J Korean Assoc Oral Maxillofac Surg.
2019 Apr;45(2):68-75. 10.5125/jkaoms.2019.45.2.68.
Chronic non-bacterial osteomyelitis in the jaw
- Affiliations
-
- 1Oral and Maxillofacial Microvascular Reconstruction LAB, Brong Ahafo Regional Hospital, Sunyani, Ghana.
- 2Department of Oral and Maxillofacial Surgery, School of Dentistry and Dental Research Institute, Seoul National University, Seoul, Korea.
- 3Department of Oral Pathology, College of Dentistry and Institute of Oral Science, Gangneung-Wonju National University, Gangneung, Korea. sukkeunlee@hanmail.net
- KMID: 2467149
- DOI: http://doi.org/10.5125/jkaoms.2019.45.2.68
Abstract
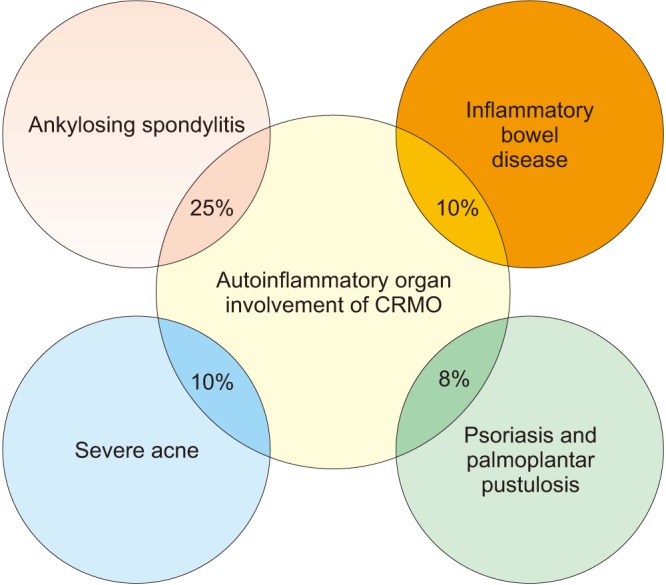
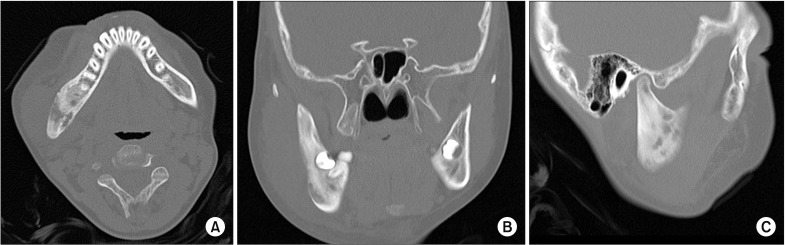
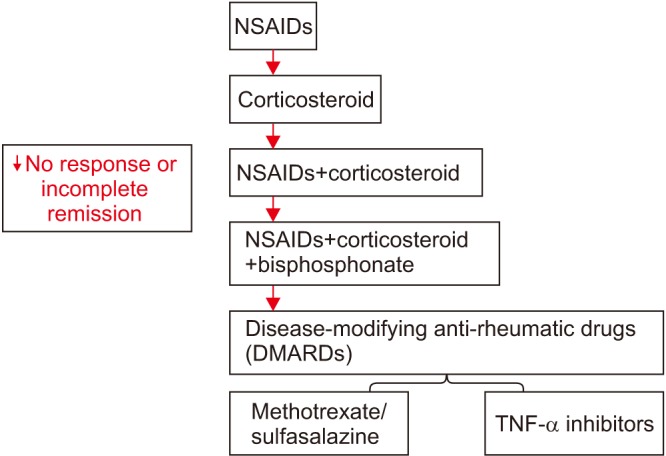
- Chronic recurrent multifocal osteomyelitis (CRMO) is one of the most severe form of chronic non-bacterial osteomyelitis (CNO), which could result in bone and related tissue damage. This autoinflammatory bone disorder (ABD) is very difficult for its clinical diagnosis because of no diagnostic criteria or biomarkers. CRMO in the jaw must be suspected in the differential diagnosis of chronic and recurrent bone pain in the jaw, and a bone biopsy should be considered in chronic and relapsing bone pain with swelling that is unresponsive to treatment. The early diagnosis of CRMO in the jaw will prevent unnecessary and prolonged antibiotic usage or unnecessary surgical intervention. The updated researches for the identification of genetic and molecular alterations in CNO/CRMO should be studied more for its correct pathophysiological causes and proper treatment guidelines. Although our trial consisted of reporting items from Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), there are very few articles of randomized controlled trials. This article was summarized based on the author's diverse clinical experiences. This paper reviews the clinical presentation of CNO/CRMO with its own pathogenesis, epidemiology, recent research studies, and general medications. Treatment and monitoring of the jaw are essential for the clear diagnosis and management of CNO/CRMO patients in the field of dentistry and maxillofacial surgery.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
An accurate diagnosis of odontogenic cutaneous sinus tract by different computed tomography unit setting
Buyanbileg Sodnom-Ish, Mi Young Eo, Soung Min Kim
J Korean Assoc Oral Maxillofac Surg. 2021;47(1):51-56. doi: 10.5125/jkaoms.2021.47.1.51.
Reference
-
1. Hofmann SR, Schnabel A, Rösen-Wolff A, Morbach H, Girschick HJ, Hedrich CM. Chronic nonbacterial osteomyelitis: pathophysiological concepts and current treatment strategies. J Rheumatol. 2016; 43:1956–1964. PMID: 27585682.
Article2. Hofmann SR, Kapplusch F, Girschick HJ, Morbach H, Pablik J, Ferguson PJ, et al. Chronic recurrent multifocal osteomyelitis (CRMO): presentation, pathogenesis, and treatment. Curr Osteoporos Rep. 2017; 15:542–544. PMID: 29080202.
Article3. Giedion A, Holthusen W, Masel LF, Vischer D. Subacute and chronic “symmetrical” osteomyelitis. . Ann Radiol (Paris). 1972; 15:329–342. PMID: 4403064.4. Andersson R. Effective treatment with interferon-alpha in chronic recurrent multifocal osteomyelitis. J Interferon Cytokine Res. 1995; 15:837–838. PMID: 8564704.5. Wang Y, Yang C, Zhang W, Lu Y, Wei W, Han Z, et al. Monofocal chronic nonbacterial osteomyelitis in the mandible accompanied with mucocutaneous disease. J Craniofac Surg. 2017; 28:e547–e551. PMID: 28692524.
Article6. Padwa BL, Dentino K, Robson CD, Woo SB, Kurek K, Resnick CM. Pediatric chronic nonbacterial osteomyelitis of the jaw: clinical, radiographic, and histopathologic features. J Oral Maxillofac Surg. 2016; 74:2393–2402. PMID: 27318191.
Article7. Monsour PA, Dalton JB. Chronic recurrent multifocal osteomyelitis involving the mandible: case reports and review of the literature. Dentomaxillofac Radiol. 2010; 39:184–190. PMID: 20203282.
Article8. Hedrich CM, Hahn G, Girschick HJ, Morbach H. A clinical and pathomechanistic profile of chronic nonbacterial osteomyelitis/chronic recurrent multifocal osteomyelitis and challenges facing the field. Expert Rev Clin Immunol. 2013; 9:845–854. PMID: 24070048.
Article9. Hedrich CM, Hofmann SR, Pablik J, Morbach H, Girschick HJ. Autoinflammatory bone disorders with special focus on chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J. 2013; 11:47. PMID: 24359092.
Article10. Stern SM, Ferguson PJ. Autoinflammatory bone diseases. Rheum Dis Clin North Am. 2013; 39:735–749. PMID: 24182852.
Article11. El-Shanti HI, Ferguson PJ. Chronic recurrent multifocal osteomyelitis: a concise review and genetic update. Clin Orthop Relat Res. 2007; 462:11–19. PMID: 17496555.12. Borzutzky A, Stern S, Reiff A, Zurakowski D, Steinberg EA, Dedeoglu F, et al. Pediatric chronic nonbacterial osteomyelitis. Pediatrics. 2012; 130:e1190–e1197. PMID: 23071213.
Article13. Hofmann C, Wurm M, Schwarz T, Neubauer H, Beer M, Girschick H, et al. A standardized clinical and radiological follow-up of patients with chronic non-bacterial osteomyelitis treated with pamidronate. Clin Exp Rheumatol. 2014; 32:604–609. PMID: 25065777.14. Khanna G, Sato TS, Ferguson P. Imaging of chronic recurrent multifocal osteomyelitis. Radiographics. 2009; 29:1159–1177. PMID: 19605663.
Article15. Jurik AG, Egund N. MRI in chronic recurrent multifocal osteomyelitis. Skeletal Radiol. 1997; 26:230–238. PMID: 9151372.
Article16. Morbach H, Schneider P, Schwarz T, Hofmann C, Raab P, Neubauer H, et al. Comparison of magnetic resonance imaging and 99mTechnetium-labelled methylene diphosphonate bone scintigraphy in the initial assessment of chronic non-bacterial osteomyelitis of childhood and adolescents. Clin Exp Rheumatol. 2012; 30:578–582. PMID: 22765947.17. Beck C, Girschick HJ, Morbach H, Schwarz T, Yimam T, Frenkel J, et al. Mutation screening of the IL-1 receptor antagonist gene in chronic non-bacterial osteomyelitis of childhood and adolescence. Clin Exp Rheumatol. 2011; 29:1040–1043. PMID: 22032624.18. Golla A, Jansson A, Ramser J, Hellebrand H, Zahn R, Meitinger T, et al. Chronic recurrent multifocal osteomyelitis (CRMO): evidence for a susceptibility gene located on chromosome 18q21.3–18q22. Eur J Hum Genet. 2002; 10:217–221. PMID: 11973628.
Article19. Nakashima T, Takayanagi H. Osteoimmunology: crosstalk between the immune and bone systems. J Clin Immunol. 2009; 29:555–567. PMID: 19585227.
Article20. Nakashima T, Takayanagi H. Osteoclasts and the immune system. J Bone Miner Metab. 2009; 27:519–529. PMID: 19455385.
Article21. Sharma M, Ferguson PJ. Autoinflammatory bone disorders: update on immunologic abnormalities and clues about possible triggers. Curr Opin Rheumatol. 2013; 25:658–664. PMID: 23917160.22. Hamel J, Paul D, Gahr M, Hedrich CM. Pilot study: possible association of IL10 promoter polymorphisms with CRMO. Rheumatol Int. 2012; 32:555–556. PMID: 21240493.
Article23. Hofmann SR, Kubasch AS, Ioannidis C, Rösen-Wolff A, Girschick HJ, Morbach H, et al. Altered expression of IL-10 family cytokines in monocytes from CRMO patients result in enhanced IL-1β expression and release. Clin Immunol. 2015; 161:300–307. PMID: 26404542.
Article24. Hofmann SR, Morbach H, Schwarz T, Rösen-Wolff A, Girschick HJ, Hedrich CM. Attenuated TLR4/MAPK signaling in monocytes from patients with CRMO results in impaired IL-10 expression. Clin Immunol. 2012; 145:69–76. PMID: 22940633.
Article25. Hofmann SR, Schwarz T, Möller JC, Morbach H, Schnabel A, Rösen-Wolff A, et al. Chronic non-bacterial osteomyelitis is associated with impaired Sp1 signaling, reduced IL10 promoter phosphorylation, and reduced myeloid IL-10 expression. Clin Immunol. 2011; 141:317–327. PMID: 21925952.
Article26. Hedrich CM, Bream JH. Cell type-specific regulation of IL-10 expression in inflammation and disease. Immunol Res. 2010; 47:185–206. PMID: 20087682.
Article27. Hofmann SR, Rösen-Wolff A, Tsokos GC, Hedrich CM. Biological properties and regulation of IL-10 related cytokines and their contribution to autoimmune disease and tissue injury. Clin Immunol. 2012; 143:116–127. PMID: 22459704.
Article28. Lindor NM, Arsenault TM, Solomon H, Seidman CE, McEvoy MT. A new autosomal dominant disorder of pyogenic sterile arthritis, pyoderma gangrenosum, and acne: PAPA syndrome. Mayo Clin Proc. 1997; 72:611–615. PMID: 9212761.
Article29. Smith EJ, Allantaz F, Bennett L, Zhang D, Gao X, Wood G, et al. Clinical, molecular, and genetic characteristics of PAPA syndrome: a review. Curr Genomics. 2010; 11:519–527. PMID: 21532836.30. Shreiner AB, Kao JY, Young VB. The gut microbiome in health and in disease. Curr Opin Gastroenterol. 2015; 31:69–75. PMID: 25394236.
Article31. Liao HJ, Chyuan IT, Wu CS, Lin SW, Chen KH, Tsai HF, et al. Increased neutrophil infiltration, IL-1 production and a SAPHO syndrome-like phenotype in PSTPIP2-deficient mice. Rheumatology (Oxford). 2015; 54:1317–1326. PMID: 25602062.
Article32. Schnabel A, Range U, Hahn G, Siepmann T, Berner R, Hedrich CM. Unexpectedly high incidences of chronic non-bacterial as compared to bacterial osteomyelitis in children. Rheumatol Int. 2016; 36:1737–1745. PMID: 27730289.
Article33. Morbach H, Hedrich CM, Beer M, Girschick HJ. Autoinflammatory bone disorders. Clin Immunol. 2013; 147:185–196. PMID: 23369460.
Article34. Cassel SL, Janczy JR, Bing X, Wilson SP, Olivier AK, Otero JE, et al. Inflammasome-independent IL-1β mediates autoinflammatory disease in Pstpip2-deficient mice. Proc Natl Acad Sci U S A. 2014; 111:1072–1077. PMID: 24395802.
Article35. Chitu V, Nacu V, Charles JF, Henne WM, McMahon HT, Nandi S, et al. PSTPIP2 deficiency in mice causes osteopenia and increased differentiation of multipotent myeloid precursors into osteoclasts. Blood. 2012; 120:3126–3135. PMID: 22923495.
Article36. Grosse J, Chitu V, Marquardt A, Hanke P, Schmittwolf C, Zeitlmann L, et al. Mutation of mouse Mayp/Pstpip2 causes a macrophage autoinflammatory disease. Blood. 2006; 107:3350–3358. PMID: 16397132.
Article37. Greenhill CJ, Jones GW, Nowell MA, Newton Z, Harvey AK, Moideen AN, et al. Interleukin-10 regulates the inflammasome-driven augmentation of inflammatory arthritis and joint destruction. Arthritis Res Ther. 2014; 16:419. PMID: 25175678.
Article38. Scianaro R, Insalaco A, Bracci Laudiero L, De Vito R, Pezzullo M, Teti A, et al. Deregulation of the IL-1β axis in chronic recurrent multifocal osteomyelitis. Pediatr Rheumatol Online J. 2014; 12:30. PMID: 25061439.
Article39. Cox AJ, Darbro BW, Laxer RM, Velez G, Bing X, Finer AL, et al. Recessive coding and regulatory mutations in FBLIM1 underlie the pathogenesis of chronic recurrent multifocal osteomyelitis (CRMO). PLoS One. 2017; 12:e0169687. PMID: 28301468.
Article40. Ferguson PJ, El-Shanti HI. Autoinflammatory bone disorders. Curr Opin Rheumatol. 2007; 19:492–498. PMID: 17762617.
Article41. Jansson AF, Müller TH, Gliera L, Ankerst DP, Wintergerst U, Belohradsky BH, et al. Clinical score for nonbacterial osteitis in children and adults. Arthritis Rheum. 2009; 60:1152–1159. PMID: 19333943.
Article42. Beck C, Morbach H, Beer M, Stenzel M, Tappe D, Gattenlöhner S, et al. Chronic nonbacterial osteomyelitis in childhood: prospective follow-up during the first year of anti-inflammatory treatment. Arthritis Res Ther. 2010; 12:R74. PMID: 20433730.
Article44. Girschick HJ, Zimmer C, Klaus G, Darge K, Dick A, Morbach H. Chronic recurrent multifocal osteomyelitis: what is it and how should it be treated? Nat Clin Pract Rheumatol. 2007; 3:733–738. PMID: 18037933.
Article45. Holden W, David J. Chronic recurrent multifocal osteomyelitis: two cases of sacral disease responsive to corticosteroids. Clin Infect Dis. 2005; 40:616–619. PMID: 15712088.
Article46. Miettunen PM, Wei X, Kaura D, Reslan WA, Aguirre AN, Kellner JD. Dramatic pain relief and resolution of bone inflammation following pamidronate in 9 pediatric patients with persistent chronic recurrent multifocal osteomyelitis (CRMO). Pediatr Rheumatol Online J. 2009; 7:2. PMID: 19138427.
Article47. Compeyrot-Lacassagne S, Rosenberg AM, Babyn P, Laxer RM. Pamidronate treatment of chronic noninfectious inflammatory lesions of the mandible in children. J Rheumatol. 2007; 34:1585–1589. PMID: 17611964.48. Eleftheriou D, Gerschman T, Sebire N, Woo P, Pilkington CA, Brogan PA. Biologic therapy in refractory chronic non-bacterial osteomyelitis of childhood. Rheumatology (Oxford). 2010; 49:1505–1512. PMID: 20430869.
Article49. Schnabel A, Range U, Hahn G, Berner R, Hedrich CM. Treatment response and longterm outcomes in children with chronic nonbacterial osteomyelitis. J Rheumatol. 2017; 44:1058–1065. PMID: 28461645.
Article50. Herlin T, Fiirgaard B, Bjerre M, Kerndrup G, Hasle H, Bing X, et al. Efficacy of anti-IL-1 treatment in Majeed syndrome. Ann Rheum Dis. 2013; 72:410–413. PMID: 23087183.
Article51. Hofmann SR, Kubasch AS, Range U, Laass MW, Morbach H, Girschick HJ, et al. Serum biomarkers for the diagnosis and monitoring of chronic recurrent multifocal osteomyelitis (CRMO). Rheumatol Int. 2016; 36:769–779. PMID: 27000045.
Article52. Miettunen PMH. Chronic non-bacterial osteitis/chronic recurrent multifocal osteomyelitis. In : Baptista MS, Tardivo JP, editors. Osteomyelitis. London: InTech;2012. p. 89–118.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Chronic maxillary sinusitis and diabetes related maxillary osteonecrosis: a case report
- Clinical study of chronic osteomyelitis
- Chronic Recurrent Multifocal Osteomyelitis: A Case Report
- Pathological Fracture of The Distal Femur, Caused by Chronic Actinomycotic Osteomyelitis: A case report
- Treatment of Chronic Osteomyelitis by Transplantation of Autogenous Omentum with Microvascular Anastomosis