J Korean Neurosurg Soc.
2019 Nov;62(6):643-648. 10.3340/jkns.2018.0152.
Risk Factors and Preoperative Risk Scoring System for Shunt-Dependent Hydrocephalus Following Aneurysmal Subarachnoid Hemorrhage
- Affiliations
-
- 1Department of Neurosurgery, Eulji University Eulji Hospital, Seoul, South Korea. grimi2@eulji.ac.kr
- KMID: 2463656
- DOI: http://doi.org/10.3340/jkns.2018.0152
Abstract
OBJECTIVE
Shunt-dependent hydrocephalus (SdHCP) is a well-known complication of aneurysmal subarachnoid hemorrhage (SAH). The risk factors for SdHCP have been widely investigated, but few risk scoring systems have been established to predict SdHCP. This study was performed to investigate the risk factors for SdHCP and devise a risk scoring system for use before aneurysm obliteration.
METHODS
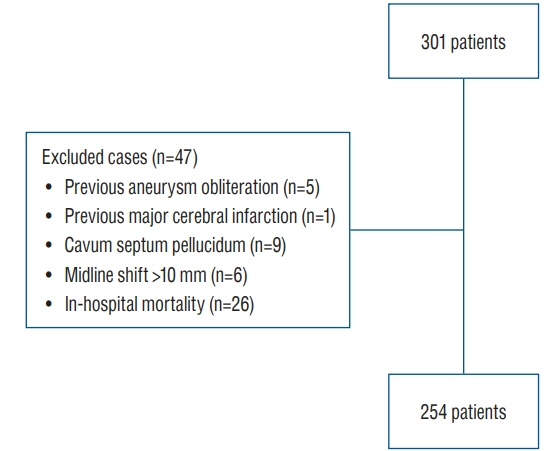
We reviewed the data of 301 consecutive patients who underwent aneurysm obliteration following SAH from September 2007 to December 2016. The exclusion criteria for this study were previous aneurysm obliteration, previous major cerebral infarction, the presence of a cavum septum pellucidum, a midline shift of >10 mm on initial computed tomography (CT), and in-hospital mortality. We finally recruited 254 patients and analyzed the following data according to the presence or absence of SdHCP : age, sex, history of hypertension and diabetes mellitus, Hunt-Hess grade, Fisher grade, aneurysm size and location, type of treatment, bicaudate index on initial CT, intraventricular hemorrhage, cerebrospinal fluid drainage, vasospasm, and modified Rankin scale score at discharge.
RESULTS
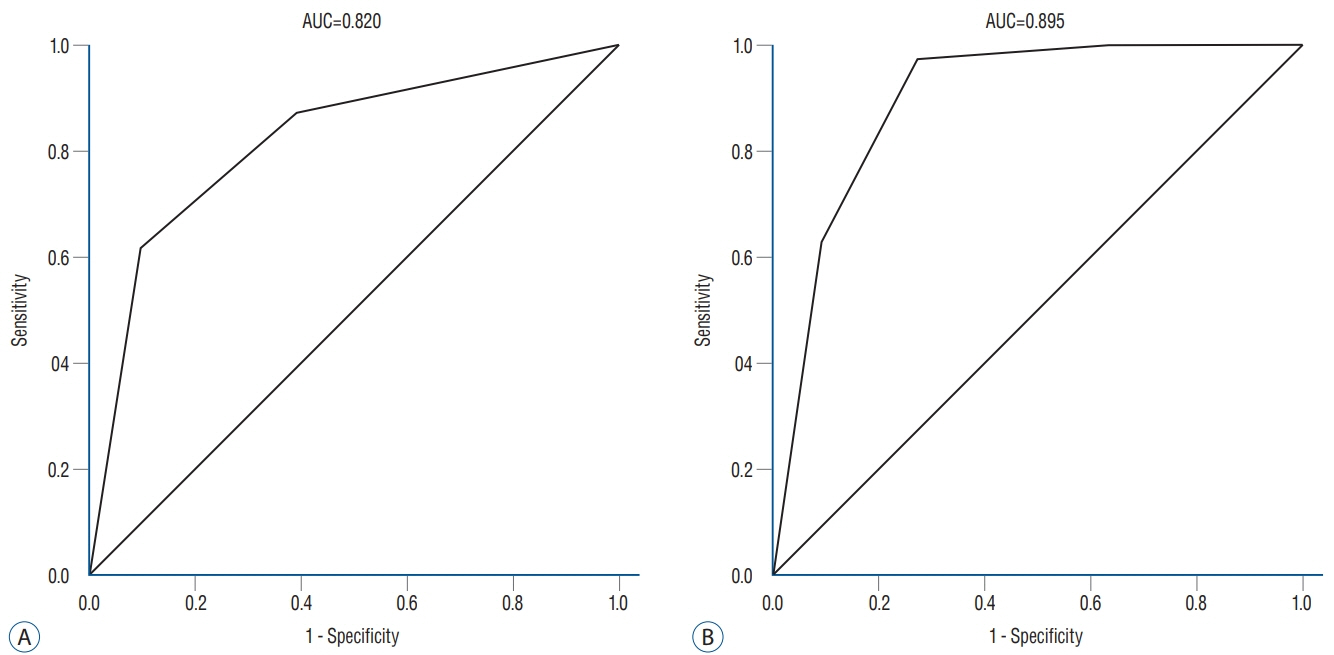
In the multivariate analysis, acute HCP (bicaudate index of ≥0.2) (odds ratio [OR], 6.749; 95% confidence interval [CI], 2.843-16.021; p=0.000), Fisher grade of 4 (OR, 4.108; 95% CI, 1.044-16.169; p=0.043), and an age of ≥50 years (OR, 3.938; 95% CI, 1.375-11.275; p=0.011) were significantly associated with the occurrence of SdHCP. The risk scoring system using above parameters of acute HCP, Fisher grade, and age (AFA score) assigned 1 point to each (total score of 0-3 points). SdHCP occurred in 4.3% of patients with a score of 0, 8.5% with a score of 1, 25.5% with a score of 2, and 61.7% with a score of 3 (p=0.000). In the receiver operating characteristic curve analysis, the area under the curve (AUC) for the risk scoring system was 0.820 (p=0.080; 95% CI, 0.750-0.890). In the internal validation of the risk scoring system, the score reliably predicted SdHCP (AUC, 0.895; p=0.000; 95% CI, 0.847-0.943).
CONCLUSION
Our results suggest that the herein-described AFA score is a useful tool for predicting SdHCP before aneurysm obliteration. Prospective validation is needed.
MeSH Terms
Figure
Reference
-
References
1. Adams H, Ban VS, Leinonen V, Aoun SG, Huttunen J, Saavalainen T, et al. Risk of shunting after aneurysmal subarachnoid hemorrhage: a collaborative study and initiation of a consortium. Stroke. 47:2488–2496. 2016.
Article2. Bae IS, Yi HJ, Choi KS, Chun HJ. Comparison of incidence and risk factors for shunt-dependent hydrocephalus in aneurysmal subarachnoid hemorrhage patients. J Cerebrovasc Endovasc Neurosurg. 16:78–84. 2014.
Article3. Chan M, Alaraj A, Calderon M, Herrera SR, Gao W, Ruland S, et al. Prediction of ventriculoperitoneal shunt dependency in patients with aneurysmal subarachnoid hemorrhage. J Neurosurg. 110:44–49. 2009.
Article4. Diesing D, Wolf S, Sommerfeld J, Sarrafzadeh A, Vajkoczy P, Dengler NF. A novel score to predict shunt dependency after aneurysmal subarachnoid hemorrhage. J Neurosurg. 128:1273–1279. 2018.
Article5. Dorai Z, Hynan LS, Kopitnik TA, Samson D. Factors related to hydrocephalus after aneurysmal subarachnoid hemorrhage. Neurosurgery. 52:763–769. discussion 769-771. 2003.
Article6. Dupont S, Rabinstein AA. CT evaluation of lateral ventricular dilatation after subarachnoid hemorrhage: baseline bicaudate index values [correction of balues]. Neurol Res. 35:103–106. 2013.
Article7. Dupont S, Rabinstein AA. Extent of acute hydrocephalus after subarachnoid hemorrhage as a risk factor for poor functional outcome. Neurol Res. 35:107–110. 2013.
Article8. Gao F, Liu F, Chen Z, Hua Y, Keep RF, Xi G. Hydrocephalus after intraventricular hemorrhage: the role of thrombin. J Cereb Blood Flow Metab. 34:489–494. 2014.
Article9. Jabbarli R, Bohrer AM, Pierscianek D, Müller D, Wrede KH, Dammann P, et al. The CHESS score: a simple tool for early prediction of shunt dependency after aneurysmal subarachnoid hemorrhage. Eur J Neurol. 23:912–918. 2016.
Article10. Johanson CE, Duncan JA 3rd, Klinge PM, Brinker T, Stopa EG, Silverberg GD. Multiplicity of cerebrospinal fluid functions: new challenges in health and disease. Cerebrospinal Fluid Res. 5:10. 2008.
Article11. Li T, Zhang P, Yuan B, Zhao D, Chen Y, Zhang X. Thrombin-induced TGF-β1 pathway: a cause of communicating hydrocephalus post subarachnoid hemorrhage. Int J Mol Med. 31:660–666. 2013.
Article12. Motiei-Langroudi R, Adeeb N, Foreman PM, Harrigan MR, Fisher WS Rd, Vyas NA, et al. Predictors of shunt insertion in aneurysmal subarachnoid hemorrhage. World Neurosurg. 98:421–426. 2017.
Article13. Nam KH, Hamm IS, Kang DH, Park J, Kim YS. Risk of shunt dependent hydrocephalus after treatment of ruptured intracranial aneurysms : surgical clipping versus endovascular coiling according to Fisher grading system. J Korean Neurosurg Soc. 48:313–318. 2010.
Article14. Pinggera D, Kerschbaumer J, Petr O, Ortler M, Thomé C, Freyschlag CF. The volume of the third ventricle as a prognostic marker for shunt dependency after aneurysmal subarachnoid hemorrhage. World Neurosurg. 108:107–111. 2017.
Article15. Rincon F, Gordon E, Starke RM, Buitrago MM, Fernandez A, Schmidt JM, et al. Predictors of long-term shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage. Clinical article. J Neurosurg. 113:774–780. 2010.
Article16. Sakka L, Coll G, Chazal J. Anatomy and physiology of cerebrospinal fluid. Eur Ann Otorhinolaryngol Head Neck Dis. 128:309–316. 2011.
Article17. Tso MK, Ibrahim GM, Macdonald RL. Predictors of shunt-dependent hydrocephalus following aneurysmal subarachnoid hemorrhage. World Neurosurg. 86:226–232. 2016.
Article18. Wilson CD, Safavi-Abbasi S, Sun H, Kalani MY, Zhao YD, Levitt MR, et al. Meta-analysis and systematic review of risk factors for shunt dependency after aneurysmal subarachnoid hemorrhage. J Neurosurg. 126:586–595. 2017.
Article19. Wilson DA, Nakaji P, Abla AA, Uschold TD, Fusco DJ, Oppenlander ME, et al. A simple and quantitative method to predict symptomatic vasospasm after subarachnoid hemorrhage based on computed tomography: beyond the Fisher scale. Neurosurgery. 71:869–875. 2012.
Article20. Woernle CM, Winkler KM, Burkhardt JK, Haile SR, Bellut D, Neidert MC, et al. Hydrocephalus in 389 patients with aneurysm-associated subarachnoid hemorrhage. J Clin Neurosci. 20:824–826. 2013.
Article21. Xie Z, Hu X, Zan X, Lin S, Li H, You C. Predictors of shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage? A systematic review and meta-analysis. World Neurosurg. 106:844–860. e6. 2017.
Article22. Yamada S, Nakase H, Park YS, Nishimura F, Nakagawa I. Discriminant analysis prediction of the need for ventriculoperitoneal shunt after subarachnoid hemorrhage. J Stroke Cerebrovasc Dis. 21:493–497. 2012.
Article23. Zaidi HA, Montoure A, Elhadi A, Nakaji P, McDougall CG, Albuquerque FC, et al. Long-term functional outcomes and predictors of shuntdependent hydrocephalus after treatment of ruptured intracranial aneurysms in the BRAT trial: revisiting the clip vs coil debate. Neurosurgery. 76:608–613. discussion 613-614; quiz 614. 2015.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Study on Risk Factors of Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage
- Factors Related to Shunt-Dependent Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage
- Risk Factors for Development of Chronic Hydrocephalus Following Aneurysmal Subarachnoidal Hemorrhage
- Clinical Analysis of Risk Factors in Shunt-dependent Hydrocephalus after Aneurysmal Subarachnoid Hemorrhage
- Analysis of the Effect of Initial External Ventricular Drainage in Patients with Aneurysmal Subarachnoid Hemorrhage on the Late Onset of Hydrocephalus