J Korean Ophthalmol Soc.
2019 Dec;60(12):1307-1311. 10.3341/jkos.2019.60.12.1307.
Metastatic Small Cell Neuroendocrine Carcinoma to the Orbit Manifesting as Total Ophthalmoplegia
- Affiliations
-
- 1Department of Ophthalmology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. mojili914@hanmail.net
- 2Department of Pathology, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea.
- KMID: 2466187
- DOI: http://doi.org/10.3341/jkos.2019.60.12.1307
Abstract
- PURPOSE
To report a case of primary ureteral small cell neuroendocrine carcinoma metastasis in the left orbital wall, with a review of the literature.
CASE SUMMARY
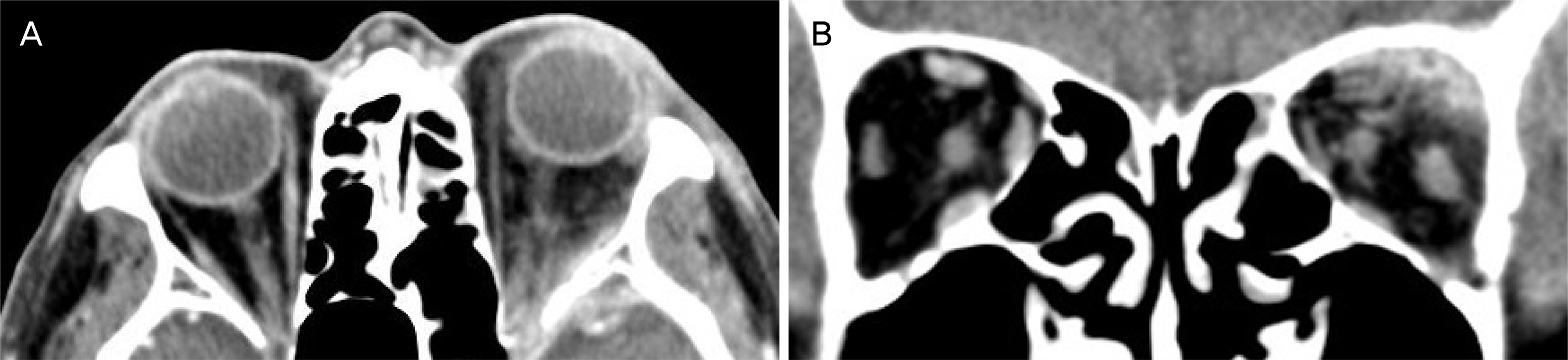
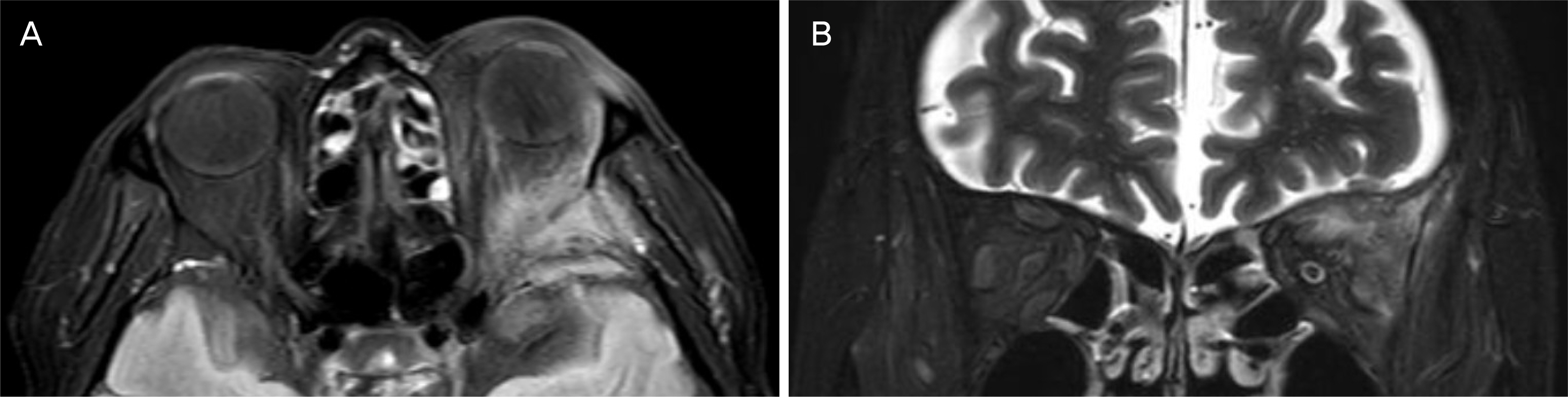
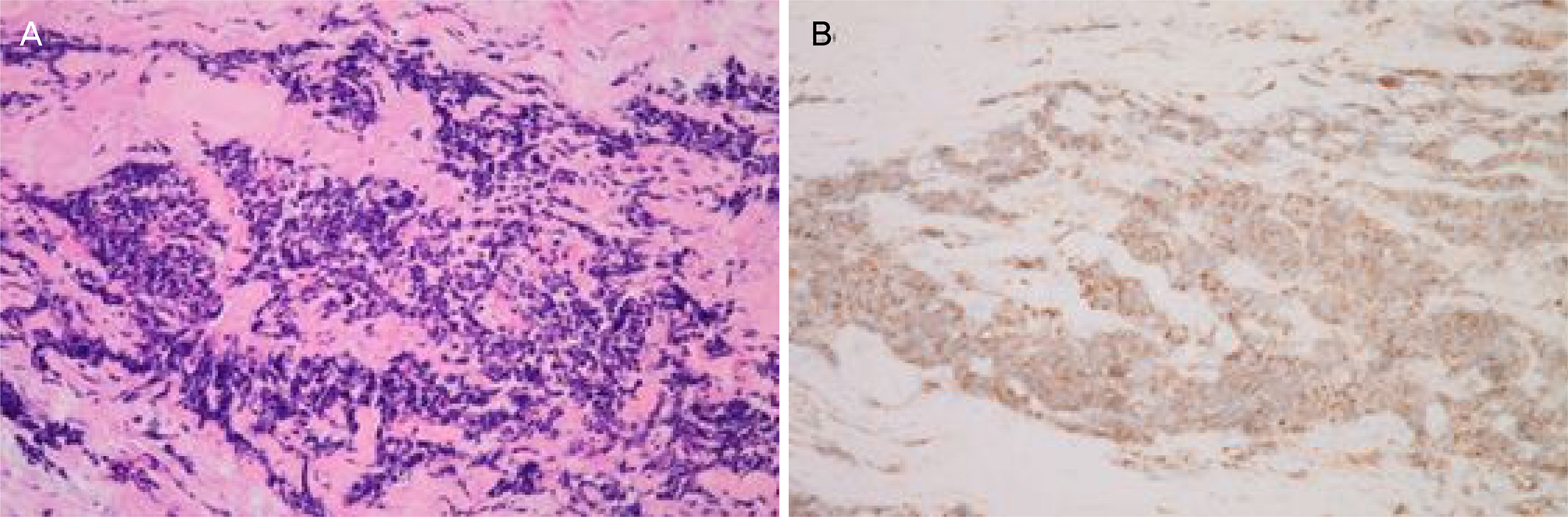
A 79-year-old male visited our clinic with a 10 day history of ocular pain, ptosis, and ophthalmoplegia in the left eye. He had been diagnosed with diabetes mellitus and was being treated for prostate adenocarcinoma. The corrected visual acuity was 0.8 in the right eye and 0.5 in the left eye. An extraocular movement test showed total ophthalmoplegia, mild exophthalmos, and ptosis in the left eye. Orbital computed tomography (CT) and magnetic resonance imaging showed an irregular mass-like enhancement in the superolateral orbital wall of the left eye, suggesting infectious and inflammatory orbital disease. After antibiotic treatment, high dose systemic steroids were administered. However, there was no improvement and the orbital CT was again performed, with no changes. A surgical biopsy for differentiating orbital tumors was performed and diagnosed as a metastatic orbital small cell neuroendocrine carcinoma. Using positron emission tomography, he was later diagnosed with a metastatic orbital small cell neuroendocrine carcinoma with multiple metastases.
CONCLUSIONS
When the patient has a mass-like lesion on imaging with ocular pain, ophthalmoplegia, or ptosis, a surgical biopsy should be performed to make a diagnosis and determine the optimal management.
MeSH Terms
Figure
Reference
-
References
1. Bloch RS, Gartner S. The incidence of ocular metastatic carcinoma. Arch Ophthalmol. 1971; 85:673–5.
Article2. Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol. 2007; 18:405–13.
Article3. Char DH, Miller T, Kroll S. Orbital metastasis: diagnosis and course. Br J Ophthalmol. 1997; 81:386–90.4. Papathanassiou M, Nikita E, Theodossiadis P, Vergados I. Orbital metastasis secondary to breast cancer mimicking thyroid-associated ophthalmopathy. Clin Exp Optom. 2010; 93:368–9.
Article5. Goldberg RA, Rootman J, Cline RA. Tumors metastatic to the abdominal: a changing picture. Surv Ophthalmol. 1990; 35:1–24.6. Barker JL Jr, Glisson BS, Garden AS, et al. Management of non-sinonasal neuroendocrine carcinomas of the head and neck. Cancer. 2003; 98:2322–8.
Article7. Fisseler-Eckhoff A, Demes M. Neuroendocrine tumors of the lung. Cancers (Basel). 2012; 4:777–98.
Article8. Ferry AP, Font RL. Carcinoma metastatic to the eye and orbit. I. A clinicopathologic study of 227 cases. Arch Ophthalmol. 1974; 92:276–86.9. Atik A, Krilis M, Shannon K. Small cell neuroendocrine abdominal masquerading as cellulitis and causing blindness via bilateral orbital involvement. Orbit. 2013; 32:197–9.10. Sira M, Clauss RP, Maclean C, Rose GE. Orbital metastases from neuroendocrine carcinoma, masquerading as graves orbitopathy. Orbit. 2010; 29:94–6.
Article11. Remick SC, Hafez GR, Carbone PP. Extrapulmonary small-cell carcinoma. A review of the literature with emphasis on therapy and outcome. Medicine (Baltimore). 1987; 66:457–71.12. Velten IM, Gusek-Schneider GC, Tomandl B. Diplopia as first symptom of a bronchogenic carcinoma. Klin Monbl Augenheikd. 2000; 217:52–4.13. Yeh S, Foroozan R. Orbital apex syndrome. Curr Opin Ophthalmol. 2004; 15:490–8.
Article14. Goldberg RA, Rootman J. Clinical characteristics of metastatic abdominalal tumors. Ophthalmology. 1990; 97:620–4.15. Huang YY, Chang A, Chou YY, Hsu WC. Metastatic abdominal tumor with initial presentation of orbital apex syndrome. Interdiscip Neurosurg. 2017; 7:9–11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Small Cell Neuroendocrine Carcinoma in the Parotid and Lacrimal Glands
- Small-cell neuroendocrine carcinoma of the breast
- A Case of Metastatic Small Cell Neuroendocrine Carcinoma of the Lung Mimicking a Merkel Cell Carcinoma
- Two Cases of Neuroendocrine Carcinomas of the Stomach: Large Cell Carcinoma and Small Cell Carcinoma
- Skin Metastasis of Neuroendocrine Carcinoma Arising in the Rectum