Obstet Gynecol Sci.
2020 Jan;63(1):35-41. 10.5468/ogs.2020.63.1.35.
Can the cervical length in mid-trimester predict the use of vacuum in vaginal delivery?
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University Bundang Hospital, Seongnam, Korea.
- 2Department of Obstetrics and Gynecology, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea. jshmom04@gmail.com
- KMID: 2467930
- DOI: http://doi.org/10.5468/ogs.2020.63.1.35
Abstract
OBJECTIVE
This study aimed to evaluate whether an increased cervical length (CL) measured in the mid-trimester is associated with vacuum-assisted vaginal delivery.
METHODS
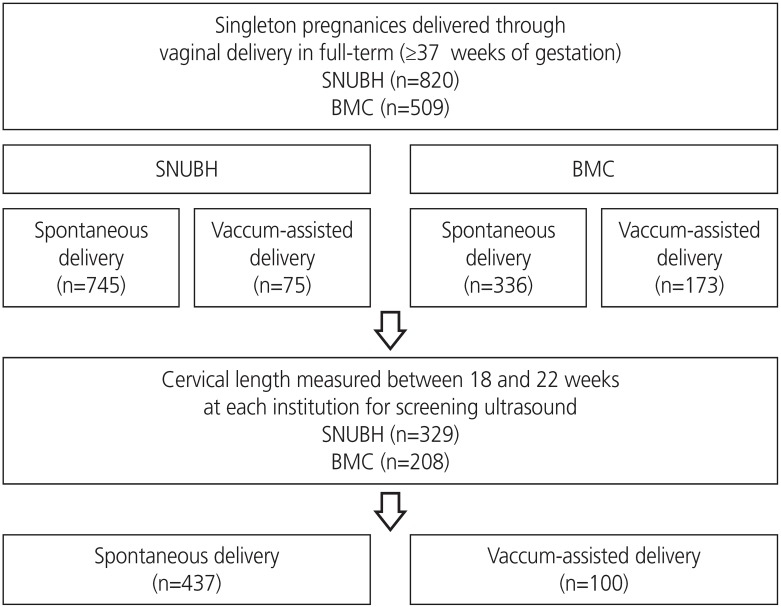
This retrospective cohort study included women who delivered vaginally in Seoul National University Bundang Hospital (n=820) and Boramae Medical Center (n=509) between January 2017 and February 2019. Multifetal pregnancies and preterm births before 37 weeks of gestation were excluded. Only those cases in which CL was measured at 18-22 weeks of gestation for the purpose of screening for preterm birth risk in each institution were analyzed (n=537). Other significant risk factors were reviewed.
RESULTS
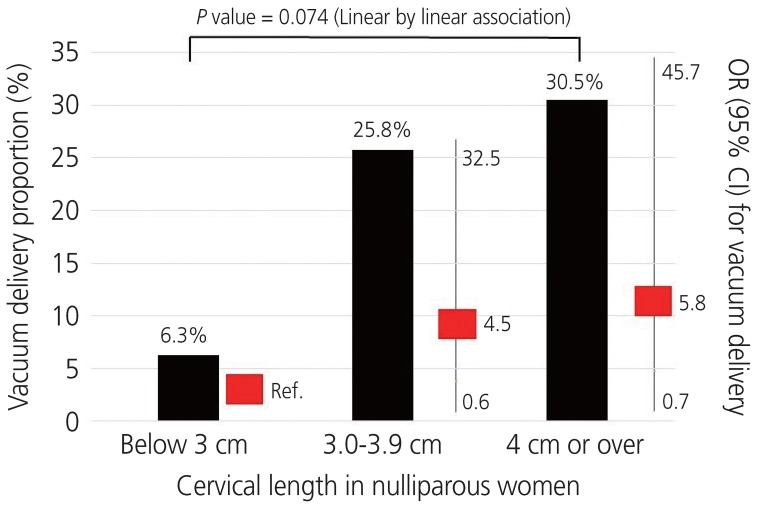
The median gestational age at delivery was 39.4 weeks (range, 37.0-41.6 weeks); 18.6% (100/537) were vacuum-assisted delivery. There was no relationship between mid-trimester CL and vacuum-assisted delivery (odds ratio [OR], 0.96; 95% confidence interval [CI], 0.57-1.62), while nulliparity was associated with a higher risk (OR, 3.64; 95% CI, 1.55-8.57) than multiparity. When the population was divided into 3 groups by CL range, vacuum-assisted delivery rates increased as CL length increased in nulliparous women.
CONCLUSION
Mid-trimester CL did not predict the need for vacuum-assisted vaginal delivery.
Keyword
MeSH Terms
Figure
Reference
-
1. Jeon J, Na S. Vacuum extraction vaginal delivery: current trend and safety. Obstet Gynecol Sci. 2017; 60:499–505. PMID: 29184857.
Article2. Merriam AA, Ananth CV, Wright JD, Siddiq Z, D'Alton ME, Friedman AM. Trends in operative vaginal delivery, 2005–2013: a population-based study. BJOG. 2017; 124:1365–1372. PMID: 28236337.
Article3. Verhoeven CJ, Nuij C, Janssen-Rolf CR, Schuit E, Bais JM, Oei SG, et al. Predictors for failure of vacuum-assisted vaginal delivery: a case-control study. Eur J Obstet Gynecol Reprod Biol. 2016; 200:29–34. PMID: 26967343.
Article4. McQuivey RW. Vacuum-assisted delivery: a review. J Matern Fetal Neonatal Med. 2004; 16:171–180. PMID: 15590444.
Article5. Metz TD, Gonzalez C, Allshouse AA, Henry E, Esplin S. Influence of patient-level factors on mode of delivery among operative vaginal delivery candidates in modern practice. Am J Perinatol. 2017; 34:974–981. PMID: 28376550.6. Muraca GM, Sabr Y, Lisonkova S, Skoll A, Brant R, Cundiff GW, et al. Morbidity and mortality associated with forceps and vacuum delivery at outlet, low, and midpelvic station. J Obstet Gynaecol Can. 2019; 41:327–337. PMID: 30366887.
Article7. Ghidini A, Stewart D, Pezzullo JC, Locatelli A. Neonatal complications in vacuum-assisted vaginal delivery: are they associated with number of pulls, cup detachments, and duration of vacuum application? Arch Gynecol Obstet. 2017; 295:67–73. PMID: 27677283.
Article8. Lund NS, Persson LK, Jangö H, Gommesen D, Westergaard HB. Episiotomy in vacuum-assisted delivery affects the risk of obstetric anal sphincter injury: a systematic review and meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2016; 207:193–199. PMID: 27865945.
Article9. Dall'Asta A, Ghi T, Pedrazzi G, Frusca T. Does vacuum delivery carry a higher risk of shoulder dystocia? Review and meta-analysis of the literature. Eur J Obstet Gynecol Reprod Biol. 2016; 204:62–68. PMID: 27522245.10. Lacker C. Preventing maternal and neonatal harm during vacuum-assisted vaginal delivery. Am J Nurs. 2012; 112:65–69.
Article11. Vacca A. Vacuum-assisted delivery. Best Pract Res Clin Obstet Gynaecol. 2002; 16:17–30. PMID: 11866494.
Article12. Hatfield AS, Sanchez-Ramos L, Kaunitz AM. Sonographic cervical assessment to predict the success of labor induction: a systematic review with metaanalysis. Am J Obstet Gynecol. 2007; 197:186–192. PMID: 17689645.
Article13. Kahrs BH, Usman S, Ghi T, Youssef A, Torkildsen EA, Lindtjorn E, et al. Sonographic prediction of outcome of vacuum deliveries: a multicenter, prospective cohort study. Am J Obstet Gynecol. 2017; 217:69.e1–69.10. PMID: 28327433.14. Herstad L, Klungsøyr K, Skjaerven R, Tanbo T, Forsén L, Åbyholm T, et al. Maternal age and emergency operative deliveries at term: a population-based registry study among low-risk primiparous women. BJOG. 2015; 122:1642–1651. PMID: 25100277.
Article15. Miller ES, Sakowicz A, Grobman WA. Association between second-trimester cervical length and primary cesarean delivery. Obstet Gynecol. 2013; 122:863–867. PMID: 24084546.
Article16. Sung SJ, Lee SM, Oh S, Choi JH, Park JY, Kim BJ, et al. Mid-pregnancy cervical length as a risk factor for cesarean section in women with twin pregnancies. J Perinat Med. 2018; 46:780–785. PMID: 29461973.
Article17. van de Mheen L, Schuit E, Liem SM, Lim AC, Bekedam DJ, Goossens SM, et al. Second-trimester cervical length as risk indicator for Cesarean delivery in women with twin pregnancy. Ultrasound Obstet Gynecol. 2015; 46:579–584. PMID: 25402630.
Article18. Smith GC, Celik E, To M, Khouri O, Nicolaides KH. Fetal Medicine Foundation Second Trimester Screening Group. Cervical length at mid-pregnancy and the risk of primary cesarean delivery. N Engl J Med. 2008; 358:1346–1353. PMID: 18367737.
Article19. Parry S, Simhan H, Elovitz M, Iams J. Universal maternal cervical length screening during the second trimester: pros and cons of a strategy to identify women at risk of spontaneous preterm delivery. Am J Obstet Gynecol. 2012; 207:101–106. PMID: 22633270.
Article20. Szychowski JM, Owen J, Hankins G, Iams J, Sheffield J, Perez-Delboy A, et al. Timing of mid-trimester cervical length shortening in high-risk women. Ultrasound Obstet Gynecol. 2009; 33:70–75. PMID: 19072745.
Article21. Colombo DF, Iams JD. Cervical length and preterm labor. Clin Obstet Gynecol. 2000; 43:735–745. PMID: 11100291.
Article22. Owen J, Szychowski JM, Hankins G, Iams JD, Sheffield JS, Perez-Delboy A, et al. Does midtrimester cervical length ≥25 mm predict preterm birth in high-risk women? Am J Obstet Gynecol. 2010; 203:393.e1–393.e5. PMID: 20708169.
Article23. Society for Maternal-Fetal Medicine, McIntosh J, Feltovich H, Berghella V, Manuck T. The role of routine cervical length screening in selected high- and low-risk women for preterm birth prevention. Am J Obstet Gynecol. 2016; 215:B2–7.
Article24. Khalifeh A, Berghella V. Universal cervical length screening in singleton gestations without a previous preterm birth: ten reasons why it should be implemented. Am J Obstet Gynecol. 2016; 214:603.e1–603.e5. PMID: 26707072.25. Boelig RC, Orzechowski KM, Berghella V. Cervical length, risk factors, and delivery outcomes among women with spontaneous preterm birth. J Matern Fetal Neonatal Med. 2016; 29:2840–2844. PMID: 26452324.
Article26. Werner EF, Hamel MS, Orzechowski K, Berghella V, Thung SF. Cost-effectiveness of transvaginal ultrasound cervical length screening in singletons without a prior preterm birth: an update. Am J Obstet Gynecol. 2015; 213:554.e1–554.e6. PMID: 26071914.
Article27. Orzechowski KM, Boelig R, Nicholas SS, Baxter J, Berghella V. Is universal cervical length screening indicated in women with prior term birth? Am J Obstet Gynecol. 2015; 212:234.e1–234.e5. PMID: 25174798.
Article28. Berghella V. Universal cervical length screening for prediction and prevention of preterm birth. Obstet Gynecol Surv. 2012; 67:653–658. PMID: 23112072.
Article29. Boelig RC, Suhag A, Guarente J, Orzechowski K, Berghella V. Second-trimester cervical length and outcomes of induction of labor at term. J Matern Fetal Neonatal Med. 2018; 31:1040–1044. PMID: 28393580.
Article30. Boelig RC, Orzechowski KM, Suhag A, Berghella V. Second trimester cervical length and prolonged pregnancy. J Matern Fetal Neonatal Med. 2016; 29:4088–4091. PMID: 26952543.
Article31. Nicholas SS, Orzechowski KM, Berghella V, Baxter JK. Second trimester cervical length and its association with vaginal birth after cesarean delivery. Am J Perinatol. 2016; 33:20–23. PMID: 26084747.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vacuum extraction vaginal delivery: current trend and safety
- A Comparative Study of Oral and Vaginal Misoprostol Administration in Mid-trimester Pregnancy Termination
- Uterine Cervical Length Measurement by Transvaginal Ultrasonography for Prediction of Preterm Delivery
- Maternal Characteristics, Short Mid-Trimester Cervical Length, and Preterm Delivery
- A Study Female of Fecal Incontinence: Effects of Parity & Delivery method