Anesth Pain Med.
2019 Oct;14(4):434-440. 10.17085/apm.2019.14.4.434.
Postoperative emergence agitation and intraoperative sevoflurane sedation under caudal block in children: a randomized comparison of two sevoflurane doses
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Yeungnam University College of Medicine, Daegu, Korea.
- 2Department of Anesthesiology and Pain Medicine, Dongsan Hospital, Keimyung University School of Medicine, Daegu, Korea.
- 3Department of Anesthesiology and Pain Medicine, School of Medicine, Kyungpook National University, Daegu, Korea. sspark@knu.ac.kr
- KMID: 2465342
- DOI: http://doi.org/10.17085/apm.2019.14.4.434
Abstract
- BACKGROUND
Sub-umbilical surgery under caudal block in conjunction with sevoflurane sedation may be safe in terms of maintaining spontaneous breathing and avoiding complications associated with general anesthesia. However, sevoflurane-induced emergence agitation (EA) continues to be a clinically important phenomenon in children. To compare the incidence of EA in children undergoing sub-umbilical surgery under caudal block with two different doses of sevoflurane.
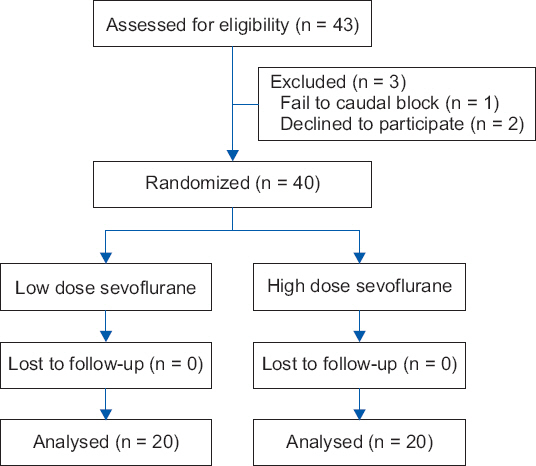
METHODS
Forty children (aged 1-5 years) scheduled to undergo inguinal hernia repair under caudal block with sevoflurane sedation via a face mask were randomized into either the low-dose (1.0%) end-tidal sevoflurane concentration group (Group LS) or the high-dose (2.5%) end-tidal sevoflurane concentration group (Group HS). We monitored EA episodes at 5 and 30 min in the post-anesthetic care unit (PACU) by using the four-point agitation scale and the Pediatric Anesthesia Emergence Delirium (PAED) scale.
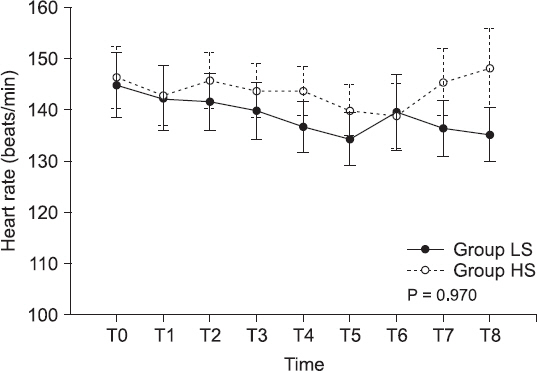
RESULTS
The four-point agitation scale scores and PAED scores were not different between the groups at 5 min. However, the agitation score was higher in Group HS than in Group LS at 30 min after arriving in the PACU. The time required to recover from sedation was longer in Group HS than in Group LS.
CONCLUSIONS
Face-mask sedation with 1.0% sevoflurane in conjunction with caudal block may be more effective than that with 2.5% sevoflurane in preventing EA.
Keyword
MeSH Terms
Figure
Reference
-
1. Veyckemans F, Van Obbergh LJ, Gouverneur JM. Lessons from 1100 pediatric caudal blocks in a teaching hospital. Reg Anesth. 1992; 17:119–25. PMID: 1606093.2. Bong CL, Yeo AS, Fabila T, Tan JS. A pilot study of dexmedetomidine sedation and caudal anesthesia for inguinal hernia repair in infants. Paediatr Anaesth. 2016; 26:621–7. DOI: 10.1111/pan.12907. PMID: 27061946.3. Balent E, Edwards M, Lustik M, Martin P. Caudal anesthesia with sedation for inguinal hernia repair in high risk neonates. J Pediatr Surg. 2014; 49:1304–7. DOI: 10.1016/j.jpedsurg.2013.11.005. PMID: 25092095.4. Choi EK, Ro Y, Park SS, Park KB. The use of EMLA cream reduces the pain of skin puncture associated with caudal block in children. Korean J Anesthesiol. 2016; 69:149–54. DOI: 10.4097/kjae.2016.69.2.149. PMID: 27066206. PMCID: PMC4823410.5. Gunter J. Caudal anesthesia in children:a survey. Anesthesiology. 1991; 75:936. DOI: 10.1097/00000542-199109001-00935.6. Sikich N, Lerman J. Development and psychometric evaluation of the pediatric anesthesia emergence delirium scale. Anesthesiology. 2004; 100:1138–45. DOI: 10.1097/00000542-200405000-00015. PMID: 15114210.7. Voepel-Lewis T, Malviya S, Tait AR. A prospective cohort study of emergence agitation in the pediatric postanesthesia care unit. Anesth Analg. 2003; 96:1625–30. DOI: 10.1213/01.ANE.0000062522.21048.61. PMID: 12760985.8. Finkel JC, Cohen IT, Hannallah RS, Patel KM, Kim MS, Hummer KA, et al. The effect of intranasal fentanyl on the emergence characteristics after sevoflurane anesthesia in children undergoing surgery for bilateral myringotomy tube placement. Anesth Analg. 2001; 92:1164–8. DOI: 10.1097/00000539-200105000-00016. PMID: 11323340.9. Son JS, Jang E, Oh MW, Lee JH, Han YJ, Ko S. Erratum:a comparison of postoperative emergence agitation between sevoflurane and thiopental anesthesia induction in pediatric patients. Korean J Anesthesiol. 2016; 69:100. Erratum for: Korean J Anesthesiol 2015;68: 3738. DOI: 10.4097/kjae.2016.69.1.100. PMID: 26885313. PMCID: PMC4754259.10. Giaufré E, Dalens B, Gombert A. Epidemiology and morbidity of regional anesthesia in children:a one-year prospective survey of the French-Language Society of Pediatric Anesthesiologists. Anesth Analg. 1996; 83:904–12. DOI: 10.1097/00000539-199611000-00003. PMID: 8895261.11. Combes X, Schauvliege F, Peyrouset O, Motamed C, Kirov K, Dhonneur G, et al. Intracuff pressure and tracheal morbidity:influence of filling with saline during nitrous oxide anesthesia. Anesthesiology. 2001; 95:1120–4. DOI: 10.1097/00000542-200111000-00015. PMID: 11684980.12. Christensen AM, Willemoes-Larsen H, Lundby L, Jakobsen KB. Postoperative throat complaints after tracheal intubation. Br J Anaesth. 1994; 73:786–7. DOI: 10.1093/bja/73.6.786. PMID: 7880666.13. Sims C, Johnson CM. Postoperative apnoea in infants. Anaesth Intensive Care. 1994; 22:40–5. DOI: 10.1177/0310057X9402200108. PMID: 8160948.14. Kim SH, Chun DH, Chang CH, Kim TW, Kim YM, Shin YS. Effect of caudal block on sevoflurane requirement for lower limb surgery in children with cerebral palsy. Paediatr Anaesth. 2011; 21:394–8. DOI: 10.1111/j.1460-9592.2011.03530.x. PMID: 21299684.15. Weldon BC, Bell M, Craddock T. The effect of caudal analgesia on emergence agitation in children after sevoflurane versus halothane anesthesia. Anesth Analg. 2004; 98:321–6. DOI: 10.1213/01.ANE.0000096004.96603.08. PMID: 14742362.16. Mallory MD, Baxter AL, Kost SI. Pediatric Sedation Research Consortium. Propofol vs pentobarbital for sedation of children undergoing magnetic resonance imaging:results from the Pediatric Sedation Research Consortium. Paediatr Anaesth. 2009; 19:601–11. DOI: 10.1111/j.1460-9592.2009.03023.x. PMID: 19645979.17. Lerman J, Davis PJ, Welborn LG, Orr RJ, Rabb M, Carpenter R, et al. Induction, recovery, and safety characteristics of sevoflurane in children undergoing ambulatory surgery A comparison with halothane. Anesthesiology. 1996; 84:1332–40. DOI: 10.1097/00000542-199606000-00009. PMID: 8669674.18. Aono J, Ueda W, Mamiya K, Takimoto E, Manabe M. Greater incidence of delirium during recovery from sevoflurane anesthesia in preschool boys. Anesthesiology. 1997; 87:1298–300. DOI: 10.1097/00000542-199712000-00006. PMID: 9416712.19. Cravero J, Surgenor S, Whalen K. Emergence agitation in paediatric patients after sevoflurane anaesthesia and no surgery:a comparison with halothane. Paediatr Anaesth. 2000; 10:419–24. DOI: 10.1046/j.1460-9592.2000.00560.x. PMID: 10886700.20. Bortone L, Bertolizio G, Engelhardt T, Frawley G, Somaini M, Ingelmo PM. The effect of fentanyl and clonidine on early postoperative negative behavior in children:a double-blind placebo controlled trial. Paediatr Anaesth. 2014; 24:614–9. DOI: 10.1111/pan.12388. PMID: 24666767.21. Cho EJ, Yoon SZ, Cho JE, Lee HW. Comparison of the effects of 0.03 and 0.05 mg/kg midazolam with placebo on prevention of emergence agitation in children having strabismus surgery. Anesthesiology. 2014; 120:1354–61. DOI: 10.1097/ALN.0000000000000181. PMID: 24566243.22. Abu-Shahwan I, Chowdary K. Ketamine is effective in decreasing the incidence of emergence agitation in children undergoing dental repair under sevoflurane general anesthesia. Paediatr Anaesth. 2007; 17:846–50. DOI: 10.1111/j.1460-9592.2007.02298.x. PMID: 17683402.23. Kern D, Fourcade O, Mazoit JX, Minville V, Chassery C, Chausseray G, et al. The relationship between bispectral index and endtidal concentration of sevoflurane during anesthesia and recovery in spontaneously ventilating children. Paediatr Anaesth. 2007; 17:249–54. DOI: 10.1111/j.1460-9592.2006.02083.x. PMID: 17263740.24. Kim KM, Lee KH, Kim YH, Ko MJ, Jung JW, Kang E. Comparison of effects of intravenous midazolam and ketamine on emergence agitation in children:randomized controlled trial. J Int Med Res. 2016; 44:258–66. DOI: 10.1177/0300060515621639. PMID: 26880794. PMCID: PMC5580063.25. Ko YP, Huang CJ, Hung YC, Su NY, Tsai PS, Chen CC, et al. Premedication with low-dose oral midazolam reduces the incidence and severity of emergence agitation in pediatric patients following sevoflurane anesthesia. Acta Anaesthesiol Sin. 2001; 39:169–77. PMID: 11840583.26. Breschan C, Platzer M, Jost R, Stettner H, Likar R. Midazolam does not reduce emergence delirium after sevoflurane anesthesia in children. Paediatr Anaesth. 2007; 17:347–52. DOI: 10.1111/j.1460-9592.2006.02101.x. PMID: 17359403.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Effects of Caudal Block on Emergence Agitation after Sevoflurane Anesthesia in Herniorrhaphy Pediatric Patients
- The Comparative Effects of Caudal Block and IV Ketorolac on Emergence Delirium after Sevoflurane Anesthesia in Children
- Effect of Dexmedetomidine on Sevoflurane Requirements and Emergence Agitation in Children Undergoing Ambulatory Surgery
- The Effect of Combined Use of Remifentanil on Postoperative Recovery Time and Emergence Agitation during Sevoflurane Anesthesia in Children
- Effects of propofol and nalbuphine on emergence agitation after sevoflurane anesthesia in children for strabismus surgery