Neonatal Med.
2019 Nov;26(4):218-222. 10.5385/nm.2019.26.4.218.
A Rare Case of Eosinophilic Gastroenteritis in a Neonate with Fever
- Affiliations
-
- 1Department of Pediatrics, Inje University Haeundae Paik Hospital, Busan, Korea.
- 2Department of Pediatrics, Soonchunhyang University Gumi Hospital, Gumi, Korea. myong47@hanmail.net
- KMID: 2466642
- DOI: http://doi.org/10.5385/nm.2019.26.4.218
Abstract
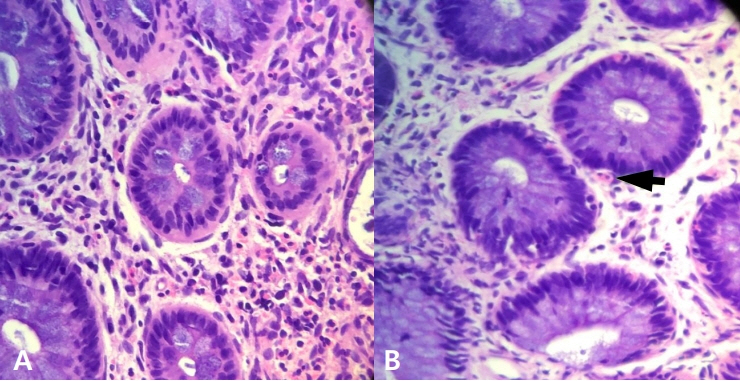
- Eosinophilic gastroenteritis is a member of eosinophilic gastrointestinal (GI) diseases and is characterized by the accumulation of eosinophils within the GI tract. Common symptoms of eosinophilic gastroenteritis are vomiting, abdominal pain, dysphagia, and weight loss, but rare fever in neonate. This report describes a 10-day-old boy who developed fever, bloody mucoid stool, and bilious vomiting resulting from eosinophilic gastroenteritis, mimicking sepsis. Sigmoidoscopy and pathologic findings revealed mucosal edema, small hemorrhagic spot, and segmental erythemoid edema in the colon and increased number of eosinophils in the lamina propria with intraepithelial eosinophils. After breast milk feeding with restriction of milk from the mother for 6 months, specific immunoglobulin to milk was class 0 (class 3, previous). The boy restarted formula feeding, and he had no fever and GI symptoms.
Keyword
MeSH Terms
Figure
Reference
-
1. Spergel JM, Book WM, Mays E, Song L, Shah SS, Talley NJ, et al. Variation in prevalence, diagnostic criteria, and initial management options for eosinophilic gastrointestinal diseases in the United States. J Pediatr Gastroenterol Nutr. 2011; 52:300–6.2. Guajardo JR, Plotnick LM, Fende JM, Collins MH, Putnam PE, Rothenberg ME. Eosinophil-associated gastrointestinal disorders: a world-wide-web based registry. J Pediatr. 2002; 141:576–81.3. Whitaker IS, Gulati A, McDaid JO, Bugajska-Carr U, Arends MJ. Eosinophilic gastroenteritis presenting as obstructive jaundice. Eur J Gastroenterol Hepatol. 2004; 16:407–9.4. Treiber GG, Weidner S. Eosinophilic gastroenteritis. Clin Gastroenterol Hepatol. 2007; 5:e16.5. Rothenberg ME. Eosinophilic gastrointestinal disorders (EGID). J Allergy Clin Immunol. 2004; 113:11–28. ; quiz 29.6. Chehade M, Aceves SS. Food allergy and eosinophilic esophagitis. Curr Opin Allergy Clin Immunol. 2010; 10:231–7.7. Lucendo AJ, Arias A. Eosinophilic gastroenteritis: an update. Expert Rev Gastroenterol Hepatol. 2012; 6:591–601.8. Abassa KK, Lin XY, Xuan JY, Zhou HX, Guo YW. Diagnosis of eosinophilic gastroenteritis is easily missed. World J Gastroenterol. 2017; 23:3556–64.9. Sopo SM, Filoni S, Giorgio V, Monaco S, Onesimo R. Food protein-induced enterocolitis syndrome (FPIES) to corn: a case report. J Investig Allergol Clin Immunol. 2012; 22:391–2.10. Nomura I, Morita H, Hosokawa S, Hoshina H, Fukuie T, Watanabe M, et al. Four distinct subtypes of non-IgE-mediated gastrointestinal food allergies in neonates and infants, distinguished by their initial symptoms. J Allergy Clin Immunol. 2011; 127:685–8.11. Fogg MI, Brown-Whitehorn TA, Pawlowski NA, Spergel JM. Atopy patch test for the diagnosis of food protein-induced enterocolitis syndrome. Pediatr Allergy Immunol. 2006; 17:351–5.12. Eigenmann PA, Belli DC, Ludi F, Kahn JM, Polla BS. In vitro lymphocyte proliferation with milk and a casein-whey protein hydrolyzed formula in children with cow's milk allergy. J Allergy Clin Immunol. 1995; 96:549–57.13. Bolukbas FF, Bolukbas C, Uzunkoy A, Baba F, Horoz M, Ozturk E. A dramatic response to ketotifen in a case of eosinophilic gastroenteritis mimicking abdominal emergency. Dig Dis Sci. 2004; 49:1782–5.14. Bischoff SC. Food allergy and eosinophilic gastroenteritis and colitis. Curr Opin Allergy Clin Immunol. 2010; 10:238–45.15. Chehade M, Magid MS, Mofidi S, Nowak-Wegrzyn A, Sampson HA, Sicherer SH. Allergic eosinophilic gastroenteritis with protein-losing enteropathy: intestinal pathology, clinical course, and long-term follow-up. J Pediatr Gastroenterol Nutr. 2006; 42:516–21.16. Tan AC, Kruimel JW, Naber TH. Eosinophilic gastroenteritis treated with non-enteric-coated budesonide tablets. Eur J Gastroenterol Hepatol. 2001; 13:425–7.17. Siewert E, Lammert F, Koppitz P, Schmidt T, Matern S. Eosinophilic gastroenteritis with severe protein-losing enteropathy: successful treatment with budesonide. Dig Liver Dis. 2006; 38:55–9.18. Choi BS, Hong SJ, Park SH, Kim HM, Choe BH. Differences in features and course of mucosal type eosinophilic gastroenteritis between Korean infants and children. J Korean Med Sci. 2015; 30:1129–35.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Eosinophilic Cholecystitis associated with Eosinophilic Cholangitis and Pancreatitis
- Diffuse Eosinophilic Gastroenteritis with Antral Obstruction: A Case Report
- A Case of Eosinophilic Gastroenteritis Presenting with Fever and Multiple Lymphadenopathy
- A Case of Eosinophilic Gastroenteritis in a Child
- Serosal Type Eosinophilic Gastroenteritis