Seto I, Contopoulos-Ioannidis DG, Ioannidis JP, Curtis S, Constantin E, Batmanabane G, Hartling L, Klassen T. Standard 6: age groups for pediatric trials. Pediatrics. 2012; 129:Suppl 3. S153–60.18. Iaria C, Arena L, Di Maio G, Fracassi MG, Leonardi MS, Famulari C, Cascio A. Acute acalculous cholecystitis during the course of primary Epstein-Barr virus infection: a new case and a review of the literature. Int J Infect Dis. 2008; 12:391–395.19. Karkera PJ, Sandlas G, Ranjan R, Gupta A, Kothari P. Acute acalculous cholecystitis causing gall bladder perforation in children. J Indian Assoc Pediatr Surg. 2010; 15:139–141.20. Derici H, Kara C, Bozdag AD, Nazli O, Tansug T, Akca E. Diagnosis and treatment of gallbladder perforation. World J Gastroenterol. 2006; 12:7832–7836.21. Kuo HC, Yang KD, Chang WC, Ger LP, Hsieh KS. Kawasaki disease: an update on diagnosis and treatment. Pediatr Neonatol. 2012; 53:4–11.22. Babb RR. Acute acalculous cholecystitis. A review. J Clin Gastroenterol. 1992; 15:238–241.23. Mourani S, Dobbs SM, Genta RM, Tandon AK, Yoffe B. Hepatitis A virus-associated cholecystitis. Ann Intern Med. 1994; 120:398–400.24. Dinulos J, Mitchell DK, Egerton J, Pickering LK. Hydrops of the gallbladder associated with Epstein-Barr virus infection: a report of two cases and review of the literature. Pediatr Infect Dis J. 1994; 13:924–929.25. Bloom RA, Swain VA. Non-calculous distension of the gall-bladder in childhood. Arch Dis Child. 1966; 41:503–508.26. Egritas O, Nacar N, Hanioglu S, Soyer T, Tezic T. Early but prolonged gallbladder hydrops in a 7-month-old girl with Kawasaki syndrome: report of a case. Surg Today. 2007; 37:162–164.27. van Breda Vriesman AC, Engelbrecht MR, Smithuis RH, Puylaert JB. Diffuse gallbladder wall thickening: differential diagnosis. AJR Am J Roentgenol. 2007; 188:495–501.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Acalculous Diffuse Gallbladder Wall Thickening in Children
- A Case of Gallbladder Perforation Complicated by Acalculous Cholecystitis due to Non-Typhoidal Salmonella
- A Case of Acute Acalculous Cholecystitis in a Patient with Systemic Lupus Erythematosus
- Necrotizing Gallbladder Torsion Masking as Acalculous Cholecystitis: A Review of Two Cases Treated with Successful Laparoscopic Cholecystectomy
- Acalculous Hemorrhagic Cholecystitis with Chronic Intraluminal Hematoma: MRI Findings