Hip Pelvis.
2019 Dec;31(4):206-215. 10.5371/hp.2019.31.4.206.
Cementless Bipolar Hemiarthroplasty for Low-energy Intracapsular Proximal Femoral Fracture in Elderly East-Asian Patients: A Longitudinal 10-year Follow-up Study
- Affiliations
-
- 1Department of Orthopaedic Surgery, Ohta-Nishinouchi Hospital, Fukushima, Japan. ichiro.okano.e31@gmail.com
- 2Department of Orthopaedic Surgery, Showa University School of Medicine, Tokyo, Japan.
- KMID: 2464237
- DOI: http://doi.org/10.5371/hp.2019.31.4.206
Abstract
- PURPOSE
Short-term outcomes following cemented and cementless hemiarthroplasties (HAs) are reported to be comparable, however, long-term outcomes of cementless HA"”especially among Asian patients"”is limited. We aimed to assess long-term outcomes in elderly East-Asian patients with intracapsular proximal femoral fractures treated with cementless HA.
MATERIALS AND METHODS
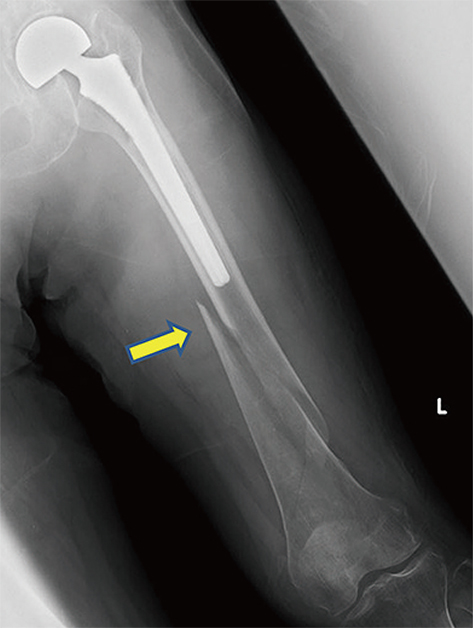
We enrolled 135 patients treated with cementless HA who met our inclusion criteria. We documented bone/implant-related complications (e.g., incidences of revision hip surgery, femoral stem subsidence, dislocation, intraoperative and postoperative periprosthetic fractures, contralateral hip fractures). We included those patients who are still alive 10 years after the index surgery in the final functional analysis of the existence of pain, ambulatory status, and residential status.
RESULTS
The mean age at injury was 78.3 years (range: 60-85 years). At the 10-year follow-up, 26 of the original patients (19.3%) had survived. During follow-up, revision hip surgery was conducted in two patients (1.5%). We recorded the incidence of intraoperative fractures, postoperative periprosthetic fractures, and contralateral fractures in two (1.5%), eight (5.9%), and six patients (4.4%), respectively. Among the 10-year survivors, six patients (23.1% of the survivors) complained of groin pain, but generally reported the pain to be tolerable.
CONCLUSION
Among elderly East-Asian patients, the incidence of revision surgery after cementless HA may be lower than that in their European counterparts, whereas the incidence of periprosthetic fractures can still be considerably higher. For patients undergoing cementless HA, prevention of such secondary fractures is of critical importance.
Keyword
MeSH Terms
Figure
Reference
-
1. Alexiou KI, Roushias A, Varitimidis SE, Malizos KN. Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging. 2018; 13:143–150.
Article2. Schrøder HM, Erlandsen M. Age and sex as determinants of mortality after hip fracture: 3,895 patients followed for 2.5-18.5 years. J Orthop Trauma. 1993; 7:525–531.
Article3. Zhang BF, Wang PF, Huang H, Cong YX, Wang H, Zhuang Y. Interventions for treating displaced intracapsular femoral neck fractures in the elderly: a Bayesian network meta-analysis of randomized controlled trials. Sci Rep. 2017; 7:13103.
Article4. Mittal R, Banerjee S. Proximal femoral fractures: principles of management and review of literature. J Clin Orthop Trauma. 2012; 3:15–23.
Article5. Manoharan G, Chatterton BD, Moores TS, Roberts PJ. Uncemented Thompson's hemiarthroplasty: safe, palliative and cost-effective surgery in the infirm patient-a consecutive series of 1445 cases. Eur J Orthop Surg Traumatol. 2018; 28:1103–1109.
Article6. Yli-Kyyny T, Sund R, Heinänen M, Venesmaa P, Kröger H. Cemented or uncemented hemiarthroplasty for the treatment of femoral neck fractures? Acta Orthop. 2014; 85:49–53.
Article7. Bell KR, Clement ND, Jenkins PJ, Keating JF. A comparison of the use of uncemented hydroxyapatite-coated bipolar and cemented femoral stems in the treatment of femoral neck fractures: a case-control study. Bone Joint J. 2014; 96:299–305.8. Deangelis JP, Ademi A, Staff I, Lewis CG. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: a prospective randomized trial with early follow-up. J Orthop Trauma. 2012; 26:135–140.
Article9. Ng ZD, Krishna L. Cemented versus cementless hemiarthroplasty for femoral neck fractures in the elderly. J Orthop Surg (Hong Kong). 2014; 22:186–189.
Article10. Shewale SB, Pandit HG, Latham JM. Hemiarthroplasty: to cement or not to cement? A preliminary report. Hip Int. 2004; 14:189–192.
Article11. Parker MI, Pryor G, Gurusamy K. Cemented versus uncemented hemiarthroplasty for intracapsular hip fractures: a randomised controlled trial in 400 patients. J Bone Joint Surg Br. 2010; 92:116–122.12. Moerman S, Mathijssen NMC, Niesten DD, et al. More complications in uncemented compared to cemented hemiarthroplasty for displaced femoral neck fractures: a randomized controlled trial of 201 patients, with one year follow-up. BMC Musculoskelet Disord. 2017; 18:169.
Article13. Langslet E, Frihagen F, Opland V, Madsen JE, Nordsletten L, Figved W. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: 5-year followup of a randomized trial. Clin Orthop Relat Res. 2014; 472:1291–1299.
Article14. Wagner P, Fuentes P, Diaz A, et al. Comparison of complications and length of hospital stay between orthopedic and orthogeriatric treatment in elderly patients with a hip fracture. Geriatr Orthop Surg Rehabil. 2012; 3:55–58.
Article15. Lin JC, Liang WM. Outcomes after fixation for undisplaced femoral neck fracture compared to hemiarthroplasty for displaced femoral neck fracture among the elderly. BMC Musculoskelet Disord. 2015; 16:199.
Article16. van den Bekerom MP, Hilverdink EF, Sierevelt IN, et al. A comparison of hemiarthroplasty with total hip replacement for displaced intracapsular fracture of the femoral neck: a randomised controlled multicentre trial in patients aged 70 years and over. J Bone Joint Surg Br. 2010; 92:1422–1428.17. Figved W, Opland V, Frihagen F, Jervidalo T, Madsen JE, Nordsletten L. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures. Clin Orthop Relat Res. 2009; 467:2426–2435.
Article18. de Jong L, Klem TMAL, Kuijper TM, Roukema GR. Factors affecting the rate of surgical site infection in patients after hemiarthroplasty of the hip following a fracture of the neck of the femur. Bone Joint J. 2017; 99:1088–1094.
Article19. Khan RJ, MacDowell A, Crossman P, Keene GS. Cemented or uncemented hemiarthroplasty for displaced intracapsular fractures of the hip--a systematic review. Injury. 2002; 33:13–17.
Article20. Ning GZ, Li YL, Wu Q, Feng SQ, Li Y, Wu QL. Cemented versus uncemented hemiarthroplasty for displaced femoral neck fractures: an updated meta-analysis. Eur J Orthop Surg Traumatol. 2014; 24:7–14.
Article21. Donaldson AJ, Thomson HE, Harper NJ, Kenny NW. Bone cement implantation syndrome. Br J Anaesth. 2009; 102:12–22.
Article22. Isotalo K, Rantanen J, Aärimaa V, Gullichsen E. The long-term results of Lubinus interplanta hemiarthroplasty in 228 acute femoral neck fractures. A retrospective six-year follow-up. Scand J Surg. 2002; 91:357–360.
Article23. Tol MC, van den Bekerom MP, Sierevelt IN, Hilverdink EF, Raaymakers EL, Goslings JC. Hemiarthroplasty or total hip arthroplasty for the treatment of a displaced intracapsular fracture in active elderly patients: 12-year follow-up of randomised trial. Bone Joint J. 2017; 99:250–254.24. von Roth P, Abdel MP, Harmsen WS, Berry DJ. Cemented bipolar hemiarthroplasty provides definitive treatment for femoral neck fractures at 20 years and beyond. Clin Orthop Relat Res. 2015; 473:3595–3599.
Article25. Moore AT. The self-locking metal hip prosthesis. J Bone Joint Surg Am. 1957; 39:811–827.
Article26. Kabelitz M, Fritz Y, Grueninger P, Meier C, Fries P, Dietrich M. Cementless stem for femoral neck fractures in a patient's 10th decade of life: high rate of periprosthetic fractures. Geriatr Orthop Surg Rehabil. 2018; 9:2151459318765381.
Article27. Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013; 48:452–458.
Article28. Khanuja HS, Vakil JJ, Goddard MS, Mont MA. Cementless femoral fixation in total hip arthroplasty. J Bone Joint Surg Am. 2011; 93:500–509.
Article29. Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994; 9:33–44.
Article30. Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995; 44:293–304.31. Chatterton BD, Moores TS, Ahmad S, Cattell A, Roberts PJ. Cause of death and factors associated with early in-hospital mortality after hip fracture. Bone Joint J. 2015; 97:246–251.
Article32. Viberg B, Overgaard S, Lauritsen J, Ovesen O. Lower reoperation rate for cemented hemiarthroplasty than for uncemented hemiarthroplasty and internal fixation following femoral neck fracture: 12- to 19-year follow-up of patients aged 75 years or more. Acta Orthop. 2013; 84:254–259.
Article33. Wagner ER, Kamath AF, Fruth KM, Harmsen WS, Berry DJ. Effect of body mass index on complications and reoperations after total hip arthroplasty. J Bone Joint Surg Am. 2016; 98:169–179.
Article34. Traina F, Bordini B, De Fine M, Toni A. Patient weight more than body mass index influences total hip arthroplasty long term survival. Hip Int. 2011; 21:694–699.
Article35. Hoaglund FT. Primary osteoarthritis of the hip: a genetic disease caused by European genetic variants. J Bone Joint Surg Am. 2013; 95:463–468.
Article36. Steinberg ME, Corces A, Fallon M. Acetabular involvement in osteonecrosis of the femoral head. J Bone Joint Surg Am. 1999; 81:60–65.
Article37. Hwang KT, Kim YH, Kim YS, Choi IY. Is bipolar hemiarthroplasty a reliable option for Ficat stage III osteonecrosis of the femoral head? 15- to 24-year follow-up study. Arch Orthop Trauma Surg. 2012; 132:1789–1796.
Article38. Muraki M, Sudo A, Hasegawa M, Fukuda A, Uchida A. Long-term results of bipolar hemiarthroplasty for osteoarthritis of the hip and idiopathic osteonecrosis of the femoral head. J Orthop Sci. 2008; 13:313–317.
Article39. Gallinaro P, Tabasso G, Negretto R, Brach del Prever EM. Experience with bipolar prosthesis in femoral neck fractures in the elderly and debilitated. Clin Orthop Relat Res. 1990; (251):26–30.
Article40. Foster AP, Thompson NW, Wong J, Charlwood AP. Periprosthetic femoral fractures--a comparison between cemented and uncemented hemiarthroplasties. Injury. 2005; 36:424–429.
Article41. Chana R, Mansouri R, Jack C, et al. The suitability of an uncemented hydroxyapatite coated (HAC) hip hemiarthroplasty stem for intra-capsular femoral neck fractures in osteoporotic elderly patients: the Metaphyseal-Diaphyseal Index, a solution to preventing intra-operative periprosthetic fracture. J Orthop Surg Res. 2011; 6:59.
Article42. Robinson CM, Adams CI, Craig M, Doward W, Clarke MC, Auld J. Implant-related fractures of the femur following hip fracture surgery. J Bone Joint Surg Am. 2002; 84:1116–1122.
Article43. Hagino H, Sawaguchi T, Endo N, Ito Y, Nakano T, Watanabe Y. The risk of a second hip fracture in patients after their first hip fracture. Calcif Tissue Int. 2012; 90:14–21.
Article44. Yamanashi A, Yamazaki K, Kanamori M, et al. Assessment of risk factors for second hip fractures in Japanese elderly. Osteoporos Int. 2005; 16:1239–1246.
Article45. Vochteloo AJ, Borger van der Burg BL, Röling MA, et al. Contralateral hip fractures and other osteoporosis-related fractures in hip fracture patients: incidence and risk factors. An observational cohort study of 1,229 patients. Arch Orthop Trauma Surg. 2012; 132:1191–1197.
Article46. Mitani S, Shimizu M, Abo M, Hagino H, Kurozawa Y. Risk factors for second hip fractures among elderly patients. J Orthop Sci. 2010; 15:192–197.
Article47. Chang JD, Yoo JH, Reddy P, Lee SS, Hwang JH, Kim TY. Risk factors for contra-lateral hip fracture in elderly patients with previous hip fracture. Injury. 2013; 44:1930–1933.
Article48. Batin S, Ozan F, Gurbuz K, Koyuncu S, Vatansever F, Uzun E. Evaluation of risk factors for second hip fractures in elderly patients. J Clin Med Res. 2018; 10:217–220.
Article49. Zhang J, Ang ML, Kwek EB. Who will walk again? Effects of rehabilitation on the ambulatory status in elderly patients undergoing hemiarthroplasty for femoral neck fracture. Geriatr Orthop Surg Rehabil. 2015; 6:168–172.
Article50. Knechel NA. The challenges of enrolling older adults into intervention studies. Yale J Biol Med. 2013; 86:41–47.51. Ridda I, MacIntyre CR, Lindley RI, Tan TC. Difficulties in recruiting older people in clinical trials: an examination of barriers and solutions. Vaccine. 2010; 28:901–906.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Bipolar Hemiarthroplasty with Cementless Femoral Stem for Unstable Intertrochanteric Fractures
- Cementless Bipolar Hemiarthroplasty for Hip Fracture in Patients More than Seventy Years Old with Osteoporosis
- Cementless Bipolar Hemiarthroplasty for Femoral Neck Fractures in Elderly Patients
- Cementless Hemiarthroplasty for Intracapsular Femoral Neck Fractures in the Octa- and Nonagenarians
- Cementless Bipolar Hemiarthroplasty for the Management of Fracture of the Femoral Neck